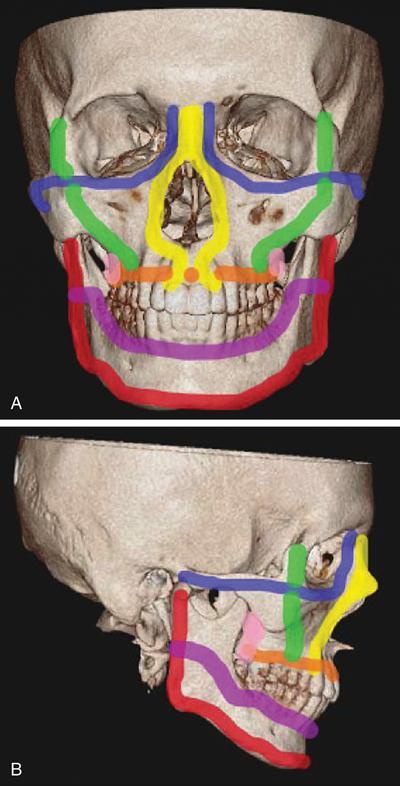
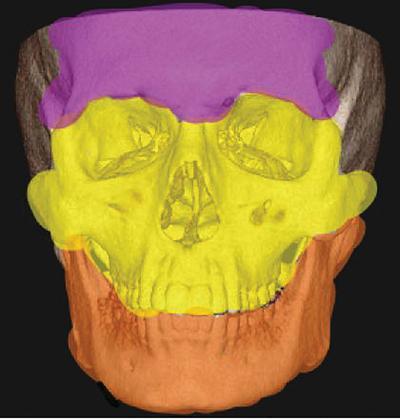
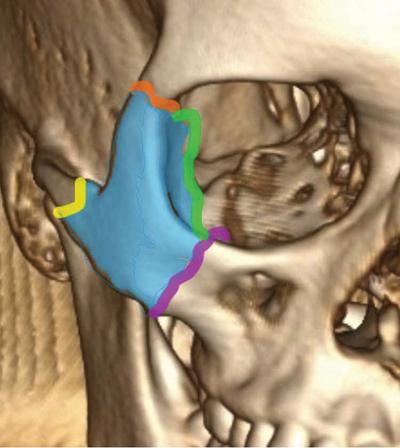
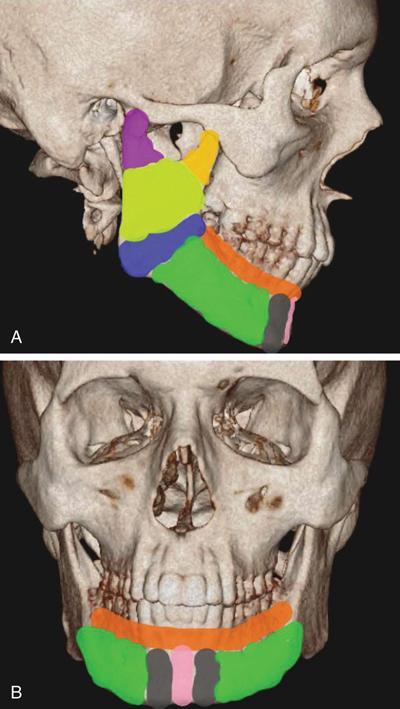
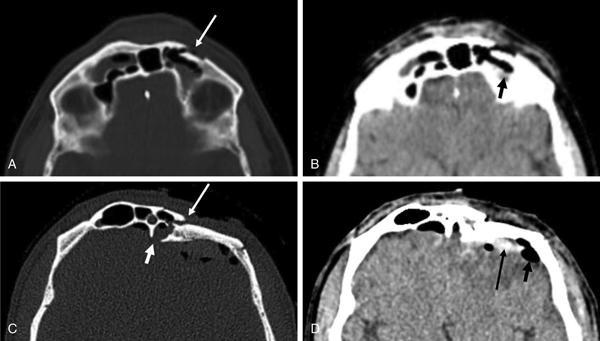
Atin Kumar, M. Sarthak Swarup, Jyoti Kumar The emergencies of head and neck can be broadly divided into traumatic and nontraumatic causes. Traumatic injuries result from blunt or penetrating trauma sustained during road traffic accidents, physical assaults, work-related accidents and falls from height. The osseous injuries can range from a simple, isolated nondisplaced fracture to complex displaced facial fractures. The nontraumatic conditions of the head and neck include a wide range of acute infectious and inflammatory conditions or the complications of head and neck neoplasms. Many of these conditions are associated with significant morbidity and mortality if not detected and treated in time. Imaging plays an important and key role in the evaluation, diagnosis and management of both traumatic and nontraumatic emergencies. Physical examination is not very reliable to rule out facial fractures in polytrauma victims due to distracting injuries and associated facial swelling. Imaging helps in detecting the fractures, their site, displacement and extent, thereby guiding the management decisions. If surgical intervention is required, imaging helps in planning the surgical approach and selecting the intraoperative technique. Computed tomography is often the imaging modality of choice due to its multiplanar capability and its wide availability in the emergency departments. In this chapter, we shall cover the overview of skeletal radiological anatomy of the head and neck with respect to trauma and discuss the various traumatic emergencies including the vascular injuries and the imaging of most common nontraumatic emergencies. The bony facial anatomy of the face is complex and is composed of a total of 14 bones. The maxilla, zygoma, nasal, palatine and lacrimal are the five paired bones, whereas mandible, sphenoid, ethmoid and vomer are the four midline unpaired bones. However, from the clinical perspective, the concept of facial buttresses or struts is more important in defining the traumatic bony lesions. The facial buttresses refer to a series of vertically or longitudinally oriented planes having a greater thickness of bone as compared with the rest of the facial skeleton. These structures maintain the shape and dimension of the face and provide a rigid protective framework for the orbital contents, nasal cavity, paranasal sinuses and teeth. According to this concept, the complex facial skeletal structure can be simplified into four pairs each of horizontally and vertically oriented struts (Fig. 3.42.1). The vertically oriented struts directly or indirectly connect the anterior facial skeleton to the posterior skull base. The facial buttress system represents the lines of inherent strength across the midface. The vertically oriented buttresses are strongest, with the horizontal buttresses providing secondary support. Otolaryngologists are familiar with a different concept of facial skeletal anatomy, in which the osseous facial skeleton is divided into the upper, middle and lower thirds (Fig. 3.42.2). Location-wise description of the fractures with regard to this concept of facial thirds is helpful for surgeons in planning the surgical approach. The upper third of the face consists of the frontal bone (including the frontal sinuses) and is separated from the middle third by the superior orbital rims and walls. The middle third of the face extends from the superior orbital rims inferiorly to the maxilla and thus includes the orbits; the nasal cavity and the maxillary, ethmoid and sphenoid sinuses. This part of the face is bounded posterolaterally by the zygomaticotemporal sutures, which connect the midface to the calvaria, and posteromedially by the pterygoid plates, which connect it to the skull base. The lower third of the face comprises the mandible. The following section describes the relevant imaging anatomy of specific facial regions. The upper third of the nasal region is bony and is made up of nasal bones, frontal processes of the maxilla and nasal process of the frontal bone. The middle and lower thirds of the nose are essentially cartilaginous and composed of upper lateral and lower alar cartilages in both sides and nasal septum in the midline. The nasal septum also has bony and cartilaginous elements. The anterior portion of nasal septum is made up of cartilage, whereas the remainder of the nasal septum is bony and composed of perpendicular plate of the ethmoid, vomer, nasal crest of the maxilla and nasal crest of the palatine bone. This region represents the bony confluence of the nose, orbit, maxilla and cranial vault and is located in the interorbital space. The space is defined laterally by the thin medial orbital walls, posteriorly by the sphenoid sinus, superiorly by the cribriform plate and anteriorly by the bony pillars (composed of the frontal process of the maxilla, nasal process of the frontal bone and the thick proximal nasal bones). The key structures lying within this region include the medial canthal tendon, lacrimal sac, nasolacrimal duct and the olfactory nerves, which can be injured in traumatic insult to this region. Evaluation of cribriform plate should be done meticulously to look for injuries, as the fractures extending superiorly to this can cause a tear in the underlying dura, allowing leakage of cerebrospinal fluid into the paranasal sinuses and nasal cavity (CSF rhinorrhoea). The frontal sinus develops by pneumatization between both the tables of frontal bone, and there is indeed a wide variability in the degree of pneumatization. It is bordered by a thick anterior wall and a relatively thin and delicate posterior wall. The dura mater and underlying frontal brain parenchyma lie in close relation deep to the posterior table. The roof of the orbit is in relation to the inferolateral aspect of the frontal sinus. Frontal sinus drainage pathway is located at the inferomedial aspect of the sinus and drains into the middle meatus. The bony orbit is formed by the contribution from seven bones: the frontal bone, zygoma, maxilla, lacrimal bone, ethmoid, sphenoid and palatine bone. The orbit houses and protects the ocular globes, extraocular muscles and other conal and extraconal structures. There are three apertures in the posterior orbit, which transmit cranial nerves for vision, ocular movement and sensory innervation. These include optic canal (optic nerve), superior orbital fissure (oculomotor, trochlear, ophthalmic division of trigeminal nerve (V1) and abducens nerve) and inferior orbital fissure (infraorbital and zygomatic nerves, branches of maxillary division of trigeminal nerve). In the emergency trauma settings, fractures of the orbit are usually described in relation to the four orbital walls: roof, floor, medial and lateral orbital wall. The infraorbital canal is located in relation to the inferior orbital rim and orbital floor, which transmits the infraorbital nerve, which provides sensory innervation to ipsilateral cheek and maxillary gingiva. The zygomatic bones are a pair of irregular bones that form the anterolateral cheek projections and a large portion of the lateral orbital walls and orbital floors. The zygoma is a thick bone and contributes to the buttress system of the midface and plays an important role in defining the height and width of the midface. It has four sutural attachment sites with the rest of the facial skeleton and calvaria that are often the site of injury namely the zygomaticofrontal suture, the zygomaticomaxillary suture, the zygomaticotemporal suture and the zygomaticosphenoid suture (Fig. 3.42.3). The central midface is composed of a pair of symmetrical maxillary bones joined at the midline. The thicker bony margins of the maxillae are major contributors to the facial buttress system. The maxilla forms the floor of the nasal cavity, part of its lateral wall and roof, and the roof of the oral cavity and contributes to the inferior rim and floor of the orbit. The body of the maxilla is roughly pyramidal in shape and contains the maxillary sinus, which has four walls: anterior, infratemporal (posterior), orbital and nasal. Laterally the maxilla is attached to the zygomatic bone to form the zygomaticomaxillary complex (ZMC) of lateral midface. The alveolar process forms the upper jaw and houses the maxillary teeth. The mandible is a U-shaped curved thick bone and comprises the lower third of the osseous skeleton of the face and provides attachment to the muscles of mastication. The thick mandibular cortices are essential components of both horizontal and vertical buttresses as described previously. The most important part of the mandible is the alveolar arch, which forms the lower jaw and houses the mandibular teeth. The anterior most prominent midportion is known as symphysis, and the areas immediately adjacent to it on either side comprise the parasymphyseal region. The further horizontal lateral portion represents the body of the mandible, which is continuous with the vertically oriented rami (Fig. 3.42.4). The junction of the ramus and body is referred to as the mandibular angle. There are two superior projections from each ramus, the coronoid process anteriorly and condylar process posteriorly. The condyles articulate with the temporal bones at the temporomandibular (TM) joints. Thus, mandible can be viewed as forming a complete ring with the skull base through bilateral TM joints. The TM joints are complex synovial joints and are the only mobile segments of the facial skeleton. The mandibular canal or inferior alveolar canal extends from the mandibular foramen in the lingual aspect of ramus to mental foramen on the buccal side of the body of the mandible. This carries the inferior alveolar nerve, a branch of mandibular division (V3) of the trigeminal nerve that provides sensation to the lower lip, chin, anterior tongue and mandibular teeth. Currently, the radiographs have a limited role in the evaluation of suspected facial fractures in emergency settings. This is because they do not provide sufficient information regarding injury severity and displacement which are the two key aspects essential for emergent management and surgical planning. They may be useful in assessment of certain simple and isolated facial bone fractures such as nasal bone and mandible. With the rapid evolution of multidetector CT techniques and owing to their easy availability, CT has almost completely replaced the conventional radiographs in the evaluation of maxillofacial osseous trauma in most centres worldwide. CT is currently the most commonly used and most sensitive imaging modality for evaluation of simple or complex facial fractures. Rapid acquisition, high spatial resolution and ability to view the bones in multiple reconstructed planes are the major advantages. It can accurately detect and characterize small and undisplaced fractures and their associated complications. Fractures often occult on clinical examination, and radiographs are easily detected on evaluation of the bone window images of CT. Besides this, the multiplanar and volume-rendered three-dimensional reconstruction images provide a good overview of bony facial anatomy, orientation and patterns of facial fractures, involvement of major facial buttresses, displacement and rotation of fracture fragments and help the surgeons in better preoperative planning. CT is also helpful in assessment of soft tissue such as ocular globes, extraocular muscles and other orbital contents. Multidetector CT has become the standard-of-care imaging modality for pre- and postoperative assessment of patients with midfacial fractures and plays a key role in anticipating complications and determining the need and timing of surgery, the ideal surgical exposure, the choice of hardware and the number of points of fixation needed to achieve stability. MRI has limited role in acute trauma settings. However, this can be a useful adjunct in patients with cranial nerve deficits not explained or incompletely characterized by CT. MRI may occasionally be used to evaluate soft-tissue injuries in stable patients due to its excellent soft-tissue contrast. Various patterns and classification systems have been devised for description of facial fractures. Based upon clinical significance, they can be broadly divided into fractures involving single facial buttress (simple) or fractures involving multiple facial buttresses (complex) (Table 3.42.1). Multiple patterns of fracture can coexist in the same patient. Radiologists should detect these fracture patterns and communicate effectively with the surgeons, rather than merely mentioning the bulk list of fractures of individual facial bones. Nasal bones are the most commonly injured bones of the facial skeleton owing to their superficial location and thinness. Nasal bone can be involved as an isolated fracture or as a component of more complex nasoorbitoethmoid (NOE) fractures, more commonly seen in the settings of high impact trauma. Although radiographs are still ordered in some centres, CT is more useful in complete evaluation. CT images should be evaluated in all the planes as subtle fractures of the nasal pyramid, and minimally displaced or transversely oriented fractures can be missed on axial CT evaluation. Sagittal reformatted images have been found to be most sensitive for these injuries. Nasal fractures can be classified according to the plane involved (Table 3.42.2, Figs 3.42.5 and 3.42.6). Fracture severity have been graded by multiple systems depending upon unilateral or bilateral involvement, degree of displacement, presence or absence of comminution, deviation of midline, and septal and soft-tissue injury. CT demonstration of nasal septal haematoma may be limited due to the presence of blood in the nasal cavity. Associated fractures of the anterior nasal spine and bony nasal septum should be meticulously searched and, if detected, warrant a speculum examination for septal cartilage. Identification of septal injury is very important, as extension of the fracture into the cartilage may disrupt the perichondrium, causing a septal haematoma, which may lead to complications such as abscess formation, and septal perforation resulting from ischaemic necrosis. Fracture or dislocation of the nasal septum leading to severe alteration of the nasal midline or with severe soft-tissue injury merits an open repair, whereas most other injuries can be treated with closed reduction. Walls of the frontal sinus are often involved in the fractures affecting the upper third of the face due to relatively thin bone than the rest of the frontal bone. These fractures are classified depending upon the involvement of anterior wall, posterior wall or both (Fig. 3.42.7) and the degree of displacement and comminution of the fracture. Fractures of the posterior wall are rarely isolated and may result in dural tear and communication between the frontal sinus and the anterior cranial fossa, with increased risk of complications such as CSF rhinorrhoea, brain herniation and intracranial infection. Posterior table fractures should be evaluated for displacement, depression, presence of pneumocephalus (suggesting dural disruption) and associated intracranial injury (Fig. 3.42.7). Fracture along the medial aspect of the frontal sinus may extend to involve the nasofrontal duct and obstruct the sinus drainage, leading to complications such as frontal sinus mucocele, sinusitis, osteomyelitis or intracranial extension with brain abscess. Injury to the nasofrontal outflow tract is indicated by frontal sinus floor fracture and medial anterior table fracture. Coronal images are particularly helpful for evaluating the base of the frontal sinus at the site of the ostium of the duct. Presence of fracture fragments within the tract is diagnostic of anatomic nasofrontal outflow tract obstruction. Fractures of the lateral frontal sinus floor usually involve the orbital roof.
3.42: Emergencies in head and neck
Introduction
Facial anatomy
Horizontally oriented facial buttresses
Vertically oriented facial buttresses
Nasal region
Nasoorbitoethmoid region
Frontal sinus region
Orbital region
Zygomatic region
Central face and maxillary region
Mandibular region
Imaging modalities
(a) Radiography
(b) Computed tomography (CT)
(c) Magnetic resonance imaging (MRI)
Traumatic bony facial injuries
Fractures Involving Single Facial Buttress (Simple)
Fractures Involving Multiple Facial Buttresses (Complex)
Nasal bone fracture
Le Fort fracture
Frontal sinus fracture
Nasoorbitoethmoid fracture
Maxillary alveolar arch fracture
Zygomaticomaxillary complex fracture
Isolated zygomatic arch fracture
Mandibular fracture
Isolated orbital wall fracture (blowout fracture)
Nasal injuries


Frontal sinus injuries
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








