Fig. 22.1
(a, b) Plain radiographs (anteroposterior (AP) and lateral) of the elbow do not show any evidence of injury (a, b: Published with kind permission. Copyright © Felix H. Savoie, III, MD)
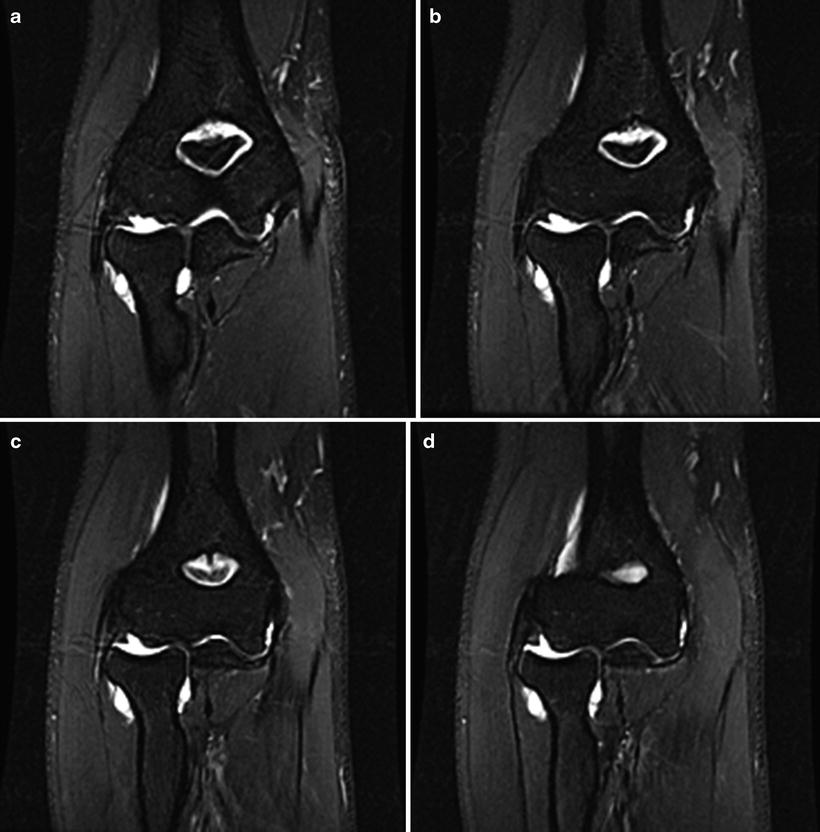
Fig. 22.2
(a–d) Coronal T2 fat-saturated images showing signal change and a small bony avulsion of the UCL from the sublime tubercle (a–d: Published with kind permission. Copyright © Felix H. Savoie, III, MD)

Fig. 22.3
(a–d) Coronal T1 images showing the small avulsion from the sublime tubercle of the ulnar insertion of the UCL (a–d: Published with kind permission. Copyright © Felix H. Savoie, III, MD)
An ulnar-sided avulsion of the MUCL from the sublime tubercle of the ulna is seen in both Figs. 22.1a, b and 22.2a–d. The fragment from the sublime tubercle measures 7 × 4 mm and has sclerotic margins indicating pathology is likely subacute. Some marrow edema can also be noted on the T2 images. The ulnar collateral ligament can still be seen inserting onto the fragment, and the remainder of the ligament demonstrates no evidence of tearing. Evaluation of the lateral collateral ligament shows no evidence of pathology. Likewise, no chondromalacia or chondral defects are seen on imaging.
Given the clinical and radiographic correlation and failure of nonoperative treatment, the risks and benefits of operative intervention were discussed with the patient and his family. The patient desired to return to his previous level of play; thus, the decision was made to proceed with elbow arthroscopy and open repair of the ulnar collateral ligament.
Operative Treatment
The patient was taken to the operating room and placed in the prone position. A standard diagnostic elbow arthroscopy was performed as seen in Fig. 22.4a–c. The radiocapitellar joint and capsule were found to be normal. The medial aspect showed evidence of instability but no signs of capsular damage. The medial gutter was found to be normal. A thickened plica was noted within the lateral gutter and was excised. The arthroscopic portion was completed.
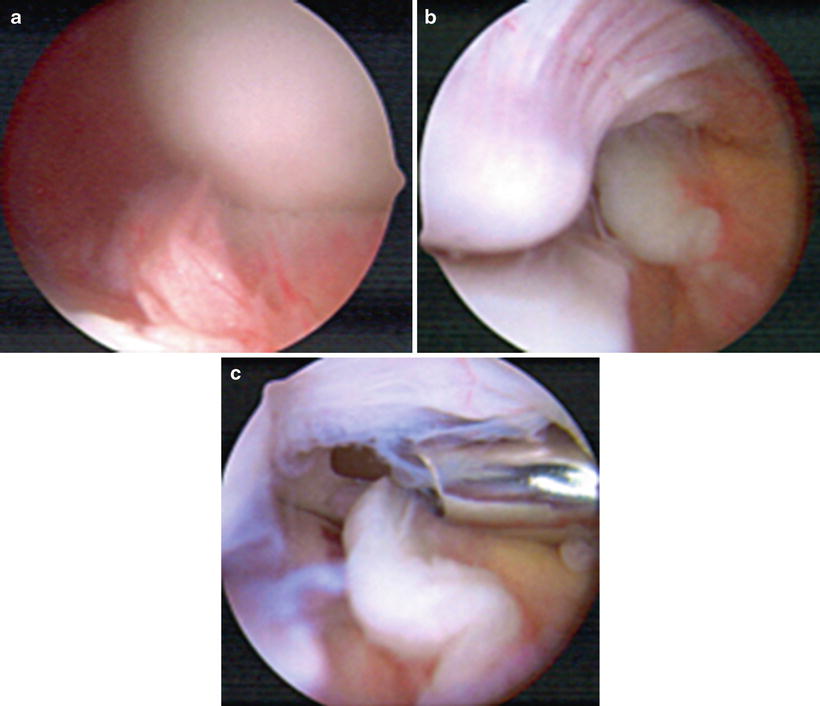
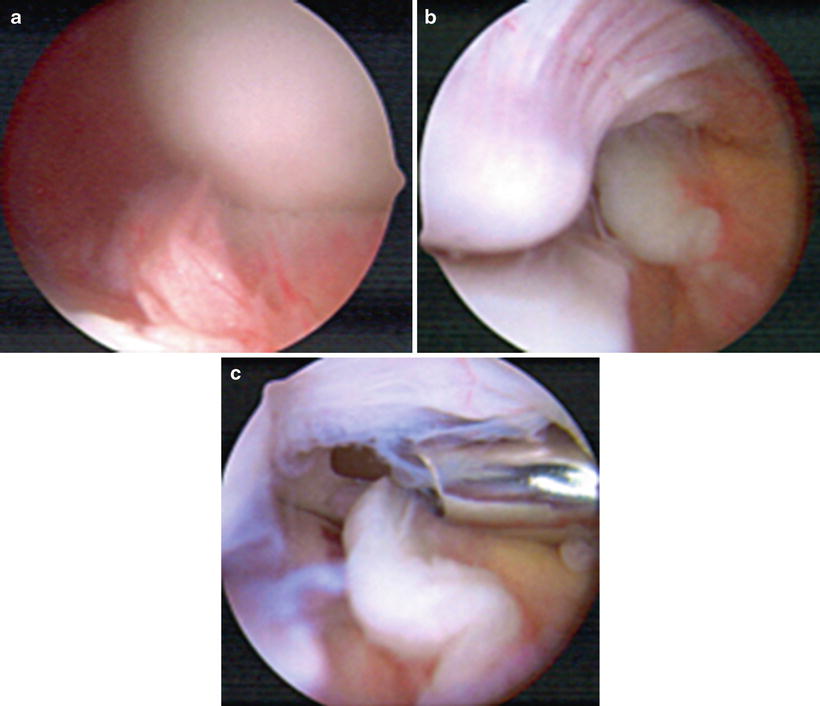
Fig. 22.4
Arthroscopic images showing the lateral gutter and synovitis (a, b), the medial gutter, and debridement of tissue in the lateral gutter (c) (a–c: Published with kind permission. Copyright © Felix H. Savoie, III, MD)
The arm was then rotated to expose the medial aspect of the elbow and the open portion of the case was completed as seen in Fig. 22.5a–d. A direct approach to the medial ulnar collateral ligament was used. A split in the flexor-pronator fascia was made posterior to the medial conjoined tendon while keeping a blunt retractor in position to protect the ulnar nerve. Upon inspection of the MUCL, the ligament itself appeared in good condition. The humeral insertion was intact; however, a small ossicle and disruption of the ulnar attachment were noted. The ligament was carefully dissected to visualize the attachment site on the sublime tubercle. The small ossicle was excised, and the bony footprint was roughened to improve healing of the ligament. A double-loaded suture anchor was placed at the footprint. Two limbs of the anchor were placed through the more posterior aspect of the ligament, while the remaining two limbs were placed through the anterior aspect. The two strands were then tied, securing the MUCL to its footprint. A #1 Vicryl was then used to plicate the midportion of the tendon. The elbow was tested and found to be stable. The incision was then irrigated and closed in standard fashion.
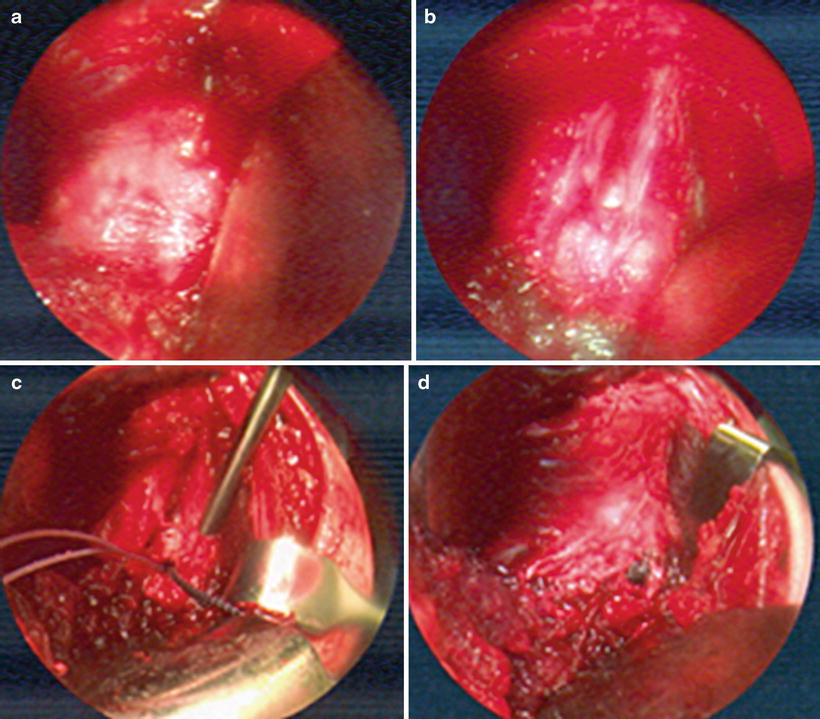
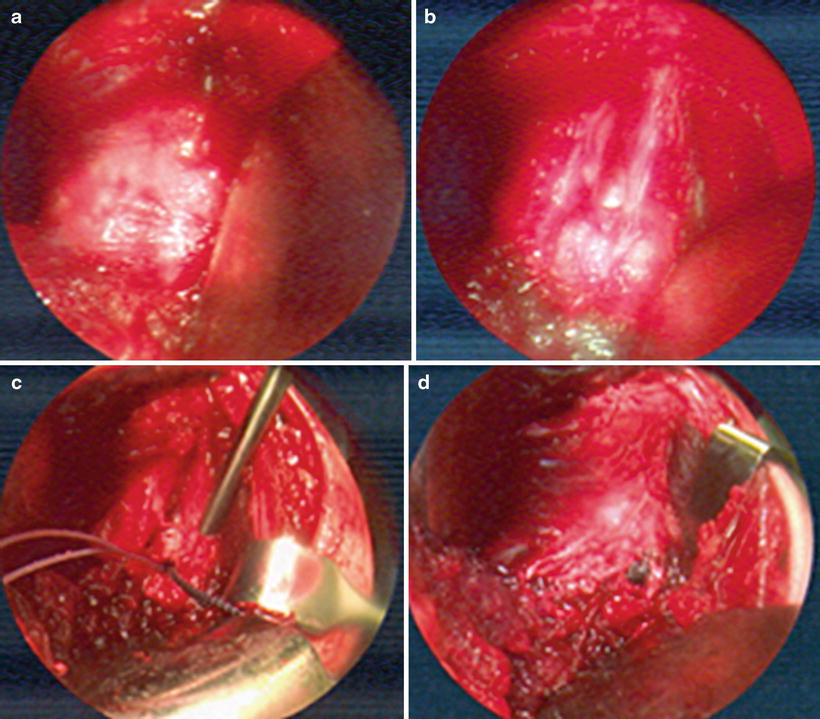
Fig. 22.5
Images of the open portion of the procedure showing (a) the intact mid-substance of the MUCL. (b) Again a preserved mid-substance of the ligament with avulsion of the ulnar aspect. (c) Suture anchor placement into the sublime tubercle. (d) Completed repair of the distal MUCL to the sublime tubercle (a–d: Published with kind permission. Copyright © Felix H. Savoie, III, MD)
MRI Case 2: MUCL Tear
History/Exam
A 19-year-old, right-hand-dominant pitcher injured his elbow while pitching. Despite initial activity modification and therapy, he was unable to return to play due to pain and dysfunction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








