Fig. 8.1
Endocavity 2D transducer (BK 1850) with 360° rotating element (BK6005) in Hardcone for endoanal ultrasound

Fig. 8.2
3D endoanal transducer (BK 2052)

Fig. 8.3
BK Pro Focus 2202 ultrasound system
Technique of Endoanal and Endorectal Ultrasound
No oral bowel preparation is required. For endorectal ultrasound, a Fleet or similar enema is given just prior to the examination. No sedation or anaesthetic is needed.
Patients are positioned in the left lateral position with the buttocks close to or overhanging the edge of the examination bed. For endoanal ultrasound, the lubricated transducer is inserted a distance of about 8 cm. In the male, the distal prostate should be visualised; in the female, the cervix. Images are then obtained at the level of the puborectalis muscle, upper, mid- and lower anal canal (Figs. 8.4, 8.5, 8.6, and 8.7).
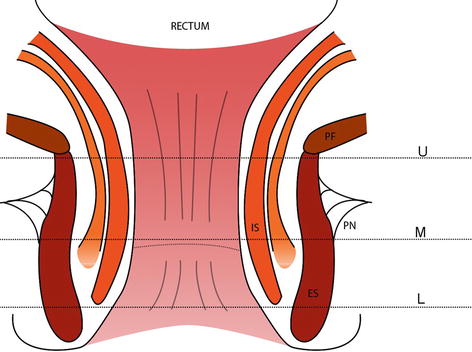
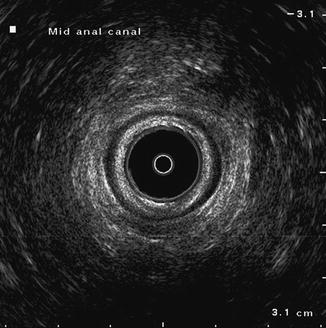
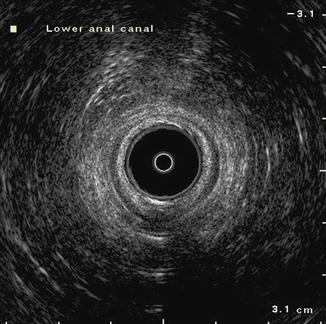
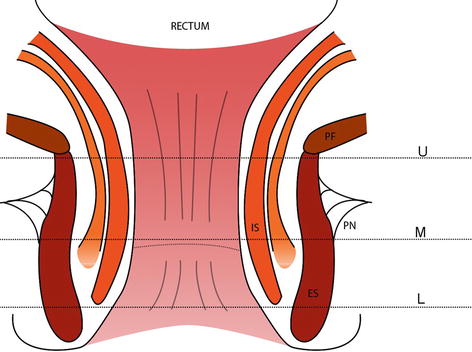
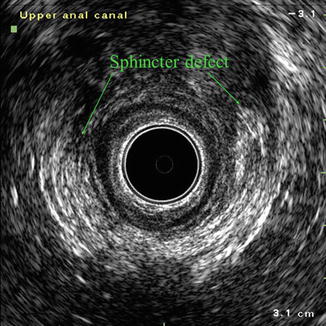
Fig. 8.5
Endoanal ultrasound image at level of upper anal canal T transducer, M mucosa, IS internal sphincter, ES external sphincter, Ant anterior, Post posterior
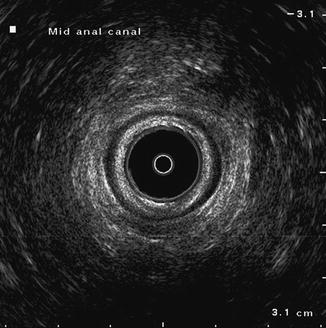
Fig. 8.6
Endoanal ultrasound image at level of mid anal canal
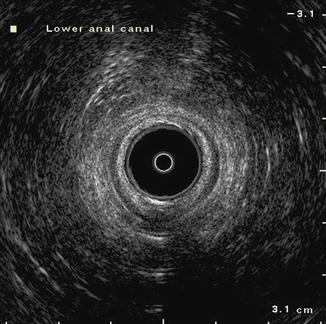
Fig. 8.7
Endoanal ultrasound image at level of distal anal canal
For endorectal ultrasound, the transducer is introduced to just proximal to the pelvic floor then the balloon is partly inflated with degassed water. The transducer can then be slowly manoeuvred proximally to the desired level. Alternatively the transducer can be introduced through a rigid sigmoidoscope.
Indications for Endoanal Ultrasound
Evaluation of Sphincter Defects
Endo anal ultrasound is invaluable in evaluation of sphincter defects in patients with fecal incontinence. Sphincter defects may involve the internal sphincter, external sphincter or a combination. Most are obstetric related but may be traumatic (usually post surgical) or sepsis related. Defects may be discrete or multiple. Figure 8.8 illustrates an anterior external sphincter defect following obstetric injury and third degree tear. There is discrete separation of external sphincter fibres anteriorly. Severe pelvic floor injury during delivery can result in fourth degree tears and development of ano-vaginal fistula (Fig. 8.9). Endoanal ultrasound can be helpful following surgical treatment (Figs. 8.10, 8.11, and 8.12) and in assessment of rectal prolapse (Fig. 8.13).