Chapter 3 Exposure factors, manipulation and dose
Image quality
Density
The use of a logarithmic measure is appropriate as the response of the eye to visual stimulation is itself logarithmic.1,2
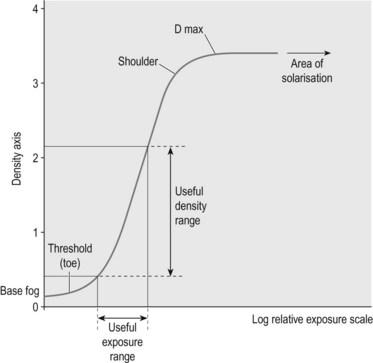
In order to be useful, the range of densities demonstrated on the image needs to be within the range for visual perception and differentiation, usually considered to be approximately D = 0.25 → 2.50 (Figure 3.1).3 Although a density of >2.5 may not be immediately differentiated by eye, densities of up to 4 may be recorded on film.4 In effect, too much information has been recorded; it is sometimes (but not always) possible to use and view this information by use of increased illumination (‘bright light’) or photographic reduction.
Variation of applied mAs is often given as the controlling factor for density,5 although the effect of variation of kVp on intensity, and therefore density, must also be considered. However, in general it is considered better to use a fixed kVp for each examination, using variations of mAs to control required changes in density.6
Contrast
Contrast can be shown to be inversely proportional to the applied kVp, hence in general at lower kVp values greater subject contrast is obtained. This is because, in the diagnostic range, the main interaction processes responsible for attenuation are photoelectric absorption and Compton scatter. Photoelectric absorption for a given beam energy is proportional to the cube of the atomic number and directly proportional to the density of the structure imaged, hence using the exposure ranges where photoelectric absorption is the dominant process (lower kVp) will maximise subject contrast. As digital systems manipulate the acquired image to produce a fixed image contrast (as described in Chapter 1), the direct relationship between kVp and subject contrast can be lost.
There is again a dose trade-off, as use of low kVp may increase skin dose. Several studies support the use of high kVp as a means of dose reduction. Guidelines for paediatric radiography recommend the use of 55–60 kVp, even for extremity work,7 but the increase in kVp will reduce subject contrast and hence image definition.8 Commonly forgotten in departments that have adapted this technique for adult use is the requirement for additional copper filtration to optimise the useful spectrum. Failure to use this additional filtration results in a reduction in image quality without the full benefit of the dose reduction intended.
High contrast, lower kVp, can be referred to as ‘short scale’,5 i.e. fewer shades of grey are represented within the image; consequently, fewer are available to represent the structures to be demonstrated. Use of a high kVp (120+)9 reduces the radiographic contrast but enables all structures to be visualised within the useful density range. Low contrast produces a ‘long scale’ image,5 with more shades of grey available for image depiction; the result is a ‘flatter’ image but with greater detail, particularly of lung parenchyma.
The ‘flat’ or grey appearance of such images does not suit all subjective tastes, and as such the technique is not universally accepted; however, this subjectivity is difficult to reconcile with accepted best practice, in terms of both image quality and dosimetry. Film readers need to educate themselves to accept these changes and embrace best practice,7 the evidence for which is now long established.9
Not to be confused with subject contrast as described above, subjective contrast is due to the observer rather than inherent in the image,10 but is nonetheless important to consider. The observer needs to be considered: eye strain and fatigue can have an effect on perception and several short viewing (or reporting) sessions are preferable to a single extended session; aids to visual acuity should be used as required (e.g. spectacles should be worn if they are needed!).
Viewing conditions need to be optimal. A dim viewing box in high ambient lighting, or holding a radiograph up to a window, are not ideal viewing conditions and will not enable accurate appreciation of either the radiographic density or the contrast demonstrated on the image. Viewing boxes should be matched for brightness and colour of illumination, checked on a regular basis, and used in appropriate conditions, i.e. in low ambient lighting.11 Digital viewing stations should be of appropriate resolution and correctly adjusted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree