Cervical radiculopathy
Cervical degenerative disk disease
Cervical disk herniation
Cervical spinal stenosis
Cervical postlaminectomy (failed neck) surgery syndrome
Cervical vertebral compression fractures
Postherpetic neuralgia/herpes zoster
Complex regional pain syndrome (I and II)
Peripheral neuropathy (diabetic, chemotherapy induced, etc.)
Phantom limb pain
Cancer-related pain
Contraindications
Absolute: unwilling patient, localized infection over procedure area, current anticoagulant use (see current america society of regional anesthesia (ASRA) and pain medicine guidelines on anticoagulants), increased intracranial pressure (ICP), bleeding diathesis, and patient that cannot remain still during the procedure.
Relative: allergy to medications that will be injected (contrast, local anesthetic, steroid) pregnancy, immunosuppression, systemic infection, and anatomic changes that would prevent a safe procedure (congenital or surgical).
Cervical Epidural Transforaminal Epidural Injection Technique
Because of the risks associated with this procedure, only physicians who have training and experience in using fluoroscopy as well as precise injection techniques should perform this procedure. All patients should be fully monitored, and equipment to handle airway, local anesthetic toxicity, and cardiovascular emergencies should be readily available.
Although physicians may have different techniques, the primary aspects of all must include proper positioning of the patient in order to optimize visualization of the anatomy of the cervical spine at the target level(s). After discussing risks and benefits, answering questions, and obtaining written informed consent, an intravenous line is placed (for sedation or for emergency access). The patient is taken into the procedure suite and can be placed in the supine, oblique, or lateral position depending on physician preference. The area of the neck is prepped and draped in a sterile manner. The fluoroscopy beam is then adjusted to visualize the intervertebral foramen at its maximum diameter, usually an anterior oblique view. The anterior surface of the superior articular process of the inferior vertebrae (posterior aspect of foramen) is identified, and the entry point is marked. The skin and subcutaneous tissues are anesthetized with 1 % lidocaine. A 25-gauge needle is then directed toward the anterior portion of the superior articular process. It should always be directed toward this bony landmark, as going directly toward the foramen could result in a needle being placed too deep and into the spinal cord. Once the superior articular process is contacted, the depth of the needle should be noted. Repositioning of the needle should never exceed this noted depth by more than a few millimeters. The needle is then carefully adjusted so that it passes into the intervertebral foramen. The needle should always remain slightly anterior to the superior articular process. It should never be in the anterior portion of the intervertebral foramen as this may risk injection into the vertebral artery.
Once the needle is in the correct position, the fluoroscope is repositioned for a true anteroposterior (AP) view. This will allow the physician to see the depth of the needle. The correct depth is when the tip of the needle lies opposite the sagittal midline of the silhouettes of the articular pillars. If the needle contacts the existing nerve root, the patient will feel radicular pain. At this point, the needle should be slightly withdrawn and the procedure halted until the sensation disappears. If the sensation does disappear, the needle can be redirected back to its intended position, but avoiding the exact spot that caused the radicular pain. Fluoroscopy should be used to check in an oblique direction as well as an AP view to confirm needle position and depth. Only after this is done should anything be injected.
After negative aspiration is confirmed, less than 1 ml of contrast solution is injected under live fluoroscopy. It should enter the intervertebral foramen and outline the spinal nerve. It is of utmost importance to be sure there is no intra-arterial injection of contrast. Although this location of needle placement usually will not contain a radicular or a vertebral artery, these arteries can be atypically located. In case of an intra-arterial injection, the contrast will move and disappear during live fluoroscopy. If this is the case, one can redirect the needle until contrast is not seen entering an artery. However, it may be more prudent, given the severity of possible intra-articular injection through the punctured site, to abort the procedure. If contrast injection leads to rapid dilution of the contrast material, it may imply that there has been subarachnoid needle placement. In this case, abort the procedure and give enough time for the puncture to heal as injection even into another location may lead to entrance of medication into the subarachnoid space through the puncture hole created.
Once it has been confirmed by AP and oblique views that there has been correct needle placement, contrast injection has been negative for intra-arterial and subarachnoid injection, the contrast appropriately outlines the spinal nerve, and injection of contrast is negative for pain or paresthesia, the local anesthetic and steroid can be given. How much steroid depends on whether the pain is monoradicular or multiradicular. If monoradicular, betamethasone (3–6 mg), triamcinolone (20–40 mg), or dexamethasone (7.5–10 mg) can be used. If multiradicular, betamethasone (12 mg), triamcinolone (80 mg), or dexamethasone (15 mg) can be used.
Once the medication has been injected, the needle is removed with a saline or local anesthetic flush to clear the needle and track of steroid. The area that was prepped should be cleansed and a bandage placed over site of needle insertion. The patient should then be taken to a recovery area where they should be monitored for complications resulting from conscious sedation as well as complications from the procedure itself.
Cervical Translaminar Epidural Injection Technique
This procedure can be performed by either a loss of resistance technique or a hanging drop technique. One technique has not been shown to be better than the other; thus, the choice of technique is based on physician preference.
Loss of Resistance Technique
After discussing risks and benefits, answering questions, and obtaining written informed consent, an intravenous line is placed (for sedation or for emergency access).The cervical interlaminar technique can be performed in either a sitting, lateral, or prone position. Each position has its own advantages and disadvantages. Since most pain practitioners use fluoroscopy to perform cervical epidural injections, the prone or lateral position is utilized. The cervical spine should be flexed to maximize the opening of the intervertebral spaces.
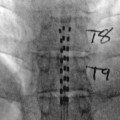
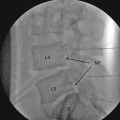
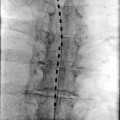
Once the patient is appropriately positioned, the neck is prepped and draped in a sterile manner, and AP fluoroscopy is used to identify the interspace that will be entered. A 17- or 18-gauge Tuohy needle (3.5 in.) is suitable for most patients. The lamina of the inferior vertebra (i.e., the lamina of T1 if performing a C7–T1 injection) is noted on AP fluoroscopy. The skin and subcutaneous tissues overlying the area are then anesthetized with 1 % lidocaine. The epidural needle is then slowly advanced under intermittent fluoroscopy until contact is made with the lamina. The depth of the needle should be noted. Once the lamina has been contacted, the stylet is removed and a lubricated 5-ml glass syringe is connected to the needle. The syringe can be filled with air, sterile saline, or both. The needle is then walked off the lamina and into the epidural space. This should be performed using a two-handed technique with the hand holding the needle stabilized against the patient’s neck to protect against needle movement if the patient moves. The syringe is slowly advanced while always maintaining continuous pressure against the plunger. Once the bevel passes into the epidural space, there is a sudden loss of resistance. The syringe is then removed from the needle, and 1 ml of contrast is injected. Epidural spread of the contrast should be noted. If subarachnoid spread (dilution) is noted, the procedure should be aborted as the puncture site may act as a gateway for local anesthetic and steroid to enter the subarachnoid space even if the injection is attempted in another intervertebral space.
Once needle location in the epidural space is confirmed, negative aspiration for blood and cerebrospinal fluid (CSF) must be confirmed; then, the medication can be injected. The needle is then withdrawn with a local anesthetic or saline flush to remove steroid from the needle and injection track.
The spread of medication in the epidural space is dependent on volume of injectate, dilation of the veins, anatomic differences in the epidural space, and age and height [7]. A number of local anesthetics can be used including lidocaine and bupivacaine. Generally, about 7 ml is enough volume to adequately cover the nerve roots with local anesthetic and steroid [8].
Hanging Drop Technique
The hanging drop technique is an alternative to the loss of resistance technique to signify entrance into the epidural space. The technique is similar to the loss of resistance technique initially as the Tuohy needle is advanced until lamina is contacted. At this point, instead of attaching a glass/plastic loss of resistance syringe, the needle is filled with saline until a bubble of fluid is visible at the hub. The needle is slowly advanced, and once the needle enters and passes through the ligamentum flavum, the drop of fluid is drawn in. This is thought to be due to the pressure in the epidural space being lower than atmospheric pressure. A lateral fluoroscopic view can be used to confirm proper positioning of the needle tip in the epidural space. The remainder of the procedure is similar to that described for a loss of resistance technique.
As an alternative to cervical transforaminal injections, a catheter can be used through the translaminar approach and directed to the nerve root as it comes off of the spinal cord. A smaller amount of medication can then be used. There is a much lower risk of injection into a vertebral artery or into a radicular artery while still accomplishing a selective nerve root block. No studies have been published comparing the efficacy of this approach versus a transforaminal approach.
Complications
Drug Related
Corticosteroids: mostly due to systemic absorption and are short-lived. It includes rash, nausea, pruritis, and hyperglycemia. More severe reactions include a Cushingoid response and adrenocortical failure.
Local anesthetics: rash, nausea, and accidental intrathecal injection with resultant spinal anesthesia. Systemic absorption can lead to seizures and refractory cardiac arrhythmias.
Procedure Related
Complications can be associated with both routes of access. These include postdural puncture headaches, infection, development of epidural hematoma (which could lead to quadriplegia), subarachnoid injection leading to a complete spinal block, and direct cervical spinal cord trauma. However, the incidences of these complications are lower in interlaminar injections if the procedure is carried out in a cooperative patient using fluoroscopy and contrast medium [9]. Multiple case reports of serious complications have been reported after cervical transforaminal injections, ranging from paraplegia to death. This is thought to be due to accidental injection of particulate steroid into a cervical radicular artery. This may lead to spinal cord infarction followed by impairment. As stated previously, no head-to-head comparisons have been done between interlaminar and transforaminal cervical epidural steroid injections. Given the positive results seen with the interlaminar approach and the serious complications associated with the transforaminal approach, it may be prudent to consider the former rather than the latter.
Thoracic Epidural Injections
This procedure is becoming more common in the chronic pain management arena. Similar to the cervical epidural procedure, the spinal cord can be injured during this procedure. It must also be remembered that the artery of Adamkiewicz can be located anywhere in the lower thoracic levels.
Indications
There are multiple uses for thoracic epidurals. One of the most common chronic pain uses is for treatment of postherpetic neuralgia. The thoracic dermatomes are the most common location for occurrence of postherpetic neuralgia. It has been shown that performing an epidural with local anesthetic during an acute herpes zoster outbreak may actually prevent PHN from developing [10].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree