Bone Disease Around the Shoulder
Bony Irregularity in the Humeral Head
Many bony abnormalities will be encountered whilst performing rotator cuff ultrasound. Some of these are common traumatic lesions, including fractures of the greater tuberosity and Hill–Sachs lesions, others are less well understood. The location of the lesion on the humeral head can sometimes be a clue to the underlying cause.
A bone defect in the anterior aspect of the humeral head could be due to a reverse Hill–Sachs lesion. These occur as a result of impaction of the humeral head against the anterior glenoid during a posterior dislocation. Bony irregularity may also be encountered in the humeral head deep to the subscapularis tendon. This is sometimes referred to as a Welch lesion. Although the cause is unknown, it is frequently found in asymptomatic individuals and, therefore, it is generally not regarded as clinically significant. It is often not located at the tendon insertion but medial to it.
More laterally, bony irregularity is commonly encountered around the biceps tendon groove. This is likely to be the consequence of enthesopathy and is most commonly seen in association with chronic rotator cuff disease. In some cases the degree of bony abnormality can be so marked as to narrow the groove itself and constrict the biceps tendon, leading to biceps tendinopathy and rupture.
Greater Tuberosity Fracture
Fractures of the greater tuberosity are more easily detected by ultrasound than plain films ( Fig. 4.1 ). They are a common cause of persistent shoulder pain following a fall on the outstretched hand where plain films have been considered to be normal. These avulsion fractures may involve the supraspinatus insertion on the greater tubersosity or, less often, the subscapularis insertion on the lesser tuberosity. Ultrasound demonstrates a cortical break associated with focal tenderness. The degree of displacement can be assessed with reasonable reliability, although not as accurately as with a CT scan. This is usually between 1 and 8 mm displacement, with larger displacements more significant as they may precipitate or accentuate subacromial impingement. It is also helpful to give an indication of the proportion of the supraspinatus footprint that is attached to the fracture fragment.

Supraspinatus Footprint Lesions
Bony irregularity is not infrequently identified at the supraspinatus insertion. The cause is not known with certainty. It may begin with traction enthesopathy, but secondary fluid ingress may enlarge the bony defect that can become quite large in some patients. The presence of bony regularity does not always indicate a supraspinatus tear; however, apart from acute tears, it is unusual to encounter a significant supraspinatus lesion where the underlying bone is completely normal.
Hill–Sachs Lesion
Bony abnormalities on the posterior aspect of the humeral head could be due to previous anterior dislocation. The typical Hill–Sachs lesion is due to an impaction of the posterolateral aspect of the humeral head against the anterior glenoid margin ( Fig. 4.2 ). In addition to detection, the size of the defect should be assessed and particularly whether there is any likelihood of it becoming locked against the posterior glenoid margin during external rotation. Large lesions may influence surgical decisions. Measurement of the distance between the bony margins and the depths of the lesion can be provided with ease during a routine ultrasound examination. It is also helpful to assess the position of the Hill–Sachs lesion with respect to the posterior glenoid margin during external rotation, though patients with recurrent dislocation may be apprehensive during the manoeuvre. This is to determine whether there is the potential to reengage at physiological external rotation angles. In large lesions and lesions where there is the potential to engage, additional anterior capsule tightening may be carried out at surgery.

The rotator cuff should also be assessed in patients who have had shoulder dislocations as up to one-third may have associated cuff tears. The incidence of tears in patients with a first dislocation is higher than that for recurrent dislocations. Women appear to rupture the rotator cuff more often than men following dislocation.
Posterosuperior Impingement
A less common cause of a posterolateral bony injury is posterosuperior impingement. This is where the posterosuperior aspect of the humeral head may impinge against the posterosuperior labrum. This is most commonly seen in throwing sports but can also occur in tennis during the serve. There is some role for using ultrasound in patients with posterosuperior impingement, though it is recognized that a complete evaluation of the glenoid labrum is not possible in many patients. The position of the humeral head and glenoid margin can be assessed during a simulated throwing manoeuvre. Bony irregularity of the humeral head that comes into contact with the glenoid during the cocking phase is suggestive of posterosuperior impingement. Vascular channels may also cause bony irregularities and these are generally quite small and in a different location. Injuries to the labrum are discussed in the next section.
The Labrum and Glenohumeral Ligaments
The Labrum
Many parts of the glenoid labrum are amenable to ultrasound investigation; however, some of the most important, namely the superior labrum, are not. Some progress has been made in the ultrasound diagnosis of anteroinferior labral disease and in posterosuperior impingement. In thin patients the posterior and posterosuperior glenoid labrum can be moderately well seen. It is a triangular shaped, bright structure with an appearance typical of fibrocartilage. In larger patients, it is more difficult to reliably assess the posterior labrum and, as with the knee meniscus and the acetabular labrum, it is difficult to firmly exclude tears. Compared with arthroscopy, ultrasound performs well in differentiating normal from abnormal labra (tear or degeneration) in this location; however, its true clinical value has yet to be established.
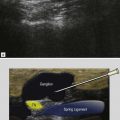
The glenoid labrum is prone to paralabral cyst formation akin to the knee meniscus and acetabular labrum. The cysts are characteristically fluid filled, largely anechoic with scattered bright foci. The most recognized site is an origin from the posterosuperior labrum, but other locations, including between the deltoid muscle and the subscapularis tendon, between the deltoid muscle and the biceps tendon and below the coracoacromial ligament, are also described. Cysts arising from the posterosuperior labrum most commonly track medially along the dorsal lip of the glenoid into the spinoglenoid notch. Here they expand and may compress the suprascapular nerve within the notch, leading to atrophy predominantly of the infraspinatus and occasionally the supraspinatus muscles. Patients complain of pain and weakness that may improve following aspiration of the cyst. The most common cause of infraspinatus atrophy is chronic nerve traction in the absence of a cyst.
The Glenohumeral Ligaments
The capsule of the shoulder joint is reinforced in several locations anteriorly by condensations that form the glenohumeral ligaments. When the joint is distended the glenohumeral ligaments may be recognized as areas where the capsule remains undisplaced by effusion, as the fluid preferentially extends between them. The glenohumeral ligaments become important in several clinical situations. The superior glenohumeral ligament can be visualized as part of the rotator interval forming its inferomedial margin, deep to the biceps tendon as it enters the groove. It can be torn as part of a rotator interval tear or become inflamed in patients with adhesive capsulitis (frozen shoulder). The middle and inferior glenohumeral ligaments may be injured in patients with anterior dislocation. The anterior limb of the inferior glenohumeral ligament is the most important as it attaches to the anteroinferior glenoid. This area can be examined by ultrasound; however, it is generally regarded as a less effective means of assessing the anteroinferior labrum than MRI or MR arthrography. The posterior limb of the inferior glenohumeral ligament is important in patients with internal instability. Capsulitis in this area leads to reduced internal rotation (GIRD phenomenon), which leads to abnormal glenohumeral contact which in turn, predisposes to tears of the superior and the posterosuperior labrum. Consistent ultrasound findings in capsulitis of the posterior limb of the inferior glenohumeral ligament have not been described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree