Forearm Anatomy
The anatomy of the forearm in one sense is as straightforward as the arm in that there are only two compartments, flexor and extensor, separated by an interosseous membrane. It is made a little trickier, however, as the flexor and extensor muscles begin medially and laterally respectively and then rotate as they are followed distally. In the midforearm, the flexor compartment occupies the anterior part of the forearm; the extensor compartment occupies the posterior and lateral part. The easiest method to identify a particular muscle of the forearm is to begin at the wrist with its tendon. The tendons at the wrist are clearly separate from each and occupy well-recognized compartments. The anatomy of the wrist and methods to remember tendon names are described in a later section. Once the tendon is found, it can be followed proximally and its associated muscle located.
Flexor Compartment
The two main muscles of the flexor compartment are flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), which occupy the central part of the compartment and make up most of its bulk. Overlying these are three muscles, flexor carpi ulnaris (FCU), palmaris longus and flexor carpi radialis (FCR) ( Fig. 10.1 ). The final member of the compartment, flexor pollicis longus (FPL), arises from the radius and lies alongside flexor digitorum profundus in the mid- and distal forearm.

The three principal nerve trunks, median, ulnar and radial, all lie in the anterior, though strictly the radial nerve is still in the lateral component of the posterior compartment, albeit in a very anterior location. Ulnar and radial nerves are accompanied by their corresponding arteries. The median nerve lies more centrally between flexor digitorum superficialis and profundus. Occasionally, the median nerve is also accompanied by a persistent median artery. The anterior interosseous nerve and its accompanying artery are located between flexor digitorum profundus and flexor pollicis longus in close proximity to the interosseous membrane.
Extensor Compartment
In the extensor compartment, three separate layers are discernible: two posterior (superficial and deep) and one lateral. The muscles in the lateral compartment are brachioradialis, and more distally extensor carpi radialis longus (ECRL) and brevis (ECRB) ( Fig. 10.2 ), whose tendons will ultimately form extensor compartment 2. In the posterior section, the superficial layer contains extensor digitorum (ED), extensor digiti minimi (EDM) and extensor carpi ulnaris (ECU) (extensor compartments 4, 5 and 6) ( Fig. 10.3 ). The deep component contains abductor pollicis longus (APL) on the radial side of extensor pollicis longus (EPL), forming extensor compartments 1 and 3 respectively. More distally, abductor pollicis longus will receive an additional component from extensor pollicis brevis (EPB) to complete compartment 1. In the proximal forearm, the extensor compartments from radial to lateral are therefore 2, 1, 3, 4, 5 and 6. It is clear that 1 and 2 are not optimally arranged and are going to have to cross each other to reach their ultimate destination. The crossover occurs just proximal to the wrist.


Although it is not particularly large, the main nerve in the extensor compartment is the posterior interosseous nerve (PIN). This is the major motor division of the radial nerve, formed below the elbow joint and passing into the posterior compartment between the two heads of supinator. Unlike its anterior namesake, the posterior interosseous nerve does not directly lie on the interosseous membrane, but between the superficial (EDC, EDM and ECU) and deep (APL and EPL) muscle groups. It can be followed distally where it is located deep to extensor digitorum communis at the level of the wrist.
Which Nerve Innervates Which Muscle?
Neural compression syndromes manifest on imaging in two ways. At the level of the compression, the nerve is usually enlarged and in many cases the lesion causing the compression can be seen. Distal to the compression, the innervated muscle may atrophy. The ultrasound features of this are usually late. MRI is more sensitive as it can also pick up the oedematous stage of denervation, which ultrasound does not. It is helpful, therefore, to know the innervation of the forearm muscle so that the correct pattern of atrophy may be recognized.
Radial Nerve
The radial nerve innervates the following muscles: triceps brachii (lateral and medial heads), anconeus, brachioradialis, extensor carpi radialis longus. Via the posterior interosseous nerve it also innervates: extensor carpi radialis brevis (ECRB), supinator, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus and extensor indicis (EI).
Ulnar Nerve
The ulnar nerve innervates the following muscles: flexor carpi ulnaris and flexor digitorum profundus (medial half). Via its deep branch it innervates: hypothenar muscles, opponens digiti minimi (ODM), abductor digiti minimi (ADM), flexor digiti minimi (FDM), third and fourth lumbrical muscles, dorsal interossei (DI), palmar interossei (PI) and adductor pollicis (AP). And via its superficial branch, the ulnar nerve innervates palmaris brevis.
Median Nerve
The median nerve innervates the following muscles: pronator teres, flexor carpi radialis, palmaris longus and flexor digitorum superficialis. Via its anterior interosseous branch: flexor digitorum profundus (lateral half), flexor pollicis longus and pronator quadratus.
Wrist Anatomy and Techniques
Overview
The most commonly employed position to examine the wrist and hand is to have the patient seated opposite the examiner. Both wrists can be placed on the examination couch, allowing full access and side-to-side comparison. Plenty of coupling jelly is required due to the varied contours of the hand, consequently an absorbent pad placed beneath the hand is essential.
As with other joints, the patient’s symptoms will direct the examination and the efficacy of ultrasound is highest when there is a specific localizing symptom. If pain is more diffuse, MRI is more likely to be helpful. The wrist examination, therefore, will be separated into specific areas with specific imaging goals in each area.
The examination of the patient with pain on the dorsal aspect of the wrist begins with an assessment of the extensor tendons. These are arranged in six compartments numbered accordingly from radial to ulnar. Each compartment is associated with specific pathology. As with tendons elsewhere, the extensor tendons are best assessed in the axial plane.
The tendons on the flexor side of the wrist are also arranged in compartments. The largest compartment is the carpal tunnel. This contains the superficial and deep flexor tendons, flexor pollicis longus tendon and the median nerve. The finger flexors share a single large synovial compartment. The flexor pollicis longus tendon has its own synovial sheath. The other three flexor tendons are flexor carpi radialis, flexor carpi ulnaris and palmaris longus. Flexor carpi radialis has its own compartment on the medial aspect of the scaphoid and tripezium tubercle and inserts on the base of the second metacarpal. Flexor carpi ulnaris inserts into the pisiform.
Position Variations
For some interventional procedures, particularly where the patient is anxious and there is a risk of fainting, an alternative position is to have the patient lying prone with their arm extended above their head, the so-called Superman position. This also allows nearly as much access to all parts of the wrist and hand. In addition, if an interventional procedure is required then, the patient’s anxiety will be allayed by being recumbent and not having to sit up and ‘observe’ the procedure.
Position 1: Extensor Wrist Radial Side
Imaging Goals
- 1.
Identify extensor compartments (ECs) 1 and 2.
- 2.
Locate and track extensor pollicis longus.
- 3.
Locate the dorsal aspect of the scapholunate ligament (SLL).
Technique
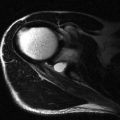
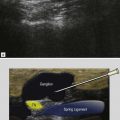
Radial sided wrist pain is common and ultrasound is helpful in detecting many of its causes. These include common conditions like de Quervain’s tenosynovitis and dorsal ganglion cyst. The examination begins with the identification of EC1, EC2 and EC3 ( Fig. 10.4 ). There are two methods used to identify these three compartments. The easiest method, and best for beginners, is to identify a bony prominence on the dorsal aspect of the radius called Lister’s tubercle ( Fig. 10.5 ). With the palm of the hand placed flat on the examination couch, the probe is placed in axial position over the middle of the forearm. The radius and ulnar bony margins are identified and the probe is moved distantly along the dorsal aspect of the radius. Just before the wrist joint is reached, a bony prominence is seen. This is Lister’s tubercle, which separates the second (lateral) from the third (medial) compartments. The second compartment contains two tendons and the third compartment a single tendon. The probe is then moved further to the radial side to locate the first compartment, which also contains two tendons. Note that the probe has to be moved ‘around the corner’ of the posteroradial margin of the radius to find compartment 1 ( Fig. 10.6 ).



With practice, the examination can begin directly over the first. The patient places the ulnar border of their hand on the examination couch. EC1 lies along the uppermost border of the radius in this hand position, in a very superficial location. Placing the probe in the axial position at the uppermost part of the wrist will reveal EC1 and its two tendons, the abductor pollicis longus and extensor pollicis brevis. The two tendons are surrounded by a tendon sheath and contained within the extensor retinaculum. The extensor retinaculum is a well-defined fibrous connective tissue structure that bridges all six extensor compartments. It is important to identify the EC1 retinaculum, as thickening may be the first abnormality encountered in patients with sclerosing tenosynovitis. The retinaculum is seen as a very thin hyporeflective line overlying the tendons close to the tip of the radial styloid ( Fig. 10.7 ). It may be better seen by rotating the probe 90° and viewing the tendons in their long axis. If it is difficult to identify, it is unlikely that it is thickened. Close by, the superficial branch of the radial nerve may also be seen passing over the EC1 as it is tracked distally.

A number of variations may be identified in the EC1. Most commonly, the two tendons share a single compartment. Occasionally a septum will be seen between them with separation into two compartments. Another variation is that, rather than having two tendons, a number of separate tendon slips may be identified.
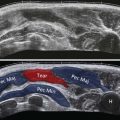
Returning to the axial plane and moving the probe a little towards the ulnar side reveals EC2. At this stage, it is often easier for the patient now to rest the palm of their hand on the examination couch. EC2 also contains two tendons: extensor carpi radialis longus and brevis. The brevis tendon is the more ulnar of the two, inserting into the base of the third metacarpal, whereas the longus inserts into the base of the second. They form the dorsal aspect of the anatomical snuff box. Keeping the probe in the axial plane and tracing proximally, it will be noted that EC1 passes over the dorsal aspect of EC2 in the distal forearm. This area is called the ‘crossover point’ ( Fig. 10.8 ) and a frictional tendinopathy may occur in this location. This is called the crossover or intersection syndrome and it is particularly common in rowers. Crepitus is a common finding in this condition and can be felt beneath the ultrasound probe.