Disorders of the Wrist
Radial
Tendon Disease
De Quervain’s Disease
The abductor pollicis longus and extensor pollicis brevis tendons are typically swollen and hypoechoic owing to oedematous change. They may be difficult to distinguish from one another as they become compressed in the confined space of the osteofibrous tunnel. The extensor retinaculum which is identified over the radial styloid can be thickened and hypoechoic, which may be an indication for release. Fluid and synovial thickening distend the tendon sheath, which is best seen surrounding the tendons distal to the retinaculum (Figs 11.1 and 11.2). Dynamic scanning shows irregular tendon gliding beneath the retinaculum during thumb extension.
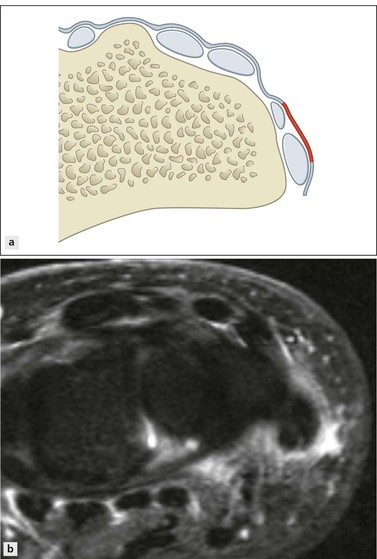
Figure 11.1 (A) The extensor retinaculum overlies the six extensor tendon compartments. The part overlying the first extensor compartment (red) becomes thickened in de Quervains disease. (B) Tendon sheath fluid and retinacular oedema in extensor compartment one.
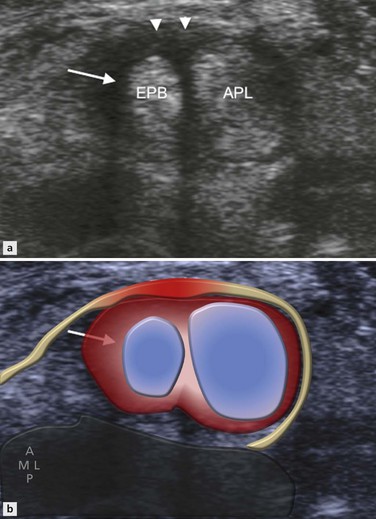
Figure 11.2 De Quervain’s tenosynovitis. Transverse image shows anechoic compressible fluid (arrow) and echogenic peripheral synovial hypertrophy (arrowheads) distending the abductor pollicis longus and the extensor pollicis brevis tendon sheath.
Care should be taken not to confuse the extensor retinaculum, which is noncompressible and located at the level of the radial styloid, with fluid within the tendon sheath, which is compressible and best seen distal to the radius.
Increased vascularity of the tendon sheath synovium and retinaculum is present in the acute phase due to inflammatory hyperaemia (Fig. 11.3).
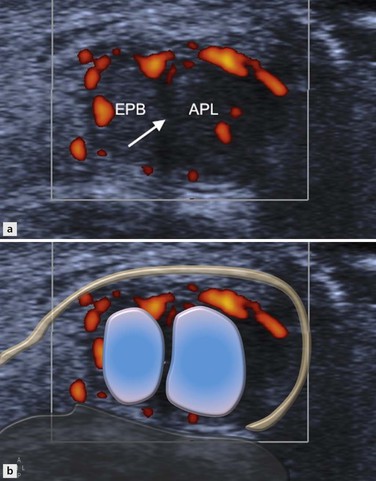
Figure 11.3 De Quervain’s tenosynovitis. Transverse image with power Doppler demonstrates increased vascularity of the abductor pollicis longus and the extensor pollicis brevis tendon sheath synovium. A paucity of peritendinous fluid is consistent with sclerosing tenosynovitis. A thin vertical hypoechoic septum (arrow) is present between the tendons.
A vertical septum splitting the first extensor compartment into two subtunnels for each of the tendons is encountered more frequently in patients with de Quervain’s disease and is thought to predispose to local tendon friction. Accessory vertical septa appear as thin hypoechoic linear bands between the tendons (Fig. 11.3). The inflammatory process may selectively involve one tendon when a septum is present. Identification of a septum is clinically significant as it forms a barrier to diffusion of injected steroids and requires decompression of both tunnels at surgery. A septum splitting the first extensor compartment and more sclerosing tenosynovitis may be indicative of a more painful injection owing to limited diffusion of injected steroid and local anaesthetic.
Proximal Intersection Syndrome
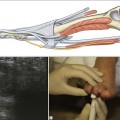
Proximal intersection syndrome, also known as ‘oarsman’s forearm’ or ‘crossover syndrome’, results from friction between the extensor carpi radialis brevis and longus tendons with the myotendinous junctions of abductor pollicis longus and extensor pollicis brevis. This condition is typically encountered in occupational or sports activities involving repetitive wrist flexion and extension, such as rowing or weightlifting. Patients present with pain and swelling along the dorsal radial aspect of the distal forearm. Fluid and synovitis are present in the tendon sheath of extensor carpi radialis brevis and longus at the level at which they are crossed by the musculotendinous junction of abductor pollicis longus and extensor pollicis brevis (Figs 11.4 and 11.5). The area of intersection is usually approximately 4 cm proximal to Lister’s tubercle. Clinical crepitus during the US examination is a useful sign.
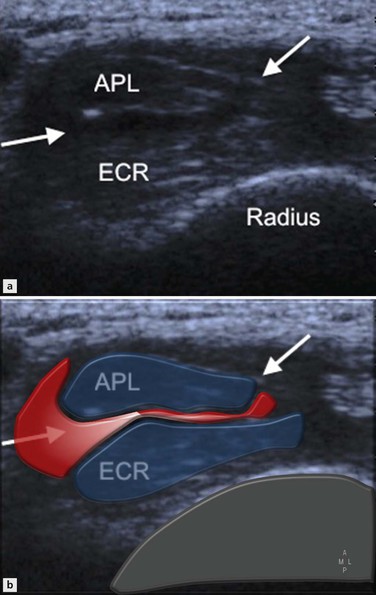
Figure 11.4 Proximal intersection syndrome. Transverse image depicts fluid in the tendon sheaths (arrows) at the crossover of the abductor pollicis longus and the extensor carpi radialis tendons.
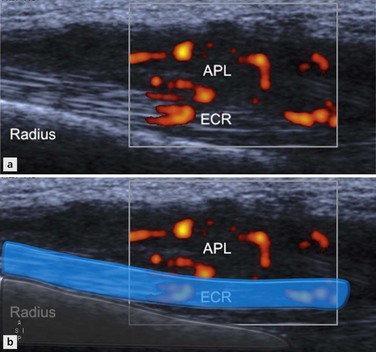
Figure 11.5 Proximal intersection syndrome. Longitudinal image with power Doppler demonstrates tenosynovitis with increased vascularity at the intersection of the abductor pollicis longus and extensor carpi radialis tendons, approximately 4 cm proximal to Lister’s tubercle.
Tenosynovitis (in intersection syndrome) may not, however, be limited to the site of crossover but can extend distally beyond the radiocarpal joint.
There is loss of the normal echogenic fat cleavage plane between the first and second extensor tendon groups. A true synovial fluid-filled bursa is a rare finding. The clinical symptoms may mimic those of scaphoid fracture, osteoarthritis of the first carpometacarpal joint, ganglion cyst or de Quervain’s tenosynovitis.