Chapter Outline
Tendon Disease
De Quervain’s Disease
De Quervain’s disease is an overuse tenosynovitis of the abductor pollicis longus and extensor pollicis brevis tendons in the first extensor compartment (EC). Low-grade chronic microtrauma is thought to underlie the condition, leading to localized thickening of the extensor retinaculum at the level of the radial styloid. This results in narrowing of the first extensor compartment with impingement and subsequent inflammation of the abductor pollicis longus and extensor pollicis brevis tendons. De Quervain’s is most common in the 30–50 year age group in patients who perform repetitive thumb movements, such as pianists and typists. Baby wrist affects new mothers as a result of repeated wrist flexion and extension with abduction of the thumb against resistance that occurs while holding the baby’s head. Patients present with pain around the radial styloid with thumb movement, which typically increases while grasping heavy objects.
Scanning in the transverse plane gives a good view of the extensor retinaculum, tendon sheath contents and presence of internal septa. A thick layer of gel may help image the contours of the wrist and avoid excessive transducer pressure, which can displace the synovial fluid.
The abductor pollicis longus and extensor pollicis brevis tendons are typically swollen and hypoechoic owing to oedematous change. They may be difficult to distinguish from one another as they become compressed in the confined space of the osteofibrous tunnel. The extensor retinaculum which is identified over the radial styloid can be thickened and hypoechoic, which may be an indication for release. Fluid and synovial thickening distend the tendon sheath, which is best seen surrounding the tendons distal to the retinaculum ( Figs 11.1 and 11.2 ). Dynamic scanning shows irregular tendon gliding beneath the retinaculum during thumb extension.
| Care should be taken not to confuse the extensor retinaculum, which is noncompressible and located at the level of the radial styloid, with fluid within the tendon sheath, which is compressible and best seen distal to the radius. |


Although de Quervain’s tenosynovitis can be associated with excess fluid within the sheath, some, if not many, patients present with a more sclerosing type, with less peritendinous fluid and more tenosynovial thickening. Thickening of the retinaculum dominates the ultrasound picture.
Thickening of the retinaculum of extensor compartment 1 should be sought in all patients presenting with radial side pain.

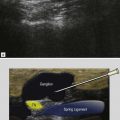
A vertical septum splitting the first extensor compartment into two subtunnels for each of the tendons is encountered more frequently in patients with de Quervain’s disease and is thought to predispose to local tendon friction. Accessory vertical septa appear as thin hypoechoic linear bands between the tendons ( Fig. 11.3 ). The inflammatory process may selectively involve one tendon when a septum is present. Identification of a septum is clinically significant as it forms a barrier to diffusion of injected steroids and requires decompression of both tunnels at surgery. A septum splitting the first extensor compartment and more sclerosing tenosynovitis may be indicative of a more painful injection owing to limited diffusion of injected steroid and local anaesthetic.
The clinical diagnosis of de Quervain’s disease is usually straightforward. The value of ultrasound is to confirm the diagnosis, exclude underlying tendinosis or tendon tear, assess the retinaculum, detect whether septa are present within the first extensor compartment and guide steroid injection into the tendon sheath or retinacular division in resistant cases.
Proximal Intersection Syndrome
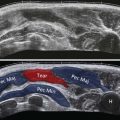
Proximal intersection syndrome, also known as ‘oarsman’s forearm’ or ‘crossover syndrome’, results from friction between the extensor carpi radialis brevis and longus tendons with the myotendinous junctions of abductor pollicis longus and extensor pollicis brevis. This condition is typically encountered in occupational or sports activities involving repetitive wrist flexion and extension, such as rowing or weightlifting. Patients present with pain and swelling along the dorsal radial aspect of the distal forearm. Fluid and synovitis are present in the tendon sheath of extensor carpi radialis brevis and longus at the level at which they are crossed by the musculotendinous junction of abductor pollicis longus and extensor pollicis brevis ( Figs 11.4 and 11.5 ). The area of intersection is usually approximately 4 cm proximal to Lister’s tubercle. Clinical crepitus during the US examination is a useful sign.
| Tenosynovitis (in intersection syndrome) may not, however, be limited to the site of crossover but can extend distally beyond the radiocarpal joint. |


Distal Intersection Syndrome
Distal intersection syndrome occurs at the crossover between the extensor carpi radialis brevis and longus tendons (second compartment) and the extensor pollicis longus tendon (third compartment), just distal to Lister’s tubercle. It is usually not the result of overuse. The deep surface of the extensor carpi radialis brevis and longus tendons is typically impinged by bony spurs due to osteoarthritis, scapholunate advanced collapse (SLAC) wrist or Colles’ fracture that result in tenosynovitis of the second extensor compartment. The biomechanical pulley effect exerted by Lister’s tubercle on the extensor pollicis longus tendon as it leaves the third compartment and crosses over the extensor carpi radialis tendons, together with a likely constricting effect of the retinaculum of the third compartment, puts the extensor pollicis longus tendon at risk. Ultrasound demonstrates a variable combination of tendinosis and tenosynovitis of the second and third extensor compartments centred at the point of intersection and underlying bony spurs impinging on the tendons. A third intersection syndrome is occasionally assigned to friction between the radial nerve and the first extensor compartment as it crosses it (Wartenberg syndrome).
Extensor Pollicis Longus Tenosynovitis
The extensor pollicis longus tendon runs in the third extensor compartment along the medial aspect of Lister’s tubercle. Mechanical friction against Lister’s tubercle results in tenosynovitis that presents with pain localized around the tubercle and, less commonly, with local crepitus during thumb movement. Restricted space beneath the retinaculum of the third compartment limits distension of the extensor pollicis longus tendon sheath at the level of Lister’s tubercle, except in cases of a very large effusion. More commonly, tendon sheath fluid accumulates just proximal to Lister’s tubercle and distally after the tendon has crossed extensor carpi radialis longus ( Fig. 11.6 ).