Marcia F. Blacksin, MD
SHOULDER
The shoulder girdle consists of the clavicle, scapula, and humerus. It connects the upper extremity to the axial skeleton with only one true joint, the sternoclavicular joint. Between the scapula and the thorax, there is a muscular connection, allowing for extended mobility, compared to the limited mobility of the pelvic girdle. The joints of the shoulder girdle are the glenohumeral or shoulder joint, the acromioclavicular (AC) joint, and the sternoclavicular joint. The scapula is a complex bone and serves as a muscle attachment site. Seventeen muscles surround the scapula, supporting movement and stabilizing the shoulder. The scapula extends from the second to the seventh rib and has 30° anterior tilt. Scapular fractures (Figure 2-1) are relatively uncommon. They require high-energy and associated injuries, such as other fractures, pulmonary contusions, pneumothorax, neurovascular injuries, and spine injuries, which occur in 35–98% of patients.1,2
Figure 2-1. Scapular neck fracture. There is a minimally displaced fracture of the scapular neck (arrow), with hairline extension into the scapular body. No extension to the glenoid surface is seen. Note that this patient is skeletally immature; the proximal humeral physis is patent.
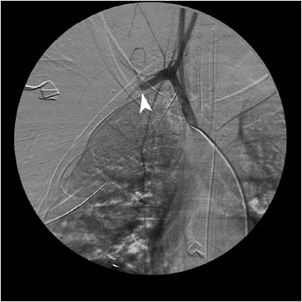
Scapulothoracic dissociation (Figure 2-2) is a rare entity that consists of disruption of the scapulothoracic articulation. It is in essence an internal forequarter amputation. Vascular disruption (Figure 2-3) and brachial plexus injuries are usually present. Clinically, patients have massive soft tissue swelling, a pulseless upper extremity, and complete or partial neurologic deficits. Radiographically, there is lateral displacement of the scapula, AC separation, displaced clavicle fracture, or sternoclavicular disruption. These devastating injuries require violent traction and rotation, usually seen in motorcycle or motor vehicle accidents.3 There is a high mortality rate. Survivors with complete brachial plexus injuries suffer from flail upper extremity.
Figure 2-2. Scapulothoracic dissociation. The medial scapula border is laterally displaced with respect to the rib cage (arrowheads). The acromioclavicular joint is disrupted (double-headed arrow).
Figure 2-3. Angiogram, scapulothoracic dissociation. Same patient as in Figure 2-2. A catheter is placed in the brachiocephalic trunk. Contrast is opacifying the proximal aspect of the right subclavian artery with abrupt cutoff of the vessel, due to disruption (arrowhead).
The clavicle serves as a rigid support from which the scapula and arm are suspended. It keeps the upper limb away from the thorax so that the arm has maximum range of movement and transmits physical impacts from the upper limb to the axial skeleton. It also protects the neurovascular bundle and lung apices. Clavicle fractures are usually caused by a fall onto the affected shoulder. Eighty percent of fractures occur in the midshaft region (Figure 2-4) and only about 2% in the medial clavicle.4 The remainder occurs in the distal third, where the coracoclavicular ligaments may be injured. Clavicle fractures can be associated with other fractures, most commonly rib fractures, brachial plexus injuries, and pneumo-/hemothorax.5
Figure 2-4. Midshaft clavicle fracture. The oblique fracture (arrows) is distracted and the distal fracture fragment is inferiorly displaced by about one shaft’s width.
The AC joint is the articulation between the acromion process of the scapula and the distal end of the clavicle. It is a diarthrodial and synovial joint. The acromion of the scapula rotates on the distal end of the clavicle. The most common mechanism of injury in AC joint separation is direct trauma to the proximal shoulder, such as in contact sports. Stability of the AC joint is maintained by the AC ligaments in the axial plane. Craniocaudal stability is achieved by the coracoclavicular ligaments. AC joint injuries (Figure 2-5) are classified into six groups, ranging from minor sprains only detectable with a comparison stress view to gross deformities of the AC joint with AC ligament and coracoclavicular ligament disruption. The average coracoclavicular distance is 1.1–1.3 cm. Detailed classification can be found in any standard radiology textbook.
Figure 2-5. Acromioclavicular joint separation. There is malalignment between the distal end of the clavicle and the acromion process (arrowheads). Note also the increased distance between the clavicle and the coracoid process.
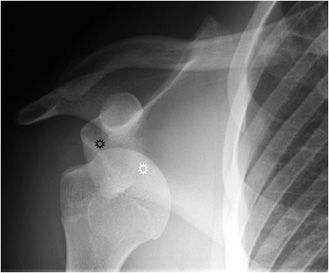
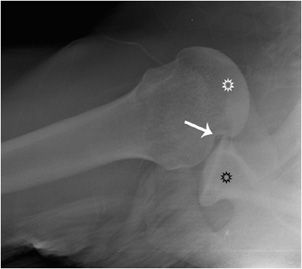
The shoulder joint is a ball and socket joint. Its stability is provided by the bony anatomy of the glenoid fossa, the coracoid, and acromion processes. The rotator cuff muscles and long head biceps muscles provide muscular restraints, whereas the glenohumeral ligaments, glenoid labra, and joint capsule also contribute to stability. Nonetheless, the shoulder joint is the most commonly dislocated major joint in the body. About 95% of shoulder dislocations are anterior dislocations (Figure 2-6). The humeral head is displaced anteriorly and inferiorly to the glenoid, in subcoracoid position. There may be a resultant impaction fracture at the posterior, superior, and lateral aspect of the humeral head, a so-called Hill–Sachs lesion (Figure 2-7). At the anterior– inferior aspect of the glenoid, a fracture may be seen on radiograph, a so-called “bony Bankart” lesion. Both lesions are best seen on postreduction films. Non-bony Bankart lesions are best evaluated with MR arthrography. An engaging Hill–Sachs lesion is defined as a defect in the humeral head large enough that the edge drops over the glenoid rim when the arm is externally rotated.6 This represents an indication for surgery, as are lesions representing more than 30% of the articular surface (determined on pre-op CT). The most common complication after anterior shoulder dislocation is a recurrent dislocation, due to damage of the stabilizing structures.
Figure 2-6. Anterior shoulder dislocation. The humeral head (white star) is displaced inferiorly and medially to the glenoid (black star) and sits inferior to the coracoid process.
Figure 2-7. Anterior shoulder dislocation. This axillary view demonstrates the humeral head (white star) being displaced anteriorly and medially to the glenoid (black star). The Hill–Sachs impaction fracture is marked with an arrow.
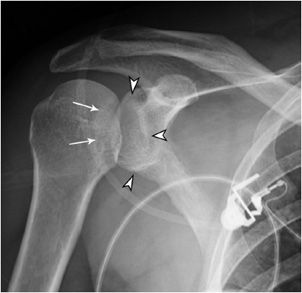
Posterior shoulder dislocations (Figure 2-8) represent about 4% of shoulder dislocations. Frequently, they are unrecognized by primary care or emergency room physicians, but are also missed radiographically in more than 50% of cases.7 Trauma or convulsive seizures can result in posterior dislocations. The average age of patients with traumatic posterior dislocation is 50 years. Patients present with history of trauma, pain, and inability to externally rotate the arm. Complications include associated fractures (glenoid rim and proximal humerus) and injury to the neurovascular bundle, especially the axillary nerve.
Figure 2-8. Posterior shoulder dislocation. The humeral head is locked in internal rotation, but typically at the same level as the glenoid (arrowheads), which makes the dislocation difficult to recognize. A trough sign is seen (arrows), representing an impaction fracture of the humeral head, also called a reverse Hill–Sachs lesion.
An inferior dislocation of the shoulder (Figure 2-9) is also called “luxatio erecta,” as the arm is locked in a forwardly elevated position. This is caused by a severe hyperabduction injury, where the humeral neck impinges against the acromion, which levers the humeral head inferiorly. There is a high rate of associated neurovascular injuries, involving the brachial plexus and axillary artery.8
Figure 2-9. Inferior shoulder dislocation. The humeral head (star) is wedged against the inferior glenoid (arrow). There is an associated displaced greater tuberosity fracture (arrowhead).
ELBOW
Radial head (Figure 2-10) or neck fractures (Figure 2-11) often occur as the result of a fall on an outstretched arm with the distal forearm angled laterally, valgus stress on the elbow, or from a direct blow to the elbow, such as with a motor vehicle accident. The elbow is a complex joint due to its intricate functional anatomy. The ulna, radius, and humerus form four distinctive joints, which are stabilized by the ulnar collateral ligament complex, the lateral collateral ligament complex, and the joint capsule. Motion is facilitated by four muscle groups: the elbow flexors, the elbow extensors, the flexor–pronator group, and the extensor–supinator group. The most commonly used classification system for both treatment and prognosis assessing radial head or neck fractures is the Mason classification (Table 2-1).
Figure 2-10. Radial head fracture. There is a nondisplaced, minimally comminuted fracture through the radial head (arrow), without gapping or step-off at the articular surface.

Figure 2-11. Radial neck fracture (A,B). There is a slightly impacted fracture through the radial neck (arrows), resulting in a sclerotic line across the radial neck. There is a sharp angle at the radial head/neck junction, which is not seen in a normal neck (compare with Figure 2-10).
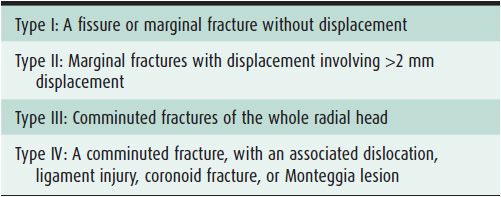
Table 2-1. Mason Classification for Radial Head and Neck Fractures
WRIST
The Galeazzi fracture–dislocation (Figure 2-12) is a radial shaft fracture with associated dislocation of the distal radio-ulnar joint (DRUJ). There may be associated compartment syndrome. Anterior interosseous nerve (AIN) palsy may also occur, but it is easy to overlook, as the AIN is a pure motor nerve, and therefore there is no sensory deficits. Injury to the AIN can cause paralysis of the flexor pollicis longus and flexor digitorum profundus muscles to the index finger, resulting in loss of the pinch mechanism between the thumb and the index finger. Galeazzi fractures are sometimes associated with wrist drop due to injury to radial nerve, extensor tendons, or muscles. They are the most likely fractures to result in malunion.
Figure 2-12. Galeazzi fracture-dislocation. (A) The forearm film demonstrates an oblique fracture through the distal radial shaft (arrow). There also is a torus fracture of the distal ulnar shaft (arrowhead). (B) The wrist film demonstrates marked ulnar angulation of the distal radial shaft fracture (arrow). The ulnar head is dislocated from the distal radioulnar joint (arrowhead) and there is a mildly displaced fracture of the ulnar styloid.
The term Colles fracture (Figure 2-13) is used for any fracture of the distal radius, with or without involvement of the ulna that has dorsal displacement of the fracture fragments. It typically occurs in the metaphysis. The mechanism of injury is falling on an outstretched arm with the wrist dorsiflexed, resulting in a characteristic “dinner fork” or “bayonet” like deformity. Colles fractures are commonly seen in osteoporotic patients. It is important to assess ulnar variance on radiographs, as there can be significant foreshortening of the radius, resulting in the ulna impinging upon the lunate bone.
Figure 2-13. Colles fracture. There is an impacted fracture through the distal radial metaphysis (arrows). There is a neutral ulnar variance; the radial and ulnar articular surface are at the same level.
A scaphoid fracture (Figure 2-14) is the most common type of carpal bone fracture. Scaphoid fractures usually cause pain at the base of the thumb and sensitivity to palpation in the anatomic snuffbox. Scaphoid bone fractures can be subtle and may not be apparent initially. Therefore, people with tenderness over the scaphoid are often casted for 7–10 days at which point a second set of radiographs are taken, and may show a more conspicuous fracture line. Alternatively, a CT scan can be used to evaluate the scaphoid. Complications include delayed union, nonunion, and osteonecrosis (Figure 2-15). The scaphoid receives its blood supply primarily from lateral and distal branches of the radial artery. Blood flows from the distal end of the bone to the proximal pole; if this blood flow is disrupted by a fracture, the bone may not heal and may necrose.
Figure 2-14. Scaphoid fracture. There is a nondisplaced fracture through the waist of the scaphoid bone (arrow).
Figure 2-15. MRI of scaphoid fracture. T1-weighted image. The fracture is marked with white arrows. There is decreased signal in the proximal pole of the scaphoid, consistent with avascular necrosis (white star).
Carpal dislocation patterns include the perilunate dislocation, lunate dislocation, and midcarpal dislocation. The injuries are secondary to hyperdorsiflexion. Perilunate dislocation (Figure 2-16) is initially missed in 25% of cases.9 A severe ligament injury is necessary to tear the distal carpal row from the lunate to result in a perilunate dislocation. This injury usually begins at the radial side, with the energy extending through the body of the scaphoid, resulting in a scaphoid fracture. The scaphoid bridges the proximal and distal carpal rows. With dislocation between these rows, the scaphoid must either rotate or fracture, which produces a perilunate dislocation. If there is an associated scaphoid fracture, the injury is called a transscaphoid perilunate dislocation (Figure 2-17).
Figure 2-16. Perilunate dislocation. The lunate bone (black star) maintains its articulation with the radius, but the capitate (white star) is dorsally dislocated from its lunate articulation.
Figure 2-17. Transscaphoid perilunate dislocation (A,B). PA and lateral views of the wrist, respectively, show the lunate well aligned with the distal radius. However, the remainder of the carpal bones are posteriorly dislocated (perilunate dislocation). This is associated with a fracture of the scaphoid waist (transscaphoid), so-called transscaphoid perilunate dislocation.
Intercarpal ligamentous injury may lead to the scapholunate dissociation, producing a gap between the scaphoid and the lunate, so-called “Terry Thomas” sign, named after the British comedian’s gap-toothed smile, also known as the “David Letterman” sign (Figure 2-18). The normal distance between the scaphoid and the lunate is 1–2 mm. A distance of 3 mm or more indicates scapholunate dissociation. The concomitant volar rotation of scaphoid bone is best depicted on a lateral wrist radiograph.
Figure 2-18. Scapholunate dissociation. Rotary subluxation of the scaphoid. Note the wide gap between the scaphoid and the lunate bones (double-headed arrow).
The lunate dislocation (Figure 2-19) is the most severe of the carpal instabilities. The lunate rotates volarly with respect to the radial articular surface. The volar rotation measures approximately 90°, so that the concave distal surface faces anteriorly and the convex proximal surface is dorsally directed. The remaining carpal bones are dorsal to the lunate and the capitate drops into the space vacated by the lunate. This injury results in tearing of most major carpal ligaments.
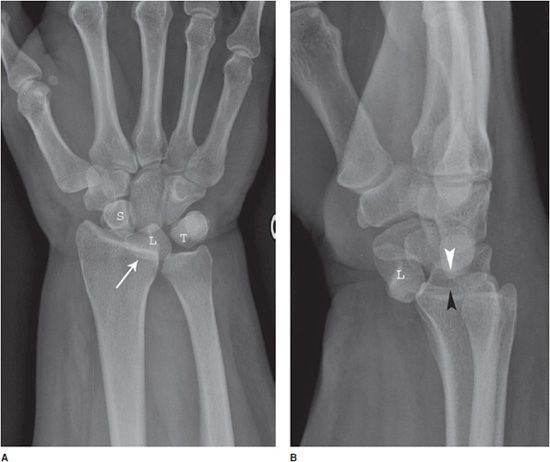
Figure 2-19. Lunate dislocation. (A) PA wrist film demonstrating a triangular appearance of the L, with the apex of the L pointing distally. The L is partially superimposed on the distal radius. (B) Lateral wrist film demonstrates the L to be completely dislocated from its normal position and approximately 90m rotated. The capitate (white arrowhead) is dorsal to the L and occupies the space vacated by the L. The distance to the radial articular surface (black arrowhead) is decreased. L, lunate; S, scaphoid; T, triquetrum.
Carpometacarpal (CMC) dislocations (Figure 2-20) occur infrequently, as these joints are supported by the strength and complexity of the CMC and intermetacarpal ligaments. The fourth and fifth CMC joints are the most common to be individually dislocated because they are more mobile than the third and the second. The oblique view of the hand is most useful in demonstrating this type of injury.10
Figure 2-20. Fourth and fifth carpometacarpal dislocation. (A) There is overlap of the fourth and fifth metacarpal bases with respect to the hamate bone (arrowhead), resulting in joint space loss. Joint spaces at the second and third metacarpophalangeal joints are well preserved (arrows). Note foreshortening of the fourth and fifth metacarpal bones (follow the arc formed by the metacarpal heads). (B) The fourth and fifth metacarpal bases are dorsally displaced (curved arrow). A small avulsion fracture from the hamate is also seen (arrowhead).
HAND
The Bennett fracture (Figure 2-21) is a fracture of the base of the first metacarpal bone that extends into the CMC joint. This intra-articular fracture is the most common type of fracture of the thumb and is nearly always accompanied by some degree of subluxation or frank dislocation of the CMC joint. Pull of the abductor pollicis longus (APL) and adductor pollicis (ADP) muscles results in displacement of the metacarpal base. Failure to properly recognize and treat the Bennett fracture will not only result in an unstable, painful, arthritic CMC joint with diminished range of motion but will also result in a hand with greatly diminished overall function.11
Figure 2-21. Bennett fracture. There is an intra- articular fracture through the base of the first metacarpal bone. The first carpometacarpal joint is disrupted and the metacarpal bone (arrow) is pulled proximally by the abductor pollicis longus muscle. A small bone fragment (arrowhead) remains in anatomic position.
A boxer fracture (Figure 2-22) involves a break in the neck of the metacarpal. It was originally described as a fracture of the fifth metacarpal bone because this is the most common one to break when punching a stationary object. Indications for surgery include more than 40° angulation and 10° of malrotation.
Figure 2-22. Boxer fracture. There is a dorsally angulated fracture at the fifth metacarpal neck (arrow).
Mallet finger, also called baseball finger, is an injury of the extensor digitorum tendon of the fingers at the distal interphalangeal joint (DIP). It results from hyperflexion of the extensor digitorum tendon, and usually occurs when a ball hits an outstretched finger and jams it, creating a ruptured or stretched extensor digitorum tendon. The extensor digitorum tendon can avulse a bone fragment (Figure 2-23). Indications for surgery are if the bony mallet involves more than 30% of the articular surface or there is an open injury.
Figure 2-23. Mallet finger. There is an avulsion fracture at the dorsal base of the distal phalanx of the fourth digit (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree