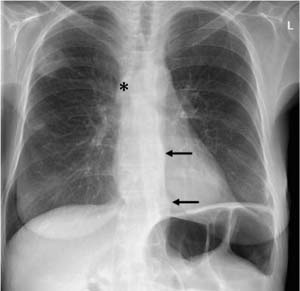
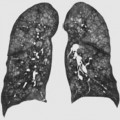
9 Disorders of the Pulmonary Circulatory System Thrombotic occlusion of the pulmonary arterial system. Common cause of acute chest pain with respiratory distress Usually originating in the pelvic or leg veins, the thrombi restrict the blood supply to the lung CTA and, to a lesser extent, ventilation/perfusion scanning (lung scan). Nonspecific inconclusive findings: Platelike atelectasis Directly demonstrates embolisms in the pulmonary arterial system (filling defects). Wedge-shaped perfusion defect. Intraluminal contrast filling defects Asymptomatic in about 80% of cases, rendering clinical diagnosis difficult Anticoagulation and fibrinolysis Good with therapy Confirm or exclude diagnosis Fig. 9.1 Massive bilateral pulmonary embolism in a 79-year-old man with acute coronary syndrome. CTA shows thrombi incompletely blocking the blood flow in both main pulmonary trunks, the superior and inferior lobe arteries, and the segmental branches: findings are consistent with acute pulmonary embolism. The plain chest radiographs were normal. Fig. 9.2 Pulmonary infarct in a 47-year-old woman with protein S deficiency. The plain chest radiograph shows a faint wedge-shaped area of opacification with a pleural base in the right upper lung field and a second smaller area in the middle lung field consistent with infarct pneumonia. The patient had a known history of thromboembolic disease, which had led to occlusion of the inferior vena cava. Collateralization via the expanded azygos vein (*, arrows).
Pulmonary Embolism
Definition
 Epidemiology
Epidemiology
 In 80% of cases however, acute pulmonary embolism remains asymptomatic.
In 80% of cases however, acute pulmonary embolism remains asymptomatic.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 This leads to capillary damage, transudation, hemorrhage, and occasionally necrosis.
This leads to capillary damage, transudation, hemorrhage, and occasionally necrosis.
Imaging Signs
 Modality of choice
Modality of choice
 Radiographic findings
Radiographic findings
 High-riding diaphragm
High-riding diaphragm  Pleural effusion
Pleural effusion  Local oligemia (Westermark sign)
Local oligemia (Westermark sign)  Rarely pulmonary infarction, appearing as a wedge-shaped opacity with a pleural base.
Rarely pulmonary infarction, appearing as a wedge-shaped opacity with a pleural base.
 CT findings
CT findings
 Nuclear medicine
Nuclear medicine
 Pathognomonic findings
Pathognomonic findings
 Signs of right heart strain.
Signs of right heart strain.
Clinical Aspects
 Typical presentation
Typical presentation
 Typical triad of chest pain, respiratory distress, and hemoptysis occurs in only about 5%
Typical triad of chest pain, respiratory distress, and hemoptysis occurs in only about 5%  Deep venous thrombosis in the pelvis or lower extremity is present in less than 50%.
Deep venous thrombosis in the pelvis or lower extremity is present in less than 50%.
 Therapeutic options
Therapeutic options
 A venal caval filter may be indicated in deep venous thrombosis in the pelvis or lower extremity where medical treatment is ineffective or contraindicated.
A venal caval filter may be indicated in deep venous thrombosis in the pelvis or lower extremity where medical treatment is ineffective or contraindicated.
 Course and prognosis
Course and prognosis
 Fatal in about 20% of cases if left untreated.
Fatal in about 20% of cases if left untreated.
 What does the clinician want to know?
What does the clinician want to know?
 Extent (unilateral or bilateral, central or peripheral).
Extent (unilateral or bilateral, central or peripheral).
Differential Diagnosis
Pneumonia | – Fever – One must consider the possibility of embolism where nonspecific shadows are present |
Tips and Pitfalls
Insufficient filling of the pulmonary arteries  Breathing artifacts.
Breathing artifacts.
Selected Reference
Guilabert JP et al. Can multislice CT alone rule out reliably pulmonary embolism? A prospective study. Eur J Radiol 2007; 62: 220–226
Pulmonary Arterial Hypertension
Definition
Abnormally elevated blood pressure in the pulmonary artery (mean pulmonary arterial pressure at rest > 25 mmHg, with exercise > 30 mmHg).
 Epidemiology
Epidemiology
Idiopathic form is rare  Secondary forms are far more common.
Secondary forms are far more common.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Increase in pulmonary arterial pressure due to cardiac pathology (left-to-right shunt, mitral stenosis, anomalous pulmonary venous connection, etc.) or pulmonary pathology (thromboembolic disease [CTEPH], emphysema, pulmonary fibrosis, etc.)  This leads to dilatation of the central pulmonary arteries
This leads to dilatation of the central pulmonary arteries  Findings in idiopathic pulmonary arterial hypertension include fibrosis and proliferative muscularization of arterioles
Findings in idiopathic pulmonary arterial hypertension include fibrosis and proliferative muscularization of arterioles  Pulmonary arterial hypertension is classified as idiopathic, familial, or associated; the latter occurs in disorders such as venous occlusive disease or capillary hemangiomatosis.
Pulmonary arterial hypertension is classified as idiopathic, familial, or associated; the latter occurs in disorders such as venous occlusive disease or capillary hemangiomatosis.
Imaging Signs
 Modality of choice
Modality of choice
Radiographs, CTA, pulmonary angiography.
 Radiographic findings
Radiographic findings
Dilated central pulmonary arteries (diameter of the middle part of the right pulmonary artery > 16 mm in men, > 14 mm in women) with abrupt changes in caliber toward the periphery  Signs of right heart strain—enlarged area of contact between the anterior wall of the heart and the sternum, prominent pulmonary trunk, prominent main pulmonary artery segment.
Signs of right heart strain—enlarged area of contact between the anterior wall of the heart and the sternum, prominent pulmonary trunk, prominent main pulmonary artery segment.
 CTA findings
CTA findings
The pulmonary trunk is wider than the ascending aorta  Abrupt changes in caliber
Abrupt changes in caliber  In CTEPH there are mural irregularities, intraluminal webs and bands, ste-noses, and/or thromboembolic vascular occlusion
In CTEPH there are mural irregularities, intraluminal webs and bands, ste-noses, and/or thromboembolic vascular occlusion  Mosaic perfusion
Mosaic perfusion  Signs of right heart strain—right ventricular dilatation and hypertrophy with protrusion of the interventricular septum against the left ventricle.
Signs of right heart strain—right ventricular dilatation and hypertrophy with protrusion of the interventricular septum against the left ventricle.
 Pulmonary angiographic findings
Pulmonary angiographic findings
Vascular picture is identical to CTA.
 Pathognomonic findings
Pathognomonic findings
Dilated central pulmonary arteries with abrupt changes in caliber toward the periphery.
Clinical Aspects
 Typical presentation
Typical presentation
Symptoms are nonspecific—dyspnea during exercise  Limited exercise tolerance
Limited exercise tolerance  Fatigue
Fatigue  Advanced-stage disease shows signs of right heart failure.
Advanced-stage disease shows signs of right heart failure.
 Therapeutic options
Therapeutic options
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree