Disorders of the Wrist
Miscellaneous
Neural Entrapment
Carpal Tunnel Syndrome
Median Nerve Changes
Size
The median nerve is typically swollen at the proximal carpal tunnel and flattened as it passes beneath the flexor retinaculum and at the distal extent of the tunnel (Fig. 13.1), regardless of the cause of compression. An abrupt change in the calibre of the nerve at the proximal carpal tunnel is referred to as the ‘notch sign’ (Fig. 13.2).
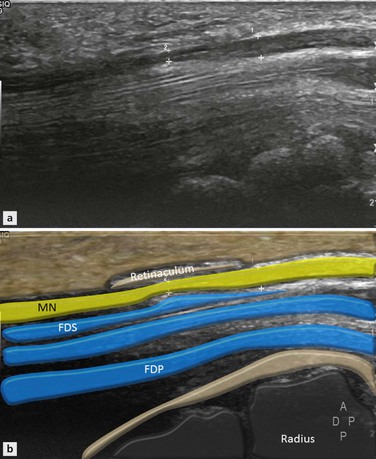
Figure 13.1 Sagittal image of volar aspect of wrist. There is a change in calibre of the median nerve as it passes under the flexor retinaculum that is consistent with CTS. Some mild separation of the tendon fibres is evident.
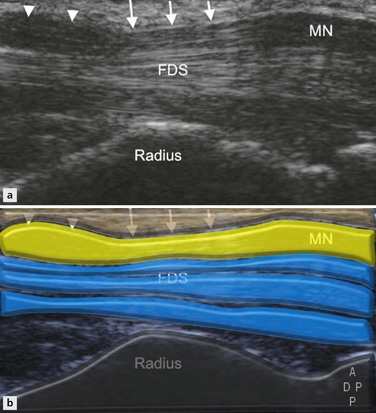
Figure 13.2 CTS. Longitudinal image shows swelling and hypoechogenicity of the MN just proximal to the carpal tunnel (arrowheads). The nerve is flattened as it passes beneath the flexor retinaculum (arrows), resulting in a change in calibre of the nerve, which is referred to as the ‘notch sign’. The MN lies superficial to the FDS tendons.
The cross sectional area of the median nerve should be measured at the point of maximum enlargement. This usually occurs just proximal to the flexor retinaculum, a position located slightly cranial to the pisiform.
Two methods are used to measure the cross sectional area of the median nerve: the direct method, using the ellipse tool on the ultrasound machine, or the indirect method, by means of the ellipse formula [(maximum anteroposterior diameter) × (maximum transverse diameter) × ( )]. There is a high degree of correlation between the two methods. Transducer positioning potentially affects measurement of the median nerve cross sectional area.
)]. There is a high degree of correlation between the two methods. Transducer positioning potentially affects measurement of the median nerve cross sectional area.
The transducer should always be perpendicular to the nerve, including when the nerve courses obliquely from superficial to deep.
Tilting the transducer over the nerve or slightly changing wrist position can achieve optimal transducer orientation.
Ranges between 9 mm2 and 15 mm2 have been proposed.
Comparing cross sectional area measurements of the median nerve at the level of the carpal tunnel and pronator quadratus has been proposed to eliminate interindividual and internerve variability. A difference in the cross sectional area of 2 mm2 or greater yielded the greatest sensitivity and specificity for the diagnosis of CTS.
Occasionally, the notch sign may occur at the distal edge of the retinaculum (inverted notch sign). In these cases, the nerve is flattened at the distal tunnel and no shape change is seen at the proximal tunnel. An inverted notch sign indicates distal compression, which should be highlighted in the report so that appropriate distal or palmar electrophysiological testing is performed.
Flexor Retinaculum Changes
Volar bowing of the flexor retinaculum is seen secondary to increased pressure within the carpal tunnel (Fig. 13.3). This is assessed at the distal end of the carpal tunnel (hamate–trapezium level). A line joining the hook of the hamate and the tubercle of the trapezium is made. The largest distance from this line to the retinaculum reflects the degree of volar bulging. A value of more than 4 mm is considered significant.
Carpal Tunnel Content
The most common cause of CTS is tenosynovitis of the flexor tendons. Ultrasound demonstrates hypoechoic fluid and synovitis in the tendon sheaths which separate the flexor tendons (Fig. 13.3). Doppler signal depends on the activity of the synovitis.
When scanning for tenosynovitis in the carpal tunnel, dynamic scanning in the transverse plane during finger flexion and extension helps differentiate the tendons from echogenic synovitis.
Space occupying lesions within the carpal tunnel are seen well with ultrasound. Ganglia are the commonest and appear as well-defined anechoic masses with no internal vascularity. They usually arise in the deep portion of the tunnel from the wrist joint and displace the median nerve and flexor tendons anteriorly against the flexor retinaculum. Solid tumours include lipomas (Fig. 13.4), neural tumours and giant cell tumours of the tendon sheath. A persistent median artery has been described as a cause of CTS. This is an accessory artery that arises from the ulnar artery in the proximal forearm and may accompany the median nerve through the carpal tunnel. Doppler imaging is useful for identifying it. Acute CTS may be secondary to acute thrombosis of this artery. Following penetrating injury, posttraumatic neuroma, which may affect only a portion of the median nerve, may occur (Fig. 13.5).
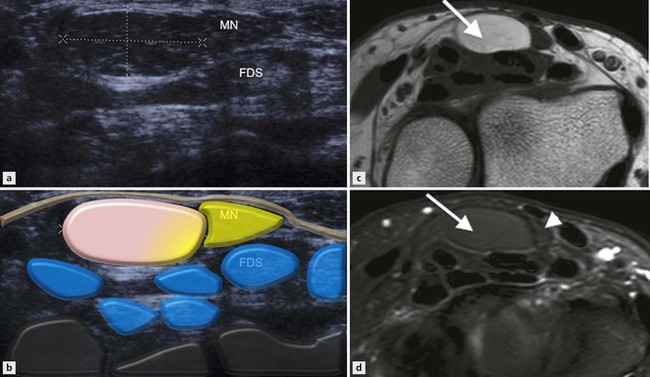
Figure 13.4 Carpal tunnel syndrome. (A, B) Transverse ultrasound image shows a solid mass (demarcated by calipers) displacing and compressing the MN in the carpal tunnel. Corresponding axial (C) T1 and (D) T2 fat saturation MR images confirm a lipoma in the carpal tunnel (arrow), which returns high-T1 signal and completely suppresses with fat saturation. Increased T2 signal of the MN (arrowhead) is in keeping with intraneural oedema.
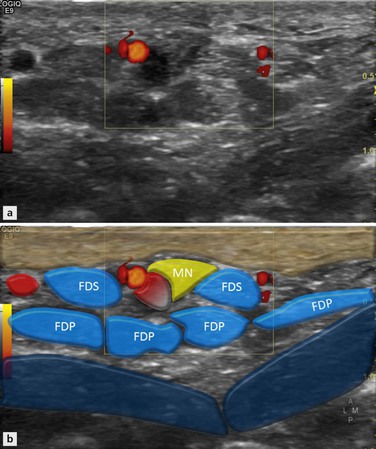
Figure 13.5 Axial image of volar aspect of wrist. There is a low-signal lesion arising from the radial aspect of the MN consistent with a median neuroma. The patient had a previous neuroma excised and this lesion represents a recurrence.
Anomalous muscles inside the carpal tunnel relate to the distal insertion of an anomalous muscle belly of the FDS of the index finger, the proximal insertion of a lumbrical muscle or an accessory flexor muscle. Accessory muscles have the typical echotexture of muscles with echogenic linear septa, change shape during contraction and relaxation, and can be seen to enter and exit the tunnel with finger extension and flexion. Abnormal bone extending into the carpal tunnel, such as callus formation or a dislocated lunate, is brightly echogenic with posterior acoustic shadowing.
Inflammatory Arthritis
Synovitis
A dorsal approach is usually best to assess carpal joint synovitis. The dorsal recesses of the radiocarpal and midcarpal joints are best imaged in the longitudinal plane. Transverse images at these levels are useful to differentiate deep intraarticular fluid and synovitis from superficial extensor tenosynovitis (Fig. 13.6). The distal radioulnar joint is best assessed in the transverse plane, often at a more proximal level than the joint line, where the joint capsule is more likely to distend.
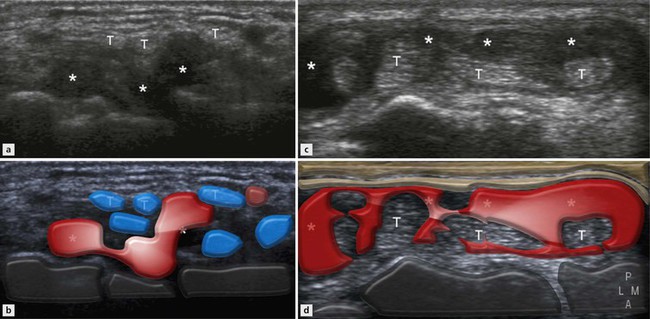
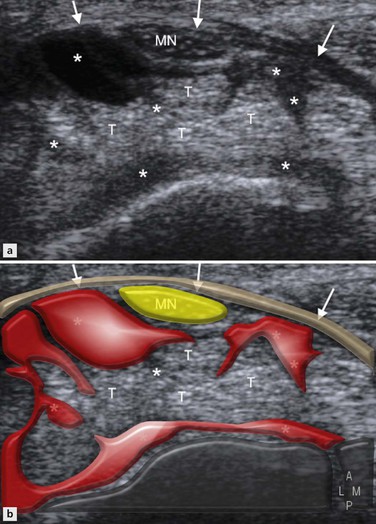
Figure 13.6 Synovitis versus extensor tenosynovitis. (A, B) Transverse image shows synovial effusion (*) in the dorsal recesses of the radiocarpal joint closely applied to the carpal bones and displacing the extensor tendons (T) posteriorly. (C, D
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree