, Joungho Han2, Man Pyo Chung3 and Yeon Joo Jeong4
(1)
Department of Radiology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(2)
Department of Pathology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(3)
Department of Medicine Division of Pulmonary and Critical Care Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(4)
Department of Radiology, Pusan National University Hospital, Busan, Korea, Republic of (South Korea)
Abstract
Drug-induced lung injury is seen as a wide variety of histologic reaction patterns and thus as diverse CT findings. The most common are interstitial pneumonia and fibrosis (either usual interstitial pneumonia [UIP] or nonspecific interstitial pneumonia [NSIP]), eosinophilic pneumonia (including DRESS syndrome; drug reaction with eosinophilia and systemic symptoms), cryptogenic organizing pneumonia (COP), diffuse alveolar damage (DAD), and hypersensitivity pneumonia [1, 2]. Other reactions such as granulomatous pneumonitis, vasculitis, alveolar proteinosis, obliterative bronchiolitis, and veno-occlusive disease are uncommon [2]. None of these histologic patterns is specific for either drug reaction in general or the reaction to a particular drug. Consequently, the diagnosis of drug-induced lung disease is based on a combination of radiologic, clinical, and histologic (when imperative) findings in a patient who has received a drug known to cause the abnormalities.
Drug-induced lung injury is seen as a wide variety of histologic reaction patterns and thus as diverse CT findings. The most common are interstitial pneumonia and fibrosis (either usual interstitial pneumonia [UIP] or nonspecific interstitial pneumonia [NSIP]), eosinophilic pneumonia (including DRESS syndrome; drug reaction with eosinophilia and systemic symptoms), cryptogenic organizing pneumonia (COP), diffuse alveolar damage (DAD), and hypersensitivity pneumonia [1, 2]. Other reactions such as granulomatous pneumonitis, vasculitis, alveolar proteinosis, obliterative bronchiolitis, and veno-occlusive disease are uncommon [2]. None of these histologic patterns is specific for either drug reaction in general or the reaction to a particular drug. Consequently, the diagnosis of drug-induced lung disease is based on a combination of radiologic, clinical, and histologic (when imperative) findings in a patient who has received a drug known to cause the abnormalities.
Interstitial Pneumonitis and Fibrosis
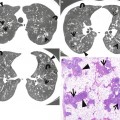
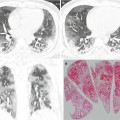
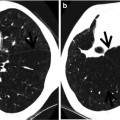
One of the most common forms of drug-induced pneumonitis is nonspecific interstitial pneumonia (NSIP) [1, 2] (Fig. 27.1). This is characterized histologically by homogeneous alveolar wall thickening by fibrous tissue and mononuclear inflammatory cells. The reaction is seen most commonly in association with methotrexate, amiodarone, or carmustine toxicity (Table 27.1). The corresponding thin-section CT (TSCT) findings usually consist of patchy or diffuse areas of ground-glass opacity (GGO) (Fig. 27.1). With progression, there may be evidence of fibrosis, including reticulation, traction bronchiectasis, and honeycombing. The abnormalities show typically lower lung zone predominance. In some patients, the fibrosis is patchy in distribution and predominantly peribronchovascular; fibrotic NSIP pattern, commonly in patients receiving nitrofurantoin [3].
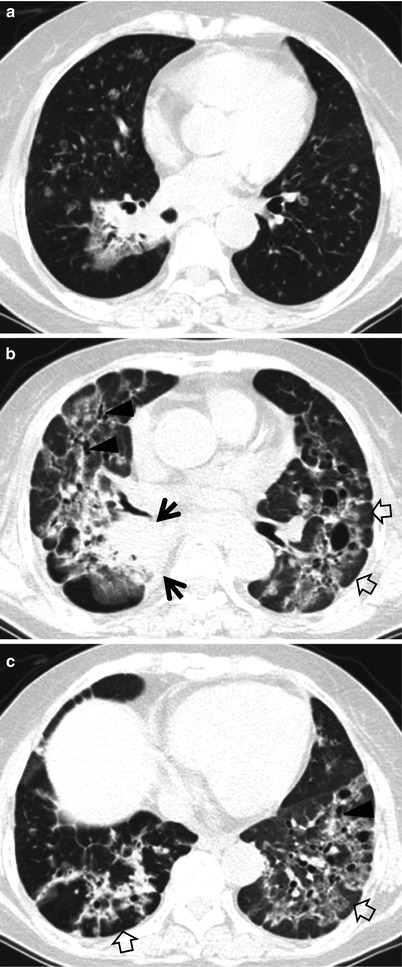
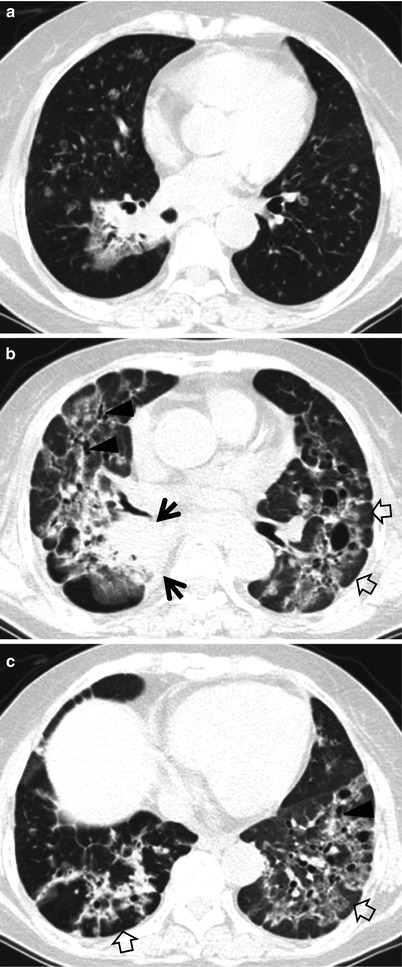
Fig. 27.1
Iressa (gefitinib)-associated pulmonary fibrosis of nonspecific interstitial pneumonia pattern of pulmonary fibrosis in a 75-year-old woman with lung adenocarcinoma. (a) Lung window image of CT scan (2.5-mm section thickness) obtained at level of right inferior pulmonary vein shows a 59-mm-sized mass in superior segment of right lower lobe and innumerable small cavitating and noncavitating nodules in both lungs (suggestive of pulmonary metastases). Patient received Iressa (gefitinib) chemotherapy. (b, c) Eighteen-month follow-up CT scans obtained at levels of right middle lobar bronchus (b) and liver dome (c), respectively, demonstrate still visible mass (arrows in b) in right lower lobe. Please also note ground-glass opacity, reticulation, traction bronchiectasis (arrowheads), and cystic lung changes in both lungs. Subpleural sparing (open arrows) and lung fibrosis of deep central involvement are noticed
Table 27.1
CT patterns of drug-induced lung disease and drugs causing such patterns of lung abnormality
CT patterns | Associated drugs |
|---|---|
Interstitial pneumonia and fibrosis (UIP or NSIP) | Methotrexate, amiodarone, carmustine, nitrofurantoin, bleomycin, busulfan, cyclophosphamide, doxorubicin, gold, penicillamine, gefitinib, sorafenib |
Eosinophilic pneumonia | Methotrexate, sulfasalazine, para-aminosalicylic acid (PAS), nitrofurantoin, nonsteroidal anti-inflammatory drugs (NSAID) |
Cryptogenic organizing pneumonia | Methotrexate, cyclophosphamide, carmustine, gold, nitrofurantoin, amiodarone, bleomycin, busulfan, erlotinib, sorafenib |
Diffuse alveolar damage | Bleomycin, busulfan, cyclophosphamide, methotrexate, amiodarone, aspirin, narcotics, gefitinib |
Hypersensitivity pneumonia | Nitrofurantoin, gefitinib, erlotinib |