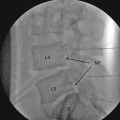
Fig. 36.1
Pictured is an axial CT acquisition with FDCT demonstrating a diskogram of a structurally normal disk. Provocative testing did not yield any pain at this level
FDCT systems produce increased scatter radiation, which can result in artifacts and inaccuracies in CT calculations. Anti-scatter grids that may increase patient radiation dose are commonly used to overcome this problem. However, radiation doses are less than that for a single helical CT [7].
Cone-beam CT/FDCT units are increasingly popular for intraoperative minimally invasive surgery [8]. Transpedicular fusions are one area where this technology is being used with success. Some of the touted advantages of modern imaging system use intraoperatively are (1) reduced time for image acquisition compared to repeatedly bringing a conventional fluoroscope into the field, (2) decreased incidence of transgression of the pedicle, (3) reduced overall operating time, and (4) reduced dose of radiation to both the surgeon and the patient. For example, a recent study compared intraoperative computer-assisted spinal navigation to serial radiography for posterior fusions at the L5/S1 level. The navigation system shortened the operative time by about 40 min compared to serial radiographs [9]. More recently, a Japanese group compared isocentric three-dimensional fluoroscopy with navigation to conventional fluoroscopy for percutaneous screw placements. This large study included 300 percutaneous screw placements of which half were inserted with the advanced imaging and half with conventional fluoroscopy. They then evaluated post-procedural accuracy with 2-mm axial slice CT imaging. The authors found that there were 7.3 % exposed screws and zero perforated pedicles in the three-dimensional image group compared to 12 % exposed screws and 3.3 % perforated pedicles in the conventional fluoroscopy group. This was a statistically significant difference for pedicle screw misplacement (P < 0.05) [10]. In a previous study of conventional two-dimensional fluoroscopy, Weinstein et al. noted a 21 % rate of misplaced pedicle screws, with the vast majority being on the medial side (towards the spinal canal) [11]. The performance of celiac or superior hypogastric plexus neurolytic blocks is potentially impeded by the size of the local tumor burden or lymphadenopathy which may limit spread of the alcohol or phenol neurolytic solution. Other soft tissue structures such as the renal cortex, thoracic duct, abdominal aorta, or inferior vena cava for celiac plexus blocks or the iliac veins, L5/S1 disk, and L5 nerve root for superior hypogastric plexus blocks may be injured by two-dimensional guidance alone. Thus, a three-dimensional imaging system may improve block accuracy and decrease potential complications. Goldschneider et al. [12] used a 3D-RA system to perform celiac plexus blocks in children with good outcomes.
When performing vertebral augmentation procedures, it is normally considered a contraindication to proceed if a retropulsed fragment is pushing posteriorly into the spinal canal, due to the risk of neurological injury as polymethyl methacrylate (PMMA) cement is injected into the vertebral body. Knight et al. demonstrated the utility of CBCT imaging for this exact scenario, however, with a successful vertebroplasty in a patient with a retropulsed bone fragment [13]. The utilization of three-dimensional technology to better treat patients seems likely to grow as the creativity of proceduralists catches up to the capability of the imaging.
Magnetic Resonance Guidance
The use of magnetic resonance imaging (MRI) has lagged behind some of the other imaging modalities but may have significant future uses. Most physicians who treat patients with complex spine disease appreciate the superiority of the imaging of soft tissue structures with MRI. However, the lack of real-time injection, the limited access to the patient, and the need for MRI-safe equipment were significant problems to overcome. Some of the advantages of MRI imaging are the lack of radiation risks (making it potentially superior for the care of pregnant women and children as well as decreasing risks to the operator), the familiarity of spinal injectionists with MRI images, and the ability to avoid contrast dyes for patients with allergies. Disadvantages of MRI-image guidance with optical tracking include distortion of imaging with needle bending, which may malposition the graphic overlay. This may increase the number of images necessary to accurately reach the target [14]. Sequeiros and colleagues evaluated the feasibility of MR guidance with an optical tracking system for diskography. The authors found that the results were similar to those with conventional fluoroscopy or CT. A 0.23 T open configuration MRI unit was utilized. Only one complication, a collapsed disk, occurred during their study of 35 patients, with 34 procedures completed [14]. In another study, Streitparth et al. studied the outcomes of spinal injection procedures such as nerve root injection, facet joint, and sacroiliac joint injections performed in an open-field MRI of 1.0 T with vertical field orientation [15]. The authors found that proton-density-weighted turbo spin-echo (PDw TSE) technique was optimal for the image guidance. They studied 183 total injections in 53 patients. Target delivery of injectate was achieved in 100 % of the nerve root blocks, but only 87 % of the facet and sacroiliac joint injections. Posterior osteophytes limited appropriate spread in some patients. There were no major complications. MRI-image guidance has not yet come of age but may continue to grow for particular procedures. Certainly, the advantages of soft tissue imaging and lack of radiation risks warrant ongoing research.
Ultrasound
Ultrasound is another technique that has become more popular with anesthesiologists for regional block procedures and with physiatrists for musculoskeletal diagnosis and joint injections over the last decade. Some chronic pain practitioners are advocating use of ultrasound for additional procedures [2]. The ability to visualize soft tissue targets (such as nerves, blood vessels, muscles, and ligaments), evaluate for anatomic variants, and the lack of risk from radiation are attractive reasons to use US. Multiple feasibility studies have been published examining the merits of various blocks of small sensory or mixed nerves, including the ilioinguinal/iliohypogastric, saphenous, lateral femoral cutaneous, suprascapular, pudendal, intercostal, and greater occipital nerves to name a few, have turned up in the last few years [16–21]. The advantage of many of these blocks is that they had previously been targeted mostly utilizing surface landmarks. Thus, the accuracy of blockade should be increased by any of the soft tissue image-guidance techniques. Some papers have examined the use of US for axial targets, but the deeper location of these blocks, the dropout (dark hypo-acoustic window causing poor visualization) caused by bone and lack of real-time contrast injection capability, renders procedures such as epidurals, selective spinal nerve blocks, facet joint blocks, lumbar, celiac and pelvic sympathetic blocks, and a few others extremely difficult and requiring of significant experience and skill.
Sympathetic Blocks
Stellate ganglion block is an example of one sympathetic block which may be advantageous for US blockade. Kapral et al. was the first to describe this technique and noted a decrease in the number of accidental vascular punctures in an ultrasound group compared to a surface landmark group [22]. Recently summarized risks of vertebral artery or deep/ascending cervical artery uptake or neck hematoma punctuate the seriousness of complications. A review from Japan reported 27 cases of retropharyngeal hematoma after stellate ganglion block (SGB) [23]. Narouze and colleagues have described the possibility of esophageal puncture as an additional risk [24]. Celiac plexus block has been studied using an anterior approach. Injury to bowel or organs is the main risks of anterior approaches. One study that is best characterized as US-assisted celiac plexus block had good success, but by today’s standards, the imaging is poor [25]. As current CT and fluoroscopy techniques are good, it is unlikely that ultrasound will make great inroads in this area.
Trigger Point and Muscular Injections
There is little glamour in the performance of deep muscular and trigger point injections, which are usually office-based procedures. Only in the thoracic area or the abdomen is there any real risk of a major complication. Fluoroscopy is basically unnecessary for these soft targets. However, ultrasound may have real advantages, as the different muscle and fascial layers can be visualized well. A deep muscle like the piriformis muscle could be targeted more accurately using US. US offers the opportunity to perform a diagnostic exam (hip rotation) to aid needle localization in the correct muscle, whereby fluoroscopy could show a contrast-striated pattern, for example, but the needle could mistakenly be in a gluteal muscle. Studies suggest excellent accuracy [26]. Trigger points in other areas have been improved by US targeting [27]. Previous closed claim data shows the danger of pneumothorax from a misplaced trigger point in the thoracic area [28].
Zygapophyseal (Facet) Joint Injections and Medial Branch Blocks
Lumbar approaches to the facet joints and the medial branch nerves have been conducted. One trial compared ultrasound-guided facet joint injections to computed tomography (CT)-guided injections [29]. Ultrasound compared favorably to the outcomes from CT in this trial. The patients with larger body mass could not be performed with US, however. Ionizing radiation doses were reduced during the study, with the US group demonstrating a mean of 14.2 ± 11.7 versus 364.4 ± 213.7 mGy.cm for the group blocked utilizing CT. The US group was also blocked in a shorter time span, which may be advantageous in a busy practice [29]. Lumbar medial branch blocks have been investigated too. One study compared blocks of the medial branches performed with US or fluoroscopy. US consistently produced blocks at the correct level suggesting precise placement, with 95 % of the needles in correct anatomical position to effectively interrupt nerve conduction [30].
A study of US utilized for third occipital nerve block procedures in the cervical spine also demonstrated good results [3] as 23 of 28 needles were placed correctly [31]. Given the fact that fluoroscopically guided procedures targeting the third occipital nerve require a three-needle approach on or around the C2/3 zygapophyseal joint, the results are intriguing.