IN EARLY GESTATION
 INTRODUCTION
INTRODUCTION
The prenatal diagnosis of cardiac malformations has been traditionally limited to the mid-second and third trimesters of pregnancy. The first description of a fetal cardiac anomaly at 11 weeks’ gestation occurred 20 years ago (1) and since then several studies reported on the detection of cardiac anomalies in the late first and early second trimesters of pregnancy by the transvaginal and the transabdominal ultrasound approach (2–6). The ability to image the fetal heart in early gestation with sufficient clarity to make a diagnosis of a cardiac malformation was made possible by the advent of high-resolution transvaginal and transabdominal probes (Figs. 10-1 and 10-2). The widespread adoption of first trimester risk assessment with nuchal translucency and other first trimester ultrasound markers increased interest in early fetal echocardiography. Nuchal translucency screening allowed for the detection of fetuses with chromosomal abnormalities in the first trimester with associated cardiac defects (7). Furthermore, an enlarged nuchal translucency is a risk factor for cardiac malformations (7–10).
Discrepancy exists in the literature with regard to the gestational age window, which warrants the term early fetal echocardiography. Some authors consider a targeted cardiac examination prior to 16 weeks’ gestation as early echocardiography (2), whereas others have established the nuchal translucency gestational age window of 11 to 13+6 weeks for early echocardiography (3). Nevertheless, most practitioners consider a targeted cardiac examination performed in the first and early second trimester window (10 to 16 weeks) as early fetal echocardiography (4).
Sufficient data on the efficacy of early fetal echocardiography have been mounting, and this examination is now considered an integral part of fetal cardiology in several centers with expertise in this area. In this book, we have integrated in each chapter discussing specific cardiac malformation a separate section on the detection of the abnormality in early gestation. In this chapter, we discuss basic and technical aspects related to the early fetal cardiac examination in addition to common indications and potential limitations of early fetal echocardiography.
 TRANSVAGINAL VERSUS TRANSABDOMINAL ROUTE
TRANSVAGINAL VERSUS TRANSABDOMINAL ROUTE
It is widely accepted that the transvaginal ultrasound (TVUS) examination of the fetus is superior to the transabdominal approach in early gestation as the former provides enhanced image resolution and quality. Disadvantages of the TVUS cardiac examination include the inconvenience involved in the preparation of the vaginal probe and its sterilization after the examination is completed and the added skills required by the operator (4). The tilting range of the probe is limited in TVUS and the operator should be familiar with manipulating the probe in one hand and the uterus in the other hand in order to optimize the approach to the fetal chest if needed. The most optimum fetal position is the low transverse position, which explains why the best TVUS examination is achieved before 13 weeks’ gestation (crown-rump length <70 mm), when the uterine size is still small and the fetus often lies in a transverse position. Beyond 13 weeks, the fetus commonly assumes a longitudinal position, and the approach to the heart is thus limited by the reduced depth of the high-resolution transvaginal probe. In our experience, fetal cardiac imaging performed by the TVUS approach is achievable and reliable in most cases between 12 and 13 weeks (crown-rump length 60 to 70 mm). After 13 weeks, the transabdominal route provides excellent quality with the latest transducers, assuming the fetus is examined in a dorsoposterior position.
We recommend an approach that is targeted to the gestational age, maternal body habitus, and the position of the fetus in utero. A combined transvaginal and transabdominal approach may be required in some cases.
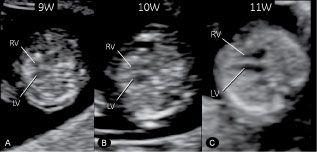
Figure 10-1. Transverse four-chamber views in three normal fetuses at 9+4 (A); 10+3 (B); and 11+2 (C) weeks’ gestation as demonstrated by transvaginal ultrasound. The lumen of right (RV) and left (LV) ventricle separated by the interventricular septum can be clearly identified by the lateral insonation. From 11 weeks’ gestation and beyond (C), the image quality under optimum conditions becomes of such clarity that reliable diagnoses can be expected.
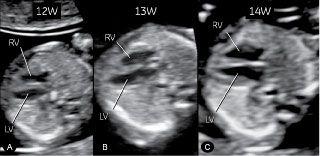
Figure 10-2. Transverse four-chamber views in three normal fetuses at 12+4 (A); 13 (B); and 14+4 (C) weeks’ gestation. Fetus at 12 (A) weeks’ gestation was examined transvaginally, while both fetuses at 13 (B) and 14 (C) weeks’ gestation were examined by high-resolution transabdominal probe (4 to 8 MHz). The switch from a transvaginal to a transabdominal approach can be achieved between 12 and 13 weeks’ gestation in most cases. LV, left ventricle; RV, right ventricle.
 CARDIAC PLANES IN GRAY SCALE AND COLOR DOPPLER
CARDIAC PLANES IN GRAY SCALE AND COLOR DOPPLER
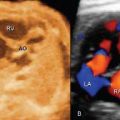
A transverse view of the fetal abdomen (Fig. 10-3) and the four-chamber view (Fig. 10-4) are reliably achieved with two-dimensional gray scale in early gestation. Abnormal cardiac anatomy at the level of the four-chamber view can be clearly demonstrated as early as 12 weeks’ gestation under optimal scanning conditions (Fig. 10-5). In many cases, the anatomic orientation of the right and left ventricular outflow tracts are not reliably seen due to their small size. By changing the insonation angle and aligning the great vessels in a transverse position, the lumen of the vessel can be better delineated (Fig. 10-6).

Figure 10-3. A: Transverse section of the upper abdomen in a normal fetus at 12+4 weeks’ gestation imaged by high-resolution transvaginal ultrasound. The stomach (St) and the descending aorta (DAO) are left-sided, while the inferior vena cava (IVC) and liver are right sided. The umbilical vein (UV) can also be identified. This plane is visualized routinely in order to exclude situs anomalies. B: Transverse section of the upper abdomen in a fetus with right isomerism at 13+2 weeks’ gestation imaged with high-resolution transabdominal scanning. The stomach (St) is right-sided, whereas the aorta (DAO), inferior vena cava (IVC), and liver are left-sided. The DAO and IVC are on the same side (called juxtaposition), suggesting the presence of situs ambiguous with right isomerism (see also Chapter 22). This fetus also had a complex cardiac defect, L, left; R, right.
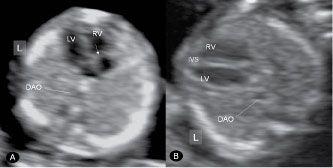
Figure 10-4. Apical (A) and axial (B) planes of the four-chamber view at 13 weeks’ gestation in two normal fetuses imaged transabdominally. Note the more apical insertion of the septal leaflet of the tricuspid valve (arrow) in A. Descending aorta (DAO) is seen in both planes and the interventricular spetum (IVS) is most optimally seen in the axial or transverse plane (B). LV, left ventricle; RV, right ventricle; L, left.
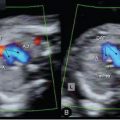
Color or high-definition power Doppler provides significant advantages in cardiac imaging in early gestation by demonstrating blood flow events in addition to flow direction. The color or high-definition power Doppler filling of an apical or basal four-chamber view separated by the septum is a good adjunct to the gray scale image. We feel that color Doppler at
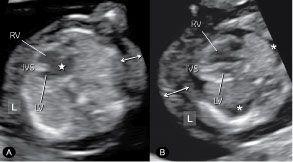
Figure 10-5. Transverse four-chamber views of two fetuses at 12 weeks’ gestation with abnormal cardiac anatomy. In fetus A, a large atrioventricular septal defect (star) is demonstrated in the center of the heart between the right (RV) and left (LV) ventricle. In fetus B, ventricular discrepancy is seen with a diminutive left ventricle (LV) in hypoplastic left heart syndrome. Note the presence of skin edema (double-sided arrow) in both fetuses and pleural effusion (asterisk) in fetus B. Fetus A had trisomy 21 and fetus B had trisomy 13. IVS, interventricular septum; L, left.
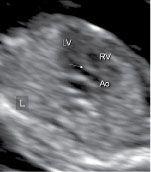
Figure 10-6. Left ventricular outflow tract in a normal fetus at 13 weeks’ gestation. Note the continuity of the medial wall of the aorta (Ao) with the ventricular septum (arrow). The lumen of the ascending aorta is best demonstrated in an insonating angle that is almost perpendicular to its course. LV, left ventricle; RV, right ventricle; L, left.
the level of the four-chamber view in early fetal echocardiography is essential in identifying normal and abnormal cardiac anatomy (Figs. 10-7 and 10-8). Color or high-definition power Doppler demonstration of the upper transverse views in the chest including the three-vessel-trachea and the transverse ductal views is, however, superior to what can be provided by the two-dimensional evaluation alone (Fig. 10-9). Aortic and ductal arches are more easily recognized in their anatomic location, size, patency, and blood flow direction. Several cardiac abnormalities involving the outflow tracts can be recognized in the three-vessel-trachea view, and a right aortic arch can also be clearly identified. Color or high-definition power Doppler is also superior to gray-scale imaging in the demonstration of aortic and ductal arches in early gestation (Fig. 10-10) and the right and left pulmonary veins draining into the left atrium (Fig. 10-11).
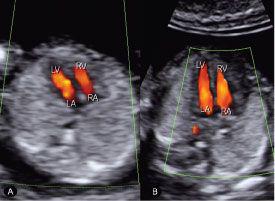
Figure 10-7. Color Doppler of an apical four-chamber view at 12 weeks’ gestation by transabdominal (A) and transvaginal (B) ultrasound examination demonstrating diastolic flow from both right (RA) and left (LA) atrium into right (RV) and left (LV) ventricle, respectively. Note that the information provided by color Doppler is very similar in both A and B with a slight superior resolution by the transvaginal approach (B). When a cardiac anomaly is suspected, additional details may be provided by the transvaginal approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree