Chapter 31 Eye and orbit
Pathology
Malignant
Tumours can be classified as arising from the skin and adnexia, orbit or intraocularly. Basal cell carcinomas (BCC) and squamous cell carcinomas (SCCs) are skin tumours commonly arising on the face, especially around the eye and lower eye lid. In contrast, lacrimal gland and nasolacrimal duct tumours are rare, as are orbital tumours. Rhabdomyosarcoma of the orbit is a tumour of childhood. It is usually embryonal and is discussed in further detail in Chapter 33. Intraocular tumours are rare with retinoblastoma occurring in the very young and melanoma in adults. The choroid is the commonest site in the eye for metastatic disease.
Primary tumours of the eye and orbit are listed below:
Radiation and ocular morbidity
The lens
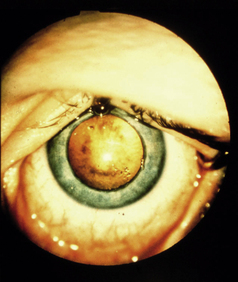
The eye contains structures that are both very radiosensitive and radioresistant. One of the most sensitive tissues in the body is the lens. Cataracts have been reported at doses as low as 2 Gy. However, it should be remembered that they invariably occur over the age of 70 and are associated with various common diseases, such as diabetes, and medications, such as steroids. The appearance and region of the cataract can help in deciding their causation. Radiation cataracts are caused by damage to cells in the anterior central area of the lens, which then start to form a cataract at the back of the lens centrally. The total dose, energy of radiation, volume of the lens, health of the eye and concomitant disease are all factors that play a part in cataract formation. When high doses are given with β-irradiation eye plaques, usually for treatment of posterior choroidal melanomas, cataracts often will not occur because of the rapid fall off of dose (as opposed to the historical use of cobalt plaques). After external beam radiotherapy, fractionated doses of over 10 Gy are likely to cause detectable lens opacities, usually occurring within 2–3 years of radiotherapy. Figure 31.1 shows a radiation cataract. Treatment of a cataract is by surgical removal, although if the eye is dry (most commonly as a result of radiotherapy), this may adversely affect the success of surgery.
The sclera and retina
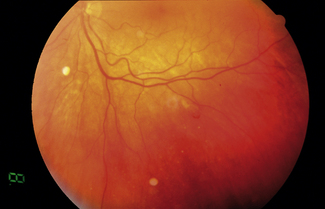
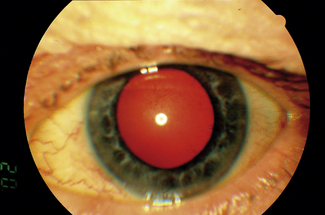
The sclera, on the other hand, is radioresistant because it is avascular and can tolerate doses of up to 100 Gy by radioactive eye plaques to a small area. Above this dose there is a risk of necrosis. The retina can tolerate doses of 50 Gy but, above this, retinal damage is manifest by haemorrhages, exudates and atrophy. Radiation atrophy and post-subcapsular cataract are shown in Figures 31.2 and 31.3. The macula is the most sensitive area of the retina and doses here should be minimized or avoided if possible when using radioactive eye plaques. Similarly, as the dose increases above 50 Gy, there is an increasing likelihood of optic atrophy.
The cornea and lacrimal apparatus
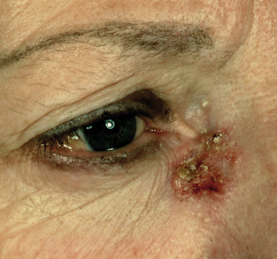
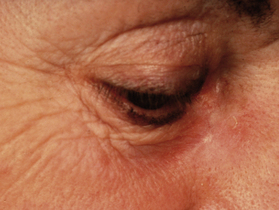
Stenosis or occlusion of the nasolacrimal duct due to a tumour adjacent to the inner canthus will result in a weeping eye (epiphora). There is evidence that this does not happen due to radiotherapy alone if it is carefully fractionated and the tumour has not comprised the function of the duct already. A dose of 45 Gy in 10 fractions on a superficial unit (100 kV) is the minimum fractionation recommended. Figures 31.4 (before radiotherapy) and 31.5 (after radiotherapy) illustrate a basal cell carcinoma in this region treated with superficial radiotherapy.
Principles of irradiation
Technique
For radical radiotherapy, patients are planned with the aid of a computed tomography (CT) scan. Paired wedged fields are usually most appropriate. A combination of three fields planned conformally may achieve a better isodose distribution for extensive tumours and reduce the dose to normal tissues (Figure evolve 31.6 ![]() ). A prescription to a dose of 54–60 Gy with 2 Gy daily treatments is commonly employed. Great attention should be paid to eye care and regular reviews should be performed by clinicians during the course of radiotherapy.
). A prescription to a dose of 54–60 Gy with 2 Gy daily treatments is commonly employed. Great attention should be paid to eye care and regular reviews should be performed by clinicians during the course of radiotherapy.