Abstract
Emergency radiologists frequently encounter challenges and scenarios that require noninterpretive skills, many of which are outside the formal training that exists in most training programs. For radiologists who fail to recognize these scenarios or are poorly equipped to handle the challenges, there can be a significant impact upon patient care and patient safety. The types of scenarios requiring noninterpretive skills are quite varied, ranging from communication and risk management to serving as a chaperone or managing intravenous contrast extravasation, which can make managing them particularly difficult for many radiologists. We have identified many of these scenarios that may occur in emergency radiology and offer key information and guidance that may serve as a resource to help emergency radiologists supplement their interpretive skills. By adding this noninterpretive expertise, emergency radiologists can be better prepared for situations that arise and become even more valuable members of their clinical team.
Keywords
Communication, contrast extravasation, decision support, dose reduction, informed consent, patient safety, risk management
Communication in Emergency Radiology
Physician-to-Patient Communication
Physician-to-patient communication is a unique challenge for radiologists. Radiologists and patients often have isolated encounters, without any prior patient-physician relationship established. Most radiology services, including an emergency radiology service, do not schedule dedicated clinic time, and therefore meeting with patients may not be a set priority in the daily workflow. Additionally, radiologists often do not have enough information from the emergency medicine team to discuss detailed management plans with patients.
For radiologists in the emergency department (ED), the physician-to-patient communication can come with a different level of challenges. Being physically in the ED and having regular shift work, emergency medicine providers are usually easier to reach for communication of study results, and they are responsible for conveying study results and diagnosis to patients with their management plans. In this setting, radiologists do not commonly encounter opportunities to discuss difficult and stressful imaging results with patients. However, situations requiring radiologist-to-patient communication may still occur. For example, it may be important for a radiologist to communicate with a patient and family when performing a focused assessment with a sonography in trauma (FAST) scan at the bedside.
In emergency radiology, physician-to-patient communication may be useful for obtaining additional clinical information not provided in the imaging requisition. At Harborview Medical Center in Seattle, Washington, emergency radiologists are embedded in the trauma section of the ED and frequently speak with patients for additional clinical history or may even perform a focused physical exam to correlate with imaging findings. In some situations, a radiologist is best suited for directly correlating imaging findings with symptoms or physical examination findings. However, such interactions may be challenging, and specific guidelines are useful to consider.
Five Tips to Begin a Successful Radiologist-to-Patient Communication in the Emergency Department
To begin, it is important to be aware of the time constraint, especially in the busy setting in the ED. It can be useful to initiate communication by explaining the special role that radiologists play in patient care, which is significantly different from the roles of other clinicians that patients usually encounter. Following this introduction, discussion should center around the actual imaging results, without commenting too extensively on the treatment options. The following list of strategies will help radiologists improve communication skills with patients and family members in the ED.
1
Use AIDET (Acknowledge, Introduce, Duration, Explanation, and Thank You) for Patient and Family
In most interactions, including those between radiologists and patients, the first impression can set the tone for the entire conversation. AIDET, which stands for acknowledge, introduce, duration, explanation, and thank you, serves as a useful guideline in promoting effective communication with patients. The role of the radiologist in patient care is not well understood beyond the medical profession, so it is important to provide context to the patient at the start of the conversation. Having a standard scripted introduction can help radiologists begin the interaction smoothly and focus on the specific medical condition of each patient.
An equally important aspect in the first impression is to acknowledge the patient’s family members, friends, or caregivers at the bedside. Many patients present to the ED accompanied by key caregivers who may have just as much clinical information or be directly responsible for decision making. Radiologists should also be mindful of the patient’s privacy and always confirm whether the conversation should be conducted alone or in the presence of the other visitors.
Example for gathering additional clinical information: “Hi, I am Dr. Smith. I’m a radiologist here in the emergency department. Patients usually don’t meet with me directly, but I work behind the scenes with your emergency medicine team to review your x-ray studies and help them make decisions based on the imaging findings. I am in the process of reviewing your foot x-rays and would like to perform a focused physical exam to help me better understand what these images mean.”
Example for performing a FAST scan or other ultrasound study and addressing the patient’s family members: “Hi, my name is Dr. Smith. I am a radiologist here in the emergency department. I understand that you are the sister. I usually work behind the scenes with your emergency medicine team to review imaging studies so that the team can use the results to decide on an appropriate treatment. Today, I’d like to perform a quick ultrasound study. After I complete the exam, I’d also like to share with you what I see.”
2
Give Concise Information, Using Terminology the Patient Can Understand
Radiologists may need to explain medical terminology in simple phrases that are easier for the general public to understand. This can be substantially different from using standard medical jargon when talking to other colleagues in the medical field. In addition, it can be helpful to have images ready or to use hand gestures to provide visual context for the verbal explanation.
Example for gathering additional clinical information: “On your foot x-ray, there is a tiny crack in your bone at the same spot where I just pressed. It seemed like that is where you are having pain as well. From what you told me, this may be a stress fracture from increased running with the new marathon training program you recently started.”
3
Provide a Radiology Plan
Describing a concrete plan can help reduce uncertainty for the patient and increase the level of trust between patients and physicians. However, this is particularly challenging in the ED because treatment plans are often in flux during emergent situations, and there are multiple teams involved in caring for any single patient. In this complex environment, radiologists can help reduce patient anxiety by outlining the process as clearly as possible. For example, if the radiologist is asked to perform a FAST exam at bedside, it is helpful to specify how the result will be communicated to the ED provider, whether via phone or in person. The radiologist can also inform the patient that ED providers and the patient’s primary care providers will be able to access the images and the radiologist’s interpretations.
Example for performing a FAST scan: “The study is normal. I am going to return to my work station and review it again carefully with my colleagues to confirm. Immediately afterward, I will speak to your emergency medicine team to tell them the final results so that they can discuss with you further regarding a treatment plan or other test options. I will also submit a report of the study results into your medical record, so your doctors will be able to access my impression along with the images we took.”
4
Use Nonverbal Cues to Show Empathy
A major aspect of effective communication is making the patient feel comfortable through nonverbal cues. For example, physicians can show empathy for the patient by simply sitting down during their conversations together. This alone can convey that the physician has dedicated time to the patient and can foster an environment conducive to establishing trust.
It is equally important to perceive and respond to nonverbal cues from patients. Patients might indicate, through their body language, emotions that they do not feel comfortable expressing out loud. Being aware of these emotions and validating them verbally can be particularly useful in stressful environments like the ED.
5
Answer All Questions With Patience
Even with the limited time available, it is crucial to give patients a chance to ask questions. The radiologist should directly answer any questions pertaining to the imaging results but defer to the ED providers regarding management plans. In addition to answering questions patiently, the radiologist should reassure the patient that there will be future opportunities to ask questions.
Be Present and Add Value as a Radiologist in the Emergency Department
With recent healthcare reform, reimbursement will soon be tied to patient satisfaction. As such, effective radiologist-patient communications are critical for patient-centered value-based care. In one study, Kuhlman et al. showed that 64% of patients want to meet the radiologists who interpret their exams. Cabarrus et al. found that 85% of patients want to see images as part of the conversation when they receive results. Such data suggest tremendous opportunities for radiologists and emphasizes the increasing importance of effective conversation skills when delivering study results to patients. Radiologists must be cognizant and take advantage of such opportunities when they arise. Radiologists often overestimate the time needed to review images with a patient. In many instances, reviewing images can save time, because a visual explanation of the disease process or abnormality may convey more than even a lengthy verbal discussion. Increasing patient awareness of the radiologist’s role in their care is a valuable way to incorporate radiology in patient-centered care.
The American College of Radiology (ACR) Imaging 3.0 initiative emphasizes radiologists’ visibility and leadership. Providing optimal patient-centered care requires that radiologists employ effective communication skills with fellow physicians and providers and with patients. Using the five tips outlined earlier, radiologists can achieve brief but impactful conversations in the ED.
Physician-to-Physician Communication
Radiologists frequently find themselves professionally compelled to propose alternative imaging plans in discussions with physician colleagues in the ED. Unfortunately, the sensitive dynamics of these conversations all too often produce the conditions necessary for a hostile exchange, especially when the proposed alternative is to forgo imaging altogether. The source of this tension is rooted in some of the most common themes underlying medical staff conflict, namely, deficiency in communication, a lack of trust, and incorrect assumptions.
Despite the potential for conflict, up to 40% of referring providers note that they would like to discuss imaging protocols in advance, and up to 50% are interested in feedback regarding protocol selection. Working in a collaborative fashion can seem time-consuming in the midst of a busy shift; however, investing a small amount of effort initially will save time in the end. Communication skills, negotiation strategies, and a touch of charisma are essential. Radiologists must also be attuned to the needs and priorities of their ED colleagues, namely, assistance in rapidly triaging severity of pathology and provision of timely and accurate diagnoses. The following section lists several strategies that will help the radiologist mitigate conflict and deescalate confrontational interactions as they arise.
Four Key Steps in Mitigating Conflict
1
Ask for More Information
When an inappropriate imaging request is ordered, the first step is to call the provider and ask for more information. This is the most critical step in conflict mitigation and will break down barriers of incorrect assumptions and lack of trust. In most instances, acquiring additional information will prove that the study is indicated or aid in choosing a more appropriate study. In conversation, use the keywords “brief” and “quick” to demonstrate respect for their time and the frenetic nature of their specialty. For example, “Can you briefly describe what you’re looking for?”
Case scenario: A noncontrast head computed tomography (CT) is ordered for the indication chronic headache. The radiologist asks for more information, and the ED provider replies, “Yes, the headache is chronic but has acutely worsened in the last couple of hours.” This indication is now appropriate, and the radiologist prevented conflict by asking for more information and avoiding an incorrect set of assumptions.
2
Provide the Best Alternative
Assisting the ED provider in choosing the most appropriate study can be difficult at times, particularly if the alternative causes perceived delays in patient care. However, the radiologist has the responsibility of caring for the patient beyond the ED visit, often on an inpatient or outpatient basis as the patient’s care evolves. The radiologist can leverage this knowledge to assist the ED provider in confidently selecting the best study in the larger context of a patient’s care. In conversation, use the keywords, “Have you considered?” or “Have you thought about?” to demonstrate regard for their clinical judgment and expertise. Other key phrases such as “saves time in the end” or “best answers your question” connect with their fundamental need for rapid and accurate diagnoses.
Case scenario: A noncontrast head CT is ordered for the indication of chronic headache. The radiologist then proposes the best alternative: “Have you considered a brain magnetic resonance (MR) instead, possibly on an outpatient basis if the patient can be safely discharged tonight? This would ultimately yield the most information and is the best diagnostic test for chronic headache. Overall, this would save time in the end and best answer your question, as the head CT will add time and is unlikely to provide diagnostic value.”
3
Provide Coaching
Myriad factors drive ED physicians in their request for inappropriate or suboptimal imaging studies. However, every instance in which a better alternative is available represents an opportunity for shared learning. Navigating these conversations begins with a thorough understanding of the American College of Emergency Physicians (ACEP) clinical practice guidelines. The ability to confidently reference these guidelines enables us to effectively educate our colleagues regarding these nationally developed standards for clinical management of ED patients. One must initiate these opportunities deftly to avoid the air of condescension. Using the keywords “You’re right, however …” in conversation overall signifies agreement but allows for a small educational opportunity.
Case scenario: A noncontrast head CT is ordered with the indication syncope. The radiologist provides coaching: “You’re right, it is important to rule out acute pathologies in the emergency setting. However, the ACEP guidelines actually state that head CT is not indicated in syncope unless there is focal neurologic deficit, significant head trauma, or some other factor guided by history or physical exam.”
4
Arrive at a Resolution Together
Allow for the possibility that your clinical acumen and even widely accepted practice guidelines may not lead to the best solution for every patient. There are circumstances in which the best course may be to trust the ED physician to exercise clinical judgment and learn to trust his or her intentions. Practice guidelines are recommendations and not absolutes. However, the radiology department should track potentially nonindicated studies with quality improvement/quality assurance databases to link outcomes to provider feedback. Low overutilization rates will continue to be essential in keeping the cost of practicing radiology at reasonable levels, particularly in the transition to new payment models, such as value-based care.
How to Deescalate a Confrontational Situation
Confrontations will inevitably arise, and when they do, it is critical to artfully defuse the situation. One effective method is to redirect attention to the needs of the colleague so he or she feels accepted and understood. Take a moment, refocus one’s perspective, and view the interaction for what it is fundamentally: an ED provider who is worried about a patient. Understanding their basic intent encourages warm and genuine responses, which are two of the key tenants in effective and charismatic communication. Maintaining a friendly temperament despite the conflict helps radiologists foster reputations as valued and accessible colleagues.
During disagreements, tone is everything—in voice and language. Tone is directly related to one’s facial expressions, body language, and hand gestures, which unfortunately are absent in most provider conversations. Over the phone, words and intonation are increasingly important, because they are the radiologist’s only form of communication. It is also important not to let emotions control the conversation. Learn to anticipate conflict, which allows one to respond positively, rather than react negatively.
Communication experts recommend having verbal aikidos that we should all feel comfortable using when necessary. The term is a reference to the martial arts technique of redirecting one’s attacker and describes phrases we can use to defuse escalating tension. For example, phrases such as “you’re right” or “I understand” are generic enough to be used abundantly and provide time to generate thoughtful responses. These phrases also represent a small form of flattery and can validate self-esteem, which may be important as hostile conversation often develops as a result of our colleagues feeling that their professional competence and reputation are under attack.
If the conversation becomes frankly confrontational, redirect attention back onto our shared common goal: the patient. The keywords “Let’s take a step back…” allow for a swift, neutral change in the direction of a conversation and represent the subtle offering of an olive branch. Remind the provider of physician-patient shared decision making, in which informing patients of options, and explaining the risks and benefits, is the cornerstone of patient autonomy and respect. For example, “What do you think the patient would want, if we asked? Would he or she want a head CT now, knowing that it will not be helpful and expose the patient to radiation? Or would he or she be willing to wait for a brain MR sometime this week?”
Finally, if all else fails, reiterate one’s commitment to partnership with the ED provider and formulate a resolution, even if it may occasionally represent a suboptimal solution. Emphasize your commitment to the relationship by stating, “I am happy to do what you feel is best, and from my point of view, this has been an educational and productive conversation.” Medicine can be a contentious profession, and it is difficult not to take altercations personally. Long work hours and conflicting demands can lead to disrespectful behavior between medical professionals, and workplace depression causes inward self-focus, lack of empathy, and unwillingness to cooperate. Hopefully, by employing some of these tactics, such situations become the rare exception to what are largely cordial workplace relationships with ED providers.
Communication to Minimize Litigation
Inappropriate interpretation, transcription mistakes, or deficient documentation of communication and recommendation can lead to errors in radiology reports, which in turn may result in legal action against radiologists. A study of the Physicians Insurers Association of America from 1985 to 2000 demonstrates that radiology ranks sixth among all specialties in the number of lawsuits filed and closed. Medical specialties with higher numbers of malpractice suits compared to radiology include obstetrics and gynecology, internal medicine, family practice, general surgery, and orthopedics. However, this data represented the total number of legal cases, suggesting that radiologists actually encounter much higher litigation rates because they represent less than 4% of doctors in the United States. To minimize litigation risk and avoid anxiety related to malpractice suits, it is paramount that radiologists learn the legal ramifications of radiology reports.
Typical legal implications in radiology are related to a variety of deficiencies in interpretation and reporting. Observation errors and errors in interpretation include scanning errors (failure to focus on the area of lesion), recognition errors (focusing on the territory of the lesion but not detecting the lesion), and errors in decision making. Of the above, decision-related errors are the most common, accounting for approximately 45% of observation errors. Finally, satisfaction of search is an error that can occur after detection of an initial lesion, when radiologists can experience reduced perception of other abnormalities, resulting in false-negative interpretations of secondary lesions.
Communicating results and recommendations have also become an essential part of the daily workflow of radiologists. Four out of five malpractice lawsuits in radiology involve complications in communication. Radiologists can minimize the risk of lawsuits by clearly documenting when and how results are communicated to other providers and to patients. Documentation should include the date and time of communication, the name of the person spoken to, and the context in which the results were discussed. A common scenario in a teaching institution would be when an attending’s final report contains a discrepancy with the overnight resident’s preliminary impression. In some lawsuits, courts have ruled that the final report must be conveyed to the ordering providers and the patient, regardless of urgency.
ACR’s Practice Guideline for Communication of Diagnostic Imaging Findings, published in 2010, states that follow-up studies to clarify or confirm initial findings should be suggested and documented in reports. In lawsuits, an ordering physician can claim ignorance of the proper actions following a radiology diagnosis, because the radiologist did not provide recommendations. Therefore, it is important for radiologists to include concrete follow-up instructions to clarify, confirm, or exclude the initial impression.
Four Must-Do’s in Communicating Imaging Results
This section discusses the four key components of communicating imaging results (in the ED or elsewhere). This is an opportunity for radiologists to directly make a difference by ensuring quality patient care while minimizing litigation risk.
1
Physician-to-Physician Communication
For any critical result or incidental findings warranting further workup or change in management, the radiologist commonly makes a phone call to the ordering provider. When conveying the diagnosis, the conversation should be simple and to the point but ensure that pertinent information is understood. It is important to be very clear, especially when offering two or more diagnoses, and explain to the ordering provider why certain differential diagnoses are more or less likely. As discussed in the previous section on physician-to-physician communication, radiologists should remain professional but firm, even if the ordering providers disagree with the imaging diagnoses.
2
Physician-to-Patient Communication
Compared to the outpatient setting, needing to communicate an urgent finding directly to a patient when the ordering providers cannot be reached is less common in the ED because of the ready availability of dedicated ED providers and staff. However, direct radiologist-to-patient communication of imaging findings can occur in the ED when the radiologist is present for the examination (e.g., ultrasound) or is performing a procedure (e.g., esophagram for leak). Radiologists may also need to contact a patient directly when there is a discrepancy with a preliminary report, and the patient has already been discharged from the ED.
3
Documentation
Documenting communication accurately is a crucial component of the patient’s medical record and for minimizing radiologists’ litigation risk. Essential components include date, time, name of the person spoken to, and the information discussed. If any recommendation was conveyed verbally, it is helpful to include it in the communication section as well. Additionally, it is good practice to document multiple communications when multiple attempts were made or if a radiologist conveyed findings to multiple services on the same study. For example, “The above critical result of a large right-sided pneumothorax was communicated to Dr. Smith (ED resident) and Dr. Jones (surgery chief resident) by Dr. Lee at 1000 hours on 1/24/2017.”
4
Further Recommendations
Recommendations, such as follow-up imaging or interventions, should be made and documented when appropriate. In the ED, this may include recommendations to consult other specialties, such as general surgery or interventional radiology, although radiologists should be careful that such subspecialty consultations are truly warranted. For example, “Recommend follow-up head CT in 6 hours and neurosurgery consult.”
Communication Challenges in the Emergency Department
1
To Whom Should Results Be Communicated in a Busy ED Setting?
At a teaching institution, radiologists may need to decide between conveying results to the attending emergency medicine physicians or the residents. In these situations, one should consult the standard protocol in his or her institution’s ED. Regardless, it is important to always document if a radiologist is unable to reach the ordering provider and the subsequent action taken if any. For example, “Unable to convey results to attending physician (Dr. Smith); the above critical finding was conveyed to the senior resident (Dr. Jones) in the ED.”
2
How Should Nonurgent Incidental Findings Be Managed?
An incidental finding may not seem like a priority in the busy ED setting, but communication and documentation are still necessary to ensure needed outpatient workup. For example, “This is not an emergent finding, but further outpatient workup is recommended.”
3
What Should Be Done During a Trauma Code?
During a trauma code, the emergency room is loud and frenetic with ongoing resuscitation and a large trauma team. At certain institutions, such as Harborview Medical Center, the emergency radiology reading room is embedded in the center of the trauma ED. This allows emergency radiologists to convey the trauma series results directly to the trauma team. In this chaotic environment, it is particularly important to make eye contact to ensure the person in charge of the trauma team receives and acknowledges the critical imaging results. Although difficult, interrupting resuscitation is acceptable when the findings are emergent and will change management, but information conveyed should be concise and clear. Communicating nonurgent incidental findings should take place after the resuscitation is completed.
Awareness of key medicolegal concepts can help radiologists reduce the risk of errors and malpractice lawsuits and ensure optimal patient care. Improving communication skills and consistently documenting conversations are ways that radiologists can take direct action to minimize litigation risk.
Patient Safety in Emergency Radiology
Emergency radiology is a high-stakes environment with rapidly evolving situations and frequent complex decision making. Functioning in this type of high-risk environment creates continual threats to patient safety, and therefore ensuring safety must be a component of the system itself. Safety is a direct result of how an organization is designed, led, and managed. At its most effective, emergency radiology provides frictionless tools and support to allow emergency healthcare personnel to provide safe, effective, patient-centered care.
Most emergency radiology departments have adopted a systematic approach to patient safety such that the entire organization is constantly engaged in efforts to prevent and identify errors before they cause harm. Rather than focusing on individual errors, modern safety practices emphasize organizational elements that promote safety and use error to identify and analyze weaknesses in the system. It is crucial that there is buy-in from all team members to ensure that errors are reported without fear of repercussion and to encourage solutions to problems that arise. Individuals in this environment must be taught situational awareness and encouraged to detect potential adverse events before harm is caused. Standardization can help individuals detect variance and potential deviations. Having a systematic method for capturing safety events should encourage ongoing analysis, timely response, and data gathering for systematic review. Some examples of specific threats against patient safety in emergency radiology include scanning the wrong patient, imaging the wrong side or body part, order entry errors, discrepancies with preliminary interpretations, interruptions and distractions, faulty communication, ineffective handoffs, and fatigue.
To ensure the correct patient and correct body part are imaged, two patient identifiers are used prior to an examination as per Joint Commission requirements. Identifiers include name, date of birth, hospital identification number, or other person-specific identifier and can be verified directly with the patient or a family member, spouse, partner, or healthcare provider who has previously identified the patient. This may seem obvious and straightforward in an outpatient setting but can be quite challenging in a chaotic emergency or trauma setting with an unresponsive patient being actively resuscitated. Patient identifiers must also be cross-referenced with the examination order to ensure the correct examination type and site are performed. After the examination is performed, the technologist must verify that the scanned patient’s images are imported into the matching patient’s folder in the picture archiving and communication system (PACS). Finally, the radiologist must be vigilant and verify that the patient information in the dictated report matches the images reviewed. Each step in this process offers the potential for errors to occur.
Correct patient identification is particularly critical in emergency radiology where images are frequently viewed (by a radiologist or other provider) immediately after they are acquired. Portable radiographs are very common in emergency radiology and particularly prone to error. In a large retrospective review of near-miss wrong-patient events, Sadigh et al. found that portable chest radiography accounted for most mislabeling-misidentification events (69%) and wrong dictation events (44%). Mislabeled or misidentified images in PACS can quickly lead to incorrect decisions and inappropriate or delayed management. Most importantly, they are often difficult to recognize after the error has occurred. In one series, the mean time between when a mislabeling-misidentification event occurred and when it was detected was 100 hours, which could result in severely compromised patient care. Standard procedures are required to minimize such occurrences. For example, the radiology information system (RIS) may link the dictation software and images in PACS. Acquiring facial photographs simultaneously with radiographs has also been reported to increase detection of mislabeled examinations without sacrificing interpretation time.
Effective communication is critical for patient safety in emergency radiology, and specific strategies have already been discussed. Failure to communicate results of radiologic examinations is reportedly the second most common cause of malpractice litigation with communication problems a causative factor in up to 80% of cases. It is insufficient to simply communicate findings and results. Radiologists must communicate results in a comprehensive and timely fashion to the appropriate person with acknowledgment of receipt and understanding of the information. In emergency radiology, it is helpful to have access to an ED whiteboard that is updated in real time to minimize time wasted contacting the incorrect provider. Ensuring that the patient’s care team and contact information are readily available helps to ensure that critical results can be communicated quickly to the appropriate provider.
Handoffs are ubiquitous in emergency radiology, occurring whenever patient information and responsibility are transferred between healthcare providers, and are among the greatest threats to patient safety. For example, a radiologist shift change may include information regarding examinations in progress, patients receiving premedication or intravenous (IV) hydration, protocols on hold, or pages awaiting a return call. In a root cause analysis (RCA), handoffs and resultant patient safety events have been shown to be particularly prone to error when information is exchanged via the telephone, which is especially applicable to emergency radiologists. Ineffective handoff events result in uncertainty regarding the care plan, near misses, or failure to effectively communicate the most important piece of information about a patient, even when the parties involved believe the handoff was effective. Because the resultant errors can have major implications for care, high-quality handoffs must be addressed on an organizational level with directed strategies for providers to ensure effective transfer of critical information. It is critical that participants understand that many handoff errors occur even when both parties believe the handoff is effective; thus specific skills must be taught and acquired.
In general, major discrepancies between resident preliminary and final faculty interpretation are infrequent, with published rates ranging from 0.8% to 2.6% in many large series. Nonetheless, standard practices must be implemented to ensure that discrepancies that do occur are managed in a timely and routine fashion to minimize any adverse effects on patient care. The first step is to ensure consistent reporting of discrepancies, among resident preliminary reports and also discrepancies among other faculty. Participants in a peer-review process must understand and accept that the purpose of the process is to improve safety and is not punitive, to encourage uniform participation and meaningful intervention. Second, emergency radiologists and emergency care providers need a consistent closed-loop process for reporting and tracking discrepancies. This process must include a follow-up mechanism to ensure that discrepancies requiring additional workup or management are tracked until the loop is closed and do not “fall through the cracks.” Periodic review of discrepancy data is also mandatory to identify trends and intervene early before safety is compromised on a larger scale.
In a busy emergency radiology practice, interruptions and distractions are frequent and can increase the possibility of errors. In this setting, radiologists (including trainees, faculty, and practicing radiologists) are constantly shifting attention between medical (e.g., image interpretation, communicating with emergency providers) and nonmedical tasks (e.g., answering phone calls or pages), particularly during off hours when nonphysician support personnel may be less available. Telephone calls are one of the most frequent workflow interrupters and were shown in one series by Balint et al. to raise the probability of a significant error by a radiology resident by 12%. Although telephone calls are a common distraction, they are by no means the only type of interruption that can increase errors and detrimentally affect safety. Any unscheduled workflow disruption can force the radiologist to disengage from his or her interpretive tasks and, in the process, forget the context and mindset that existed prior to the disruption. Returning to the prior mindset is costly, requires added time and effort, and introduces the potential for serious error. Nonetheless, distractions in an emergency radiology reading room are the norm and may be mitigated but not eliminated entirely. For example, nonradiologists can support the radiologist by managing nonmedical tasks and ensuring that interruptions, when they occur, are warranted and time sensitive. As such, efforts to optimize patient safety must balance minimizing interruptions and distractions with maintaining radiologist availability for emergency practitioners. Providing optimal patient care in the ED often relies on time-sensitive consultations, and in this setting, interrupting the radiologist may be appropriate and outweigh the risk of error.
Risk Management for Errors in Emergency Radiology
Risk, Medical Error, and Risk Management
At its core, medical care is a balance of risk and benefit. Risk is defined as a chance or possibility of danger or incurring loss or injury. Medical error is the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim. In the United States, an estimated 44,000 to 98,000 deaths per year may be attributable to medical errors and cost $17 to $29 billion.
It is important to understand that risk is not limited to the patient and also affects the medical practitioner and the healthcare system as a whole. The highest risk for errors exists in high-acuity settings, such as the intensive care unit (ICU), operating room (OR), and ED, and emergency radiology departments interface with all of these departments. Therefore, it is important that emergency radiology departments adopt forward-thinking risk management strategies to identify areas of weakness and reduce the sources of error.
In the simplest terms, radiology risk management includes systems and processes that ensure that medical images are acquired and reported in accordance with agreed protocols, by competent staff working within a defined scope of practice, and with advance identification and addressing of potential problems. This process involves all those who are responsible for the delivery of healthcare, not just the clinician who is directly caring for the patient.
The key to risk management is to acknowledge that mistakes happen and even the best processes and procedures will fail. All participants must be willing to evaluate all actions with transparency and openness, including appropriate efforts to remedy failures and alter practices where needed. A summary of possible errors, scenarios, and recommendations are summarized in Table 26.1 .
| Type of Error | Error/Scenario | Comments/Recommendation |
|---|---|---|
| Mistake, false-positive error |
|
These indicate lack of radiologic/technical skills, experience, knowledge, or insufficient training. Reducing the likelihood of mistakes typically requires more training, supervision, or occasionally disciplinary action (in case of negligence). |
| Slip, false-negative error |
|
Slips are lapses in concentration and failure of schematic behavior due to fatigue, stress, or emotional distractions, unlike mistakes that represent failure during attentional behavior. |
| Latent error |
|
Latent error refers to less apparent failures of organization or design that contribute to errors. They are typically related to a faulty institutional policy, equipment failure, organizational/management flaws, work and team environment, lack of proper staffing, and other reasons. This is also called a blunt-end error, as opposed to an active or sharp-end error, where the source of error lies with the personnel or parts of the healthcare system in direct contact with patient. |
| Close call (near-miss incidents) |
|
No injury happened as a result of this event, due to the robustness of the patient or a fortuitous and timely intervention from a member of the healthcare team. |
| Adverse event |
|
These are undesirable clinical outcomes resulting from some aspect of diagnosis or therapy, not from the underlying disease process. An adverse event does not imply error or poor quality of care. |
Lapses in the standards of care in emergency radiology may present in several ways:
- 1.
A completely unexpected error in radiologic reporting that results in harm to the patient.
- 2.
A service performing suboptimally over a period of time producing unsatisfactory outcomes.
- 3.
An individual practitioner whose performance is impaired due to inadequate knowledge or skills or dysfunction related to health and behavioral problems.
Risk Management in Emergency Radiology: Considerations and Challenges
Errors in Reporting
This is one of the key components of the patient’s overall care in the department. However, for risk management, it must be noted that the radiologist is ultimately responsible for the final report, but reporting is highly dependent on other quality measures in the department and cannot be viewed in isolation. Also, in spite of best efforts and standard reporting practices, variation will exist among radiologist reporting and interpretations. A study of ED plain radiograph reporting showed that disagreement can range from 5% to 9%.
False-positive errors
This error occurs when an abnormality is incorrectly described but is normal or a normal variant. It can also occur when a finding is attributed to the wrong cause. False-positive or cognitive errors are more likely to be related to a lack of experience or knowledge, rather than external factors. However, incomplete clinical data and unavailability of old examinations may also contribute. Risk management issues may involve repeated examinations to assess for change, seeking outside comparison examinations, and comparison with the opposite side, especially in cases of pediatric trauma. False-positive errors in emergency radiology can result in inappropriate treatment initiated for an abnormality that does not exist and treatment complications that may ensue. False-positive errors can also delay the correct diagnosis, because the patient’s symptoms are incorrectly attributed to an alternate diagnosis.
False-negative errors
False-negative errors result from underreporting, where a finding is missed or incorrectly dismissed, and are five times more common than false-positive errors. This includes findings that were not present on the original image due to an inadequate exam. False-negative errors in emergency radiology can have the drastic negative effect of delaying diagnosis and management.
Intrinsic and Extrinsic Factors
Several intrinsic (related to radiologist) and extrinsic factors (not directly related to radiologist) may be responsible for producing errors:
Poor-quality examinations
This can be due to inadequately trained staff, poor equipment, or suboptimal working conditions, such as when a technologist is overwhelmed and unsupported. Poor-quality examinations may result from failure to use correct imaging parameters (radiographic technique, sequence parameters, sonographic gain/frequency, etc.), performing inappropriate views, improper centering of anatomy, failure to mark the region of interest, and so on. It is also important to consider patient factors, such as size, body habitus, inability to stay still, and inability to reposition, which can all be responsible for poor exam quality. This requires staff to be educated about how to identify barriers with directed strategies for how to overcome limitations. Regardless of the source of error, if a radiologist identifies a poor-quality or nondiagnostic exam, he or she should clearly state the technical limitation and request a repeat or alternate procedure and, in most cases, defer interpretation until exam quality is sufficient. The exam should also be flagged for internal review so that a proper risk assessment can be undertaken, and the source of the poor quality can be addressed.
Failure to consult previous studies or reports
The importance of reviewing old studies cannot be understated. Using a comparison examination to establish temporal stability can help make an indeterminate finding more likely benign, which can help prevent unnecessary workup. Similarly, establishing a timeline during which findings developed can help narrow the differential diagnosis or gauge whether findings are getting better or worse. For radiologists, this is analogous to history taking and should be standard practice for all radiologic reporting. To support the radiologist in this effort, hospitals and radiology departments must ensure that there is a robust system for archiving and storage of old studies, such that pertinent comparison exams are readily available when needed. This includes hiring adequate clerical and information technology staff, software support to upload outside studies, and investing in short-term and long-term storage. Achieving such a system requires balancing costs and practicality of storage and retrieval of old images with the risk of a lesion being missed or misinterpreted when old films are not available.
Clinical information
Accurate clinical information is a vital component of an imaging request or requisition. Lack of clinical information or inadequate/inaccurate clinical information has been shown to be a common source of reporting error. Ideally, the requisition will include pertinent clinical information that helps the radiologist focus on the area of concern and answer specific questions. However, it would be naïve to assume that all requisitions will include comprehensive accurate clinical information. In an ED setting, radiologists frequently receive incomplete or irrelevant clinical history, which can be a major source of error and inefficiency. In many cases, at the time the examination is ordered, data gathering is ongoing, so the emergency provider does not yet have all relevant information. Consequently, emergency radiologists should be prepared to search for relevant clinical information when necessary. To support the radiologists, emergency radiology departments should be proactive and establish frictionless mechanisms for accessing the medical record during the course of image interpretation. This can be achieved in a variety of ways, including direct integration of the electronic medical record (EMR) into the PACS, using support personnel to gather additional data, or launching an always-open EMR window on a separate computer or accessory monitor.
Multiple lesions
Failure to report multiple lesions has been previously described as a source of reporting error, commonly due to satisfaction of search. The missed lesions can be related or unrelated to the primary finding. Failure to diagnose an additional neoplastic lesion can change management (e.g., medical vs. surgical) or delay diagnostic workup.
Poor viewing conditions
Standard viewing conditions must be established for image interpretations to minimize error that can result from poor viewing conditions. Interpreting radiographs can be particularly sensitive to viewing conditions, especially for subtle findings. Emergency radiology departments should have standard practices with periodic review of workstations and viewing conditions. Radiologists should also be taught how to establish optimal viewing conditions so that they can report suboptimal conditions if they arise.
Fatigue
Resident and/or staff fatigue is another cause of errors, and several studies have demonstrated how overwork affects accuracy and its medical-legal implications. Strategies for minimizing fatigue can include limiting workload to only truly emergent cases while on call, having overlapping or short call shifts, and providing more coverage to high-volume areas like ED CT.
Service Failure
Some errors are due to failure of the systems or the service line in a hospital or radiology department. Potential areas of service failure include the following:
Inadequate staffing
Hospitals may be inadequately staffed to provide quality emergency radiology services on a 24-hour basis. If 24-hour in-house radiologists are not feasible, then it is imperative to define what services are provided during the daytime and on a 24-hour basis. During holidays and weekends, some specialized services may need to be temporarily withdrawn or arrangements may need to be made with other healthcare providers. In areas where an in-house radiologist is not available, a robust remote access network can be used to allow radiologists elsewhere to remotely view and report studies. Remote interpretations can be provided by radiologists within the department or outsourced to other groups (e.g., teleradiology). Some departments require periodic night shifts for staff and/or residents for ED calls.
Miscommunication
If not addressed on a system level, miscommunication can result in an inappropriate investigation being performed, incorrect treatment initiated, or the wrong patient or wrong side being imaged. Emergency radiology departments need standard practices for communication of urgent results or unsuspected findings to minimize deviation and errors. Many departments use internal codes that flag the study, in addition to documenting verbal communication. All such verbal communication should be followed with documentation in the patient chart or radiology report, indicating the time and the person with whom the information was shared.
Preliminary interpretations
Use of electronic or verbal preliminary reports is a common strategy for providing 24-hour emergency radiology but should be acknowledged as a potential source of system failure, especially if radiologists use them inconsistently or have different expectations for what constitutes a preliminary report. Although it facilitates prompt communication between a busy emergency radiology department and the ED, a hasty verbal impression or incorrect preliminary report can result in serious error, especially when the case was not reviewed comprehensively. Emergency radiology departments must have standard policies regarding what is expected and appropriate for preliminary interpretations so that radiologists and emergency providers have consistent expectations. Reading of preliminary reports by attending and/or subspecialty radiologists should be performed in a timely fashion, with consistent expectations regarding the time from preliminary to final interpretation.
Excess workload/inadequate workflow
Overworked radiology departments with suboptimal workflow will tax all components of the system and are a setup for system-related errors. The department should have mechanisms for dynamically responding to increased workload (e.g., major disaster or trauma), including how to appropriately allocate and assign resources and personnel where needed. Examination volumes should also be periodically evaluated so that longitudinal trends can be identified and increasing workload can be anticipated.
Machine and equipment error
Paperless and filmless departments have been revolutionary but have contributed to another category of errors. Examples include incorrect patient identifiers in the PACS, assigning images to the wrong patient in a RIS-PACS system, dictated reports that are not pushed to PACS and/or the EMR, incorrect examination timestamps that do not match the report, incorrect accession numbers resulting in reports with the wrong header or assigned to the wrong patient, and examinations not completed by technologists that never populate the radiology worklists. The role of the RIS-PACS administrator is critical in anticipating and identifying such errors before they affect patient care.
Practitioner Performance
Lack of subspecialty training
The ever-increasing complexity of radiology coupled with the massive scope of the specialty means that diagnostic imaging is used for a myriad of conditions from head to toe. This presents significant challenges for radiologists and technologists alike. As part of their practice, emergency radiologists often become proficient in the most common examinations performed in the ED, regardless of whether they have received subspecialty training. However, emergency radiologists may encounter examinations for which they do not feel properly trained or have not maintained their expertise, which can lead to errors and suboptimal care. Subspecialty training may be beneficial or required in certain areas, and it is important that radiologists acquire such subspecialty training when it is needed. It is also important that radiologists recognize their limitations and consider subspecialty backup, if available. In large departments, having many radiologists with a variety of subspecialty interests may be feasible, but this may not be possible in small departments.
Lack of continuing medical education
It is imperative that physicians keep abreast of changes in their specialty and within their scope of practice. This is required to provide good patient care and for maintaining hospital credentials, board certification, and licensing. Medical knowledge evolves quickly, and radiologists must include continuing education as a necessary component of their practice.
Inappropriate conduct and psychological or medical problems
Physical and mental health are a critical component of practitioner performance and, when impaired, can result in serious errors and dangerous situations. An impaired physician or staff member poses a risk to him or herself, his or her coworkers, and his or her patients. Continuously assessing practitioner wellness is crucial for maintaining a functional department and should be a priority. Resources must be available so that practitioners know how to recognize impairment, in themselves and others, and how to seek help.
Risk Management Paradigm
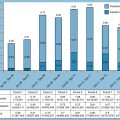
The risk management paradigm involves several components, all sharing the common goal of providing safeguards for the patient, personnel, and the organization ( Fig. 26.1 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree