Alya Sheikh, MD
The elbow joint is a hinge joint with a loose capsule and collateral ligaments. The capsule is situated along the anterior and posterior aspect of the joint, preventing flexion–extension movements, whereas the collateral ligaments prevent medial and lateral movements. The articulating bones include the distal humerus, proximal radius, and ulna. The medial humeral condyle, also known as the trochlea, articulates with the upper end of the ulna known as the coronoid process. The humeroradial part of the joint consists of the capitellum (distal humerus) and head of the radius.
The elbow joint is often subject to overuse injuries. Partial or complete tears of tendons such as the biceps tendon are not infrequent and are often an indication of magnetic resonance imaging (MRI) study. Nerve entrapment syndromes around the elbow are often diagnosed clinically and MRI is usually indicated to rule out a lesion that could be within the nerve or causing compression of the nerve. In this chapter, we will discuss some of the common conditions affecting the elbow joint.
IMAGING PROTOCOL
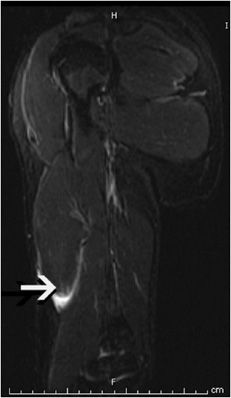
All imaging should start with radiographs, including anteroposterior and lateral views of the elbow joint (Figure 15-1). While a bony injury might be evident on these views, when no obvious fracture line or misalignment is noticeable, one has to look at the soft tissues to see if there are secondary signs of insult, such as a “sail sign.” This is a triangular density of fat lifted into the field of view by the effusion in the elbow joint (Figure 15-2). There is controversy as to whether an anterior or posterior sail sign is more important. Any sign of a joint effusion, whether anterior or posterior, merits further investigation.
Figure 15-1. Normal elbow. Lateral radiograph of the elbow. Note anterior stripe of fat is adjacent to the distal humerus.
Figure 15-2. Sail sign. The fat overlying the joint capsule is lifted off due to distension of the joint capsule by joint effusion and appears as a triangular hypodensity proximal to the joint line (arrow).
In our institution, we routinely perform the following MR sequences: coronal T1-weighted, coronal short tau inversion recovery (STIR), axial T1-weighted, axial T2-weighted fat-suppressed, sagittal proton density (PD) weighted fat-suppressed, and sagittal T2-weighted sequences. Further sequences are tailored according to what is seen on initial imaging, and the benefits of using gadolinium (Gd) are weighed against the risks. If an ultrasound-guided biopsy is under consideration we require a Gd-enhanced T1-weighted fat-suppressed sequence to see if enough synovial tissue is visualized to merit an ultrasound-guided biopsy.
EPICONDYLITIS
Pain at the origin of common flexor or extensor group of tendons is usually termed epicondylitis. Even though the pain is directly related to microtears of the tendon origins, an inflammatory component at the level of the epicondyle has not been demonstrated. The lateral-sided pain is commonly referred to as Tennis Elbow, while the one on the medial side is termed Golfers Elbow. The diagnosis is usually clinical but MRI can be used as an adjunct to confirm the suspected diagnosis. The coronal sequences are most useful as they show both medial and lateral tendons in a single view. When diseased, the affected tendons exhibit mixed signal on T1-weighted sequences and increased signal on T2-weighted sequences. The intensity of the signal on fluid-sensitive sequences varies with the degree of microtears. In partial tears, it is hyperintense to the adjacent muscles. In full-thickness tears, the site of injury might show a very high signal consistent with fluid and hemorrhage at the origin site (Figure 15-3). Other secondary signs like periosteal reaction at the epicondyles, or edema in the anconeus muscle, have been described but seem to be extremely rare in day-to-day practice.1
Figure 15-3. Lateral collateral ligament (LCL). In this T1-weighted coronal image, the white arrow points to a relatively thickened LCL with some surrounding edema. This image demonstrates the normal location of LCL.
MEDIAL AND LATERAL COLLATERAL LIGAMENT TEARS
These are usually sports-related injuries and become important to diagnose as part of the workup for medial or lateral elbow pain. There are three parts of the medial collateral ligament (MCL): anterior, medial, and lateral. Injuries of the anterior band of the MCL are common. The thicker anterior bundle of the MCL is seen as a hypointense linear signal on all coronal-oriented pulse sequences (Figure 15-3). The proximal portion of the MCL may show high signal due to synovial invagination and should not be mistaken for a tear. Most injuries occur in the mid-substance during excessive valgus stress.1 Partial tears are more common and usually not too difficult to diagnose on fluid-sensitive sequences on MRI (Figure 15-3). These tears are often diagnosed when joint fluid or contrast (in case of MR arthrogram) extends below the joint line and reaches the sublime tubercle; this finding on MRI is referred to as the “T- sign” (Figure 15-4). The sublime tubercle is the medial aspect of the ulnar coronoid process where the anterior band of the MCL attaches.
Figure 15-4. Tear of the common flexor tendons origin with UCL avulsion-related T-sign. T2-weighted fat-saturated image in coronal plane demonstrates increased signal and partial disruption of the common flexor tendons at their origin (arrow). Also notice the T-sign created by fluid seeping between the ulnar collateral ligament (UCL) and the sublime tubercle due to partial avulsion of the UCL.
Chronic partial tears are seen as thickening or thinning of the ligament, which may or may not be associated with signal changes (Figures 15-3 to 15-6). Tears of the MCL can be associated with medial epicondylitis, ulnar neuropathy, or posteromedial olecranon impingement.2,3 The medial and lateral portions of the MCL are difficult to visualize on MRI and beyond the scope of this chapter.
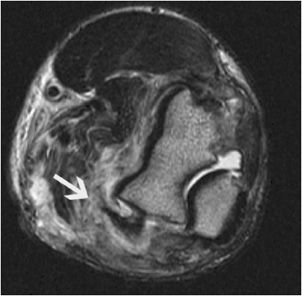
Figure 15-5. Partial tear of the common flexor tendons. Axial T2-weighted image demonstrates edema around the partially torn common flexor tendons (arrow) as well as in the medial group of muscles.
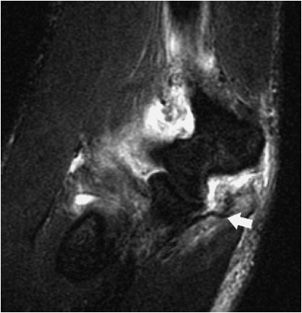
Figure 15-6. Avulsion of UCL. T2-weighted fat-suppressed coronal image shows a joint effusion as well as avulsion of the UCL (arrow).
The lateral collateral ligament (LCL) contains a number of structures; the most important, from an imaging point of is therefore presumed to be more susceptible to injury.6 It is also theorized that mechanical impingement of the tendon in the radioulnar space during pronation and bicipital tuberosity enthesophytosis contributes to an increased risk of tears.4–6
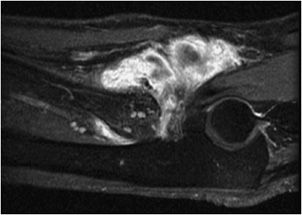
Patients with complete tears often complain of acute pain in the antecubital fossa, swelling, and ecchymosis. These signs and symptoms can sometimes be accompanied by an audible pop and palpable bump in the mid-distal or proximal arm corresponding to the retracted biceps brachii muscle (Figures 15-10B, and 15-12).4 Complete tears without retraction and partial tears may have a less dramatic presentation, and sometimes the diagnosis of chronic distal tendon tears may even be missed or delayed (Figures 15-13 to 15-15).7 The differential diagnosis for pain in the antecubital fossa includes partial tear of the distal biceps tendon, cubital bursitis, bicipital tendinosis, lateral antebrachial cutaneous nerve entrapment, and posterior interosseous nerve syndrome.4
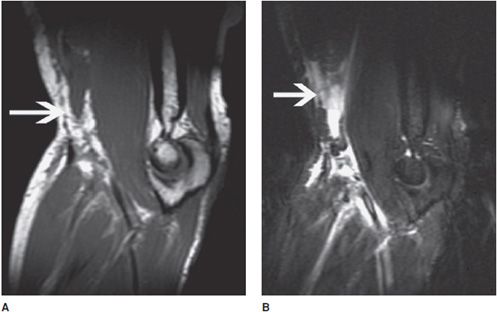
If the diagnosis of a distal biceps tendon rupture is uncertain clinically, MRI of the elbow is often obtained. One study by Festa, et al. demonstrated that although MRI is very sensitive in diagnosing complete tears, it is significantly less sensitive in diagnosis of partial tears.7 However, the overall sensitivity and specificity of MRI in detecting distal biceps tendon tears are 92.4% and 100%, respectively.7 To better view, is the lateral ulnar collateral ligament (LUCL). It is usually seen as a hypointense linear band extending from the radial to the ulnar side on the most posterior series of coronal MRI images (Figures 15-7 and 15-8).
Figure 15-7. Lateral ulnar collateral ligament (LUCL). The arrow on this coronal T2-weighted fat-suppressed image points to a normal LUCL seen as a hypointense structure coursing posteriorly from lateral to medial side.
Figure 15-8. LUCL edema. The arrow on this T2-weighted fat-saturated coronal image demonstrates edema around the LUCL, suggestive of a sprain or partial tear. (C) Fluid-sensitive MRI demonstrates capitellar edema as increased signal along with fragmentation of the capitellum.
BICEPS TENDON TEAR
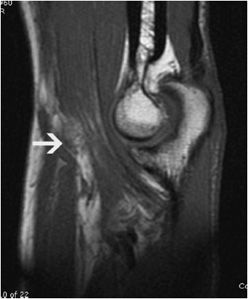
Biceps tendon injuries usually involve the proximal aspect of the tendon at the level of the shoulder. Ruptures of the distal biceps tendon account for only 3% of all biceps tendon injuries.4 Distal biceps tendon tears usually affect men between the ages of 30 and 60 years, with the injury most often affecting their dominant arm.5 The incidence of distal biceps tendon tears is estimated to be 1.2 per 100,000 patients based on a 2002 demographic study.4,5 Smoking and steroid use may increase the risk of rupture. The injury occurs when an extending force of 40 kg or greater is applied on a flexed and supinated forearm.6 The normal biceps insertion can be appreciated on sagittal T1-weighted or axial images as hypointense structures that insert on both radial and ulnar sides in the antecubital fossa (Figures 15-9A,B, and 15-14). Acute trauma of this nature can lead to tears of the tendon approximately 2 cm above its attachment (Figures 15-10A,B and 15-11).4,6 This point is considered the hypovascular zone and visualize the full length of the distal biceps tendon, Giuffre and Moss innovated the FABS (flexed elbow, abducted shoulder, supinated forearm) view in 2004. To obtain this image, the patient is prone in the scanner with the arm overhead, elbow flexed to 90n, and forearm in supination.6,7 In complete distal biceps tendon ruptures MRI findings include discontinuity and increased diameter of the torn tendon, tendon retraction, fluid-filled tendon sheath, and edema or increased T2 signal in the biceps muscle and surrounding soft tissues. One may also see edema in the area of the bicipital tuberosity and bicipitoradial bursitis (Figure 15-16).6,7 A caveat to keep in mind is that the proximal portion of the tendon and muscle may not be retracted when the overlying aponeurosis known as the lacertus fibrosus is intact.3 For partial tears, MRI findings include change in tendon caliber (usually thickened), abnormal tendon contour and internal signal, edema or increased T2 signal at the radial tuberosity, and increased fluid signal in the tendon sheath.6,7
Figure 15-9. Normal biceps tendon. (A,B) On sagittal T1-weighted images, biceps tendon is seen as a hypointense structure (arrow) anterior to the brachialis tendon. One may need to scroll through the images to see the full tendon.
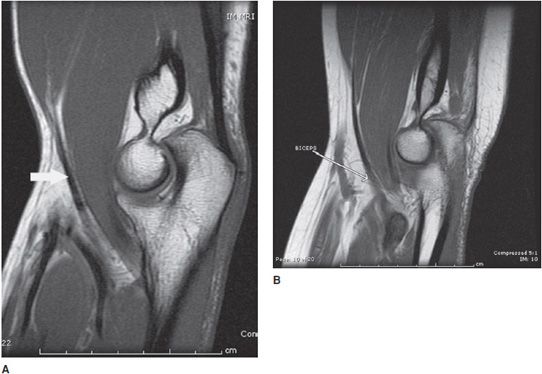
Figure 15-10. Biceps brachialis tear. (A) Sagittal T1-weighted image shows a tear of the biceps tendon. The hypointense tendon is not seen in its entire course and the retracted biceps muscle is seen above the antecubital fossa (arrow). Note the surrounding normally bright fat has stranding due to edema. (B) Sagittal T2-weighted fat-saturated image shows the retracted biceps muscle surrounded by edema and hemorrhage (arrow).
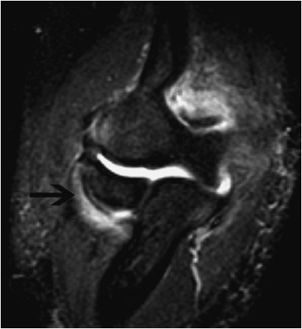
Figure 15-11. Biceps partial tear. T1-weighted sagittal image with partial tear of the biceps (arrow) tendon. Note the relative lack of muscle belly retraction.
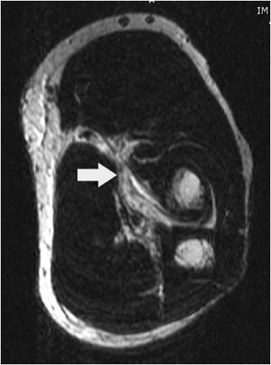
Figure 15-12. Biceps tear with retraction. Sagittal proton density sequence shows retraction of the torn biceps tendon (white arrow) with edema and hemorrhage in the musculotendinous junction.
Figure 15-13. Biceps distal insertion tear. Axial PD image showing a tear of the distal insertion of the biceps tendon (arrow). No hypointense linear structure is seen where the arrow points, indicating distal insertion tear.
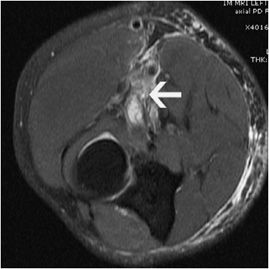
Figure 15-14. Distal biceps tear. Axial PD-weighted image with fat-suppressed shows fluid near the expected site of biceps tendons, indicating distal biceps tendon tear (arrow).
Figure 15-15. Torn biceps retraction. T2-weighted coronal image showing a retracted biceps tendon (arrow) at the mid-arm level.
Figure 15-16. Biceps bursitis. Contrast-enhanced T1-weighted fat-suppressed sagittal plane image shows intense contrast enhancement in the antecubital fossa surrounding the biceps tendon. (Image from reference no.22)
The treatment varies between occupational therapy/rehabilitation to surgery depending on the individual patient’s clinical presentation and needs. For complete avulsion of the distal biceps tendon, especially in young active patients or athletes, the treatment of choice is anatomic surgical repair.7 Partial tears are usually treated conservatively with analgesics, though sometimes surgery may be necessary if symptoms persist or there is significant loss of strength and function.6 Proximal tears are usually diagnosed after clinical symptoms and signs as an absence of the long head of biceps in the bicipital groove on axial T2-weighted images, usually during shoulder MRIs.
TRICEPS TEARS
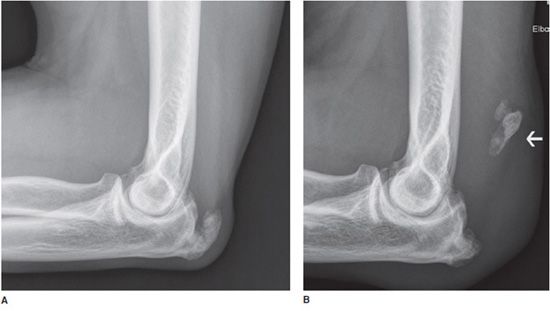
Distal triceps tendon tears are considered rare, accounting for less than 1% of all upper extremity tendon-related injuries.8 However, a retrospective study of consecutive elbow MRIs by Koplas, et al. indicated a greater prevalence of 3.8% for distal triceps tendon injuries.9 Mechanism of injury is usually forced elbow flexion against the contracted triceps. It can occur from a fall on an outstretched hand or direct trauma to the posterior elbow. Normal triceps inserts on the olecranon and sometimes enthesophytes can be seen at the insertion site (Figure 15-17A,B). Athletes such as football players, especially lineman, and weightlifters are susceptible to this among other elbow-related injuries.9 Predisposing systemic illnesses include secondary hyperparathyroidism associated with renal failure, rheumatoid arthritis, osteogenesis imperfecta, anabolic steroids, and reportedly insulin-dependent diabetes, among others.8 Local steroid injections and olecranon bursitis may also be associated with distal triceps tendon tears.8
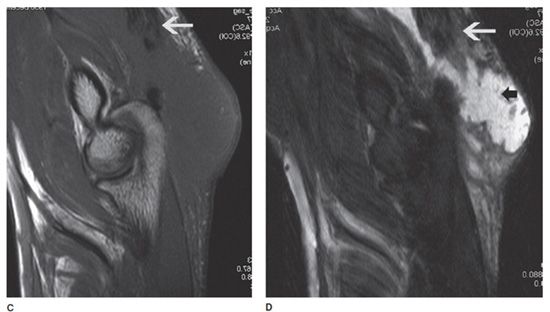
Figure 15-17. Triceps avulsion fracture. (A) Lateral radiograph shows an enthesophyte at the triceps insertion on the olecranon. (B) Lateral radiograph in same patient shows triceps avulsion fracture of the enthesophyte (arrow) that has migrated proximally with the muscle belly. (C and D) Sagittal T1-weighted and T2-weighted MRIs in same patient demonstrate triceps tear (white arrows) and hematoma (small black arrow in D).
With acute distal triceps tendon rupture symptoms include pain, swelling, ecchymosis, and reduced range of motion. On clinical exam, one might find a palpable defect in the area of the torn tendon, though, if there is significant swelling this can be difficult to assess. Elbow extension against gravity is also difficult.8
Radiographs may on occasion demonstrate a tiny avulsed fracture fragment off the olecranon (Figures 15-17B–D). Rarely, a large avulsed fracture fragment of the olecranon may be seen.8
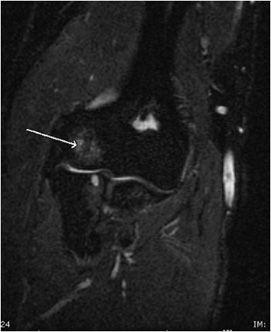
MRI of the elbow has proved useful in evaluating the extent of injury involving the tendons, while simultaneously allowing the clinician to assess for other potential causes of pain in cases when the clinical diagnosis is in question, and lastly, as a preoperative planning tool for cases that may require surgical intervention. Axial and sagittal T2-weighted MR images are helpful, though the tendon is best visualized in the sagittal plane.2,10 Most commonly, the tendon will tear at or near its attachment site to the olecranon (Figures 15-17C,D). Intrasubstance and musculotendinous junction tears are less common.9 Partial tears are seen as small focal regions of discontinuity manifesting as increased T2-weighted signal in the tendon and adjacent soft tissues, with some tendon fibers remaining intact. A large fluid-filled defect in the distal tendon with tendon retraction indicates a full-thickness tear.2 Increased T2-weighted signal or edema can be seen in the surrounding soft tissues, triceps muscle, and occasionally in the olecranon. Other associated findings may include olecranon bursitis, elbow joint effusion, and possibly a radial head fracture.9
Surgical anatomic reattachment of the tendon to the olecranon is the recommended treatment of complete ruptures. Conservative management of partial tears is acceptable, although in cases where patients have persistent weakness, surgery may be considered.8,11
PANNER DISEASE
Osteochondrosis of the capitellum, also known as Panner or Panners disease, is rare and occurs mostly in boys between the ages of 5 and 10 years. As it is commonly seen in young baseball pitchers, it is also referred to as Little Leaguers elbow, a term that ideally should be reserved to describe medial epicondylar apophysitis specifically, as discussed in the next section. Panner disease is differentiated from osteochondritis dissecans (OCD) based primarily on age, with the latter occurring mostly in adolescents or adults when the capitellum is completely ossified.12 However, these two entities may be considered stages of the same process, with OCD reflecting the later phase of disease. The etiology is uncertain, but repetitive injury secondary to lateral impaction forces and a relatively poor blood supply may contribute to the development of this disease. Panner disease results in osteochondrosis of the capitellum, which can be seen radiographically (Figure 15-18A).13 One may also see increased sclerosis, collapse, and eventual reossification with restoration of the original bony contour if aggravating forces are removed.12 However, it does not result in formation of a loose body, in contrast to OCD.
Figure 15-18. Panner disease. (A) AP radiograph of elbow shows hypodensity (arrow) at the capitellum. (B) T1-weighted coronal image of elbow shows decreased marrow signal due to edema and capitellar fragmentation (loss of smooth capitellar contours). (C) Fluid-sensitive MRI demonstrates capitellar edema as increased signal along with fragmentation of the capitellum.
Patients present with pain, stiffness, and decreased range of motion, but often recover fully with little to no residual disease with conservative medical management.
MRI generally reveals diffuse abnormal signal in the capitellum (Figures 15-18B,C). Additional findings of bone fragmentation, cystic changes, cartilaginous defects, and loose bodies may be seen with OCD.14 Elbow contusions are not confined to capitellum and usually involve adjacent bones around the articular surface, corresponding to bone bruises (Figure 15-19).
Figure 15-19. Elbow contusions. Coronal plane fluid-sensitive MRI image shows increased signal in the capitellum (arrow) and cystic changes in the radial head due to posttraumatic or osteoarthritic changes.
LITTLE LEAGUERS ELBOW
Little Leaguers elbow was a term originally coined by Brogdon and Crow in 1960 to describe separation and fragmentation of the medial epicondylar apophysis of the elbow in adolescent pitchers.15,16 In young throwing athletes, the repetitive medial tensile stresses on the medial epicondyle, as well as the pull of the flexor–pronator muscle group, and medial UCL during the acceleration phase of throwing leads to microtrauma of the UCL and epiphysis. The anterior band of the UCL as previously mentioned is the most important in that it provides the most restraint to the valgus stress placed on the joint during throwing.
In adults, the sequelae of ongoing valgus stresses of throwing include degeneration, microtears, or rupture of the UCL, but in adolescents it is the immature apophysis of the medial epicondyle that bears the brunt of these valgus stresses.16
These patients generally complain of medial elbow and proximal forearm pain during throwing, and initially the pain improves with rest. However, as the disease progresses the pain may become continuous with loss of velocity, distance, and throwing effectiveness.16,17 Radiographs may demonstrate widening at the epiphysis, separation, fragmentation, and hypertrophy of the medial epicondyle. One study showed that up to 63% of young pitchers had pain at the medial epicondyle, with approximately 70% of these throwers having evidence of separation and 40% demonstrating fragmentation.17,18
As there is wide variety of injuries that would manifest with medial elbow pain, MRI becomes necessary to help determine the exact cause of the symptoms and to tailor the treatment accordingly. Generally, MRI shows evidence of marrow edema within and deep to the medial epicondylar apophysis, manifesting as high signal on T2-weighted imaging.
Often the term Little Leaguers elbow is used as an umbrella term for a variety of associated findings that may also be present on MRI, including complete tears or avulsions of the UCL, flexor–pronator strains, and proximal ulna stress fractures, as well as lateral compartment injuries including Panner disease and OCD of the capitellum, among others.16,17
OLECRANON BURSITIS
A bursa is a synovial lined flattened sac filled with trace fluid located between adjacent structures, such as tendon and bone, and helps reduce friction between them during movement. The olecranon bursa is located in the subcutaneous tissues just posterior to the olecranon, and is the most commonly affected bursa in the elbow.
Olecranon bursitis is a clinical diagnosis, with MRI being performed only rarely when there is clinical concern for an underlying abscess or osteomyelitis.19 However, olecranon bursitis is often incidentally diagnosed on MRI due to secondary inflammation and fluid in the bursa related to trauma or a variety of other inflammatory conditions for which the MRI initially was ordered.19,20
Because of its superficial location, it is susceptible to overuse or direct trauma with resultant nonseptic bursitis, also known as coal miners elbow or student elbow. It has also been seen in football players playing on artificial turf. Besides trauma, other etiologies include infection, rheumatoid arthritis, and gout. Tophi can be seen as soft tissue swelling with calcifications depending on time since diagnosis (Figure 15-20A). Other causes include chondrocalcinosis, hydroxyapatite crystal deposition, and obesity.17,20 It can also be seen in patients with uremia as well as those on hemodialysis.
Figure 15-20. Olecranon bursitis. (A) Lateral radiograph of the elbow in a patient with gout. There is soft tissue swelling over the olecranon as well as calcifications of the tophi (arrow). Noncalcified tophi are also seen as soft tissue masses in the subcutaneous fat. (B) Sagittal plane T1-weighted MRI demonstrating decreased signal in the bursa due to fluid accumulation. Interspersed in the bursa are foci of signal loss (seen as signal hypointense to the muscle signal) caused by calcifications (arrow). Protons in the calcified areas remain immobile causing a signal drop in all sequences. (C) T2-weighted fat-suppressed image shows lack of signal due to calcifications (arrow) and mixed signal in the bursa. The mixed signal is reflective of the complex nature of the fluid with urate crystals.
Approximately one-third of olecranon bursitis cases are due to infection, most commonly Staphylococcus aureus. Up to half of all septic cases are secondary to reduced immunity most commonly due to alcohol abuse, but also steroids, diabetes, renal insufficiency, and malignancy.17,20 Fever, tenderness, and regional cellulitis are common with septic bursitis, though these findings are nonspecific.17 Clinical differentiation between aseptic and septic bursitis can be challenging, and aspiration of the bursal fluid is important in making the diagnosis.17,20
Axial and sagittal T2-weighted MR images are helpful in diagnosing olecranon bursitis.21 MRI findings include a collection over the olecranon that is hypointense on T1 with variable signal on T2-weighted images (Figures 15-20B,C). Associated findings commonly include soft tissue edema with contrast enhancement, as well as enhancement of the bursal wall. These findings can be seen with both septic and aseptic bursitis, though septic olecranon bursitis can be excluded if there is no bursal or soft tissue enhancement20 (Figure 15-21).
Figure 15-21. Elbow inflammation with synovium enhancement. A contrast-enhanced T1-weighted image with fat suppression shows synovial enhancement (arrow) that reflects synovitis due to inflammation or infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree