11 | Doppler Ultrasound in the Diagnosis of Fetal Anomalies |
It is axiomatic that the initial diagnosis of fetal anomalies is made by conventional gray-scale B-mode sonography. However, Doppler ultrasound—especially color-coded blood flow diagnosis—increasingly allows the diagnosis to be refined and more precisely delineated. Thus, whereas the detection of an anomaly depends on the experience of the examiner and the resolution of the B-mode image, the use of color Doppler ultrasound is highly advantageous in further exploring organ function and differential diagnosis. This is accepted unanimously for fetal echocardiography. However, even a simple example will demonstrate the importance of color Doppler ultrasound in the diagnosis of malformations: The differential diagnosis between an intracerebral cyst and an aneurysm can be made with certainty only using color-coded Doppler ultrasound, since an aneurysm will be outlined in color, while a cyst remains colorless.
But even the demonstration of a normal vascular tree or pathological changes in it can clarify fetal anomalies. For instance, the demonstration by color Doppler of the absence of a renal a. can prove renal agenesis.
However, the precondition for the diagnosis of fetal anomalies is the correct setting of the instrument. For the display of venous flows, the setting must be adapted to their slow range of flow velocities, i. e., a low pulse repetition frequency (PRF) must be selected. By contrast, the faster arterial flow rates can only be displayed accurately with higher PRFs.
Since, as stated above, the diagnosis of fetal anomalies depends primarily on a high-resolution B-mode image, only those fetal anomalies in various organ systems are described in the following for which diagnosis is facilitated by using color Doppler sonography. They are listed in Table 11.1.
Tabelle 11.1 Diagnoses and further differentiation of fetal malformations that can be markedly facilitated by color Doppler ultrasound.
Region of body | Fetal malformation Körperregion |
|---|---|
Central nervous system, head, neck | Arachnoid cysts, porencephalic cysts, intracranial neoplasms, hydrocephalus, tumors of the neck, fetal goiters, hemangiomata |
Lung | Hypoplasia of the lung (?), diaphragmatic herniae, hemangiomata |
Heart | All cardiac anomalies |
Gastrointestinal tract | Omphalocele, gastroschisis |
Urogenital system | Renal malformations |
Skeleton | Sacrococcygeal teratomata |
Other anomalies | Placenta, hydrops fetalis, anhydramnios, anomalies of the umbilical cord |
Anomalies in the Region of the Head and Neck
Examination of this region of the body by color Doppler is most profitable for anomalies of the fetal brain and soft-tissue tumors of the neck.
A normal color Doppler display of the blood supply at the base of the skull is shown in Figure 11.1.
A display showing intracerebral cysts might be of an actual cystic space such as an arachnoidal cyst, a ventricular hydrocephalic dilatation, cystic brain anomalies as in holoprosencephaly, choroid plexus cysts, or aneurysms of the vein of Galen. Naturally only aneurysms will show blood flow inside the cyst, while other anomalies by their nature do not (Fig. 11.2a–c).
Additionally, the spectral Doppler feature of Doppler ultrasound examination of the intracerebral aa., especially the middle cerebral a., permits conclusions to be drawn about intracerebral pressure.
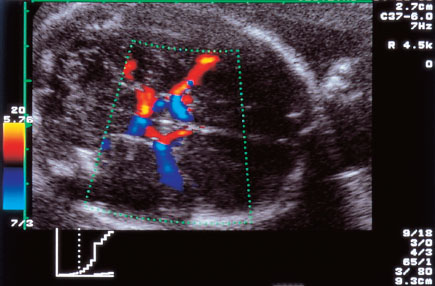
Fig. 11.1 Display of the normal vascular supply at the base of the skull. Circle of Willis with middle cerebral a.
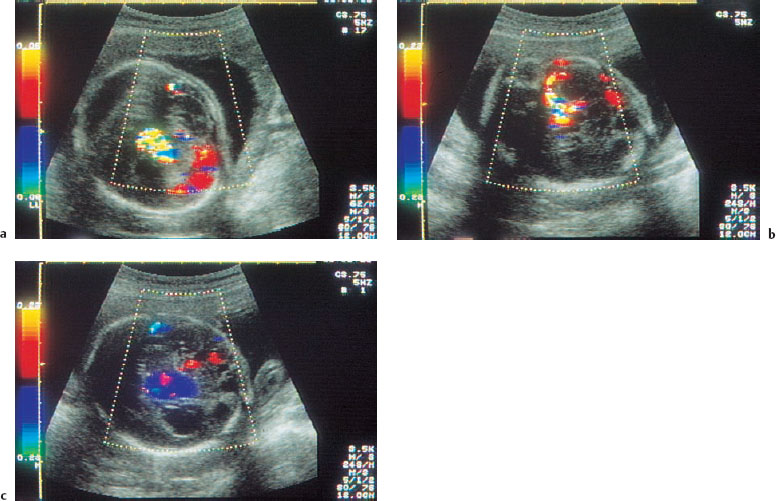
Fig. 11.2a Fetal brain with several cysts, which on color Doppler are seen to be filled with blood, showing they are aneurysms.
Fig. 11.2b,c Additional cuts display more aneurysms in the brain.
The thickness of the cerebral cortical mantle in hydrocephalus (Fig. 11.3a) is not an indicator of the prognosis for cognitive development. Perhaps in the future the degree of intracranial pressure, measured by Doppler sonography, may provide such an indication (Fig. 11.3b).
Postpartum changes in blood flow velocity in relation to the degree of ventricular dilatation in hydrocephalus may be divided into three stages:

Fig. 11.3a Fetal hydrocephalus in the 33rd week of gestation.
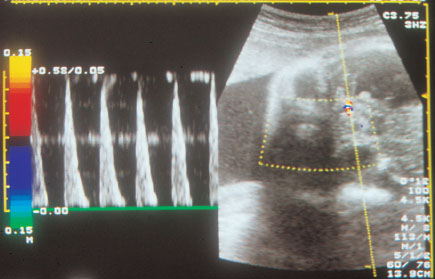
Fig. 11.3b Physiologically there should be diastolic forward flow in the 32nd week of gestation. The middle cerebral a. in this infant exhibits zero diastolic flow, which may indicate increased intracranial pressure.
Stage 1:
In the slowly developing so-called “low-pressure hydrocephalus,” in which the ventricles are only minimally dilated, no significant changes can be found by Doppler ultrasound in the flow rates in the intracranial vessels.
Stage 2:
In moderately dilated ventricles increased diastolic blood flows may be found, and these may lead to a reduced pulsatility index (PI). This phenomenon is interpreted as increased perfusion and a protective mechanism for cerebral tissue (brain sparing).
Stage 3:
Rapidly progressive ventricular dilatation is marked by a significant reduction in diastolic amplitude. In especially severe cases blood flow may even be reversed (Fig. 11.4). The result is a raised PI. Such a finding is an indicator of impending ischemic cerebral tissue damage.
A derivation of this postpartum procedure is the use of Doppler ultrasound ante partum.
In a fairly large number of cases of hydrocephalus Voigt and his co-workers (Voigt et al. 1995) demonstrated that increasing ventricular dilatation led to increased resistance in cerebral blood flow, with consequent impairment of perfusion. In this way the reduction in the cortical mantle was associated with an increase in intracerebral pressure. The authors point out that Doppler ultrasound is the ideal means of determining the correct time for delivery in order to prevent damage to the fetal brain by excessive pressure. Figure 11.5 shows the relationship between perfusion pressure and increased intracerebral pressure.
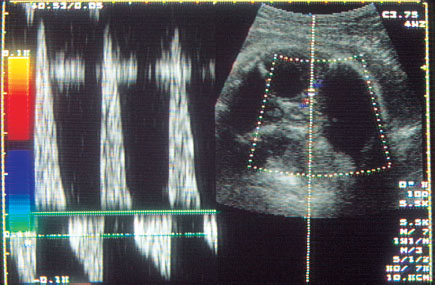
Fig. 11.4 Display of reverse diastolic flow in the middle cerebral a., suggesting very high intracranial pressure.
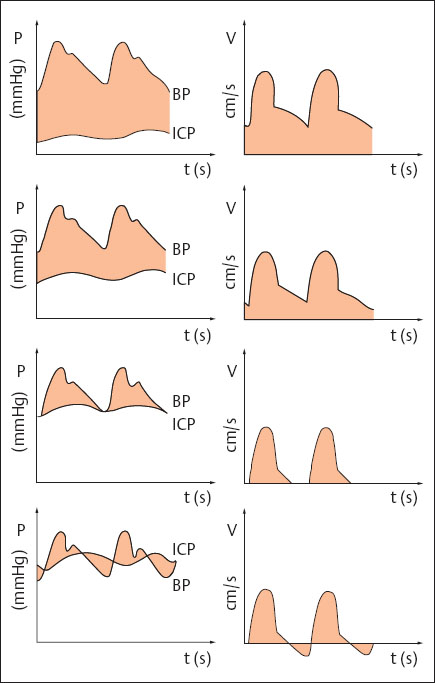
Fig. 11.5 Association between perfusion pressure (PP) and flow profile in the cerebral arteries (PP = BP–ICP). The left side shows the relation between blood pressure (BP), which is considered constant, and increasing intracranial pressure (ICP). The right shows the corresponding Doppler spectra that might be expected theoretically. As ICP increases, PP decreases with a consequent decrease in diastolic flow. Once ICP reaches end-diastolic pressure, no more forward flow can be detected. If ICP exceeds BP during diastole, the result is end-diastolic flow reversal (after Voigt et al 1995).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree