A. Normal study
B. Leiomyoma
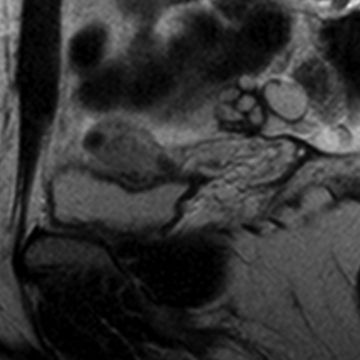
C. Adenomyosis
D. Endometrial cancer
E. Cesarean-section scar
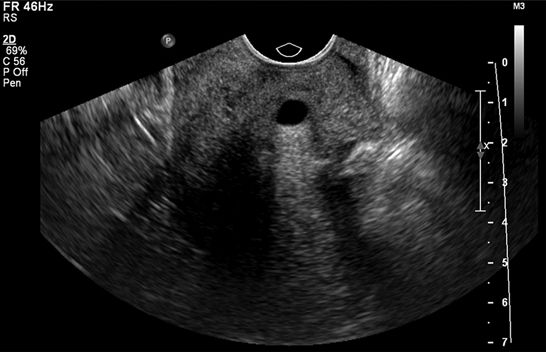
3 A 57-year-old female with postmenopausal bleeding undergoes a transvaginal ultrasound. How should the endometrial stripe measurement be made?
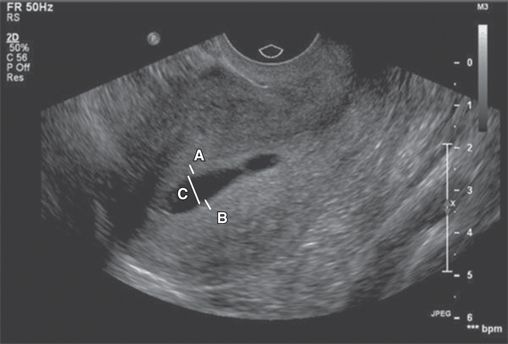
A. Line A + Line B
B. Line A + Line B + Line C
C. Line A + Line B − Line C
D. Line A
E. Line B
F. Line C
4 A 70-year-old female with postmenopausal bleeding undergoes a transvaginal pelvic ultrasound. What endometrial stripe measurement is an indication for endometrial biopsy?
A. ≥3 mm
B. ≥4 mm
C. ≥5 mm
D. ≥6 mm
5 A 22-year-old female with pelvic pain and a serum hCG of 1,200 mIU/mL undergoes a transvaginal pelvic ultrasound. The ovaries are normal, and no adnexal mass is identified. How should the imaging findings be reported?
A. Findings consistent with an intrauterine pregnancy, no follow-up required
B. Findings consistent with a pseudogestational sac, treat for ectopic pregnancy
C. Findings likely an intrauterine pregnancy, follow-up to confirm
D. Findings likely a pseudogestational sac, admit for possible ectopic pregnancy
6 A 28-year-old female with primary infertility undergoes a hysterosalpingogram. Which of the following maneuvers will reduce the radiation dose delivered to the patient?
A. Changing from 5 to 3 pulses per second
B. Placing a lead apron on the operator
C. Moving the image intensifier away from the patient
D. Opening the collimation
7 A 56-year-old female with pelvic pain undergoes a pelvic examination, and biopsy demonstrates cervical cancer. MRI of the pelvis is performed. What stage is this neoplasm?

A. Less than IIB
B. IIB or greater
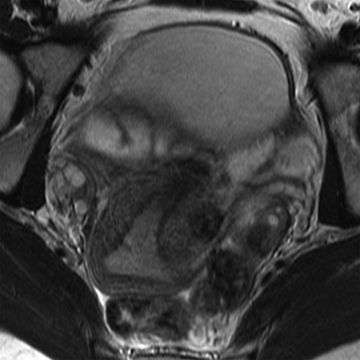
8 A 30-year-old female with menorrhagia undergoes a pelvic MRI. What junctional zone thickness is commonly used to indicate a high specificity for the diagnosis of adenomyosis?
A. >4 mm
B. >8 mm
C. >12 mm
D. >16 mm
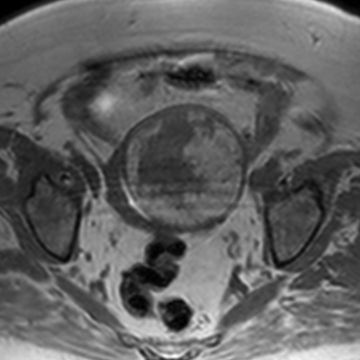
9 A 56-year-old female with postmenopausal bleeding undergoes a transvaginal ultrasound. What is the most likely diagnosis for the adnexal mass?
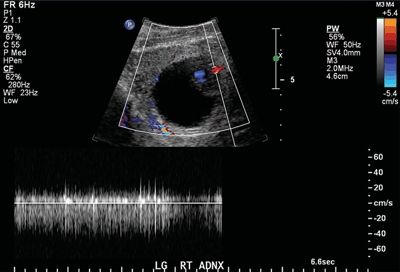

A. Cystadenocarcinoma
B. Granulosa cell tumor
C. Endometrioma
D. Immature teratoma
10 A 25-year-old female undergoes a pelvic MRI to evaluate for adenomyosis. How should the junctional zone thickness be measured?

A. Line A + Line B
B. Line A + Line B + Line C
C. Line A + Line C − Line B
D. Line A or Line C
11 A 60-year-old female with cervical cancer undergoes a pelvic MRI. According to the FIGO staging system, what stage is this neoplasm?
A. IIA
B. IIB
C. IIIA
D. IIIB
12 The cornerstone of cervical cancer staging with pelvic MRI is thin-section T2-weighted imaging without fat saturation angled to the short axis of the cervix. The pulse sequence commonly used for this purpose utilizes a multislice fast spin echo technique. Which of the following modifications would increase the image acquisition time required for this pulse sequence?
A. A reduction in the echo train length
B. An increase in the echo time
C. A reduction in the repetition time
D. An increase in the frequency-encoding matrix
13 A 22-year-old female with vaginal bleeding and a positive urine pregnancy test undergoes a pelvic ultrasound. A gestational sac is identified containing a yolk sac and a fetal pole. No fetal cardiac activity is detected. According to the Society of Radiologists in Ultrasound (SRU) 2012 guidelines, at what crown rump length size is absent fetal cardiac activity considered diagnostic of fetal loss?
A. ≥3 mm
B. ≥5 mm
C. ≥7 mm
D. ≥9 mm
14 A 32-year-old female with multiple uterine fibroids undergoes consultation for uterine artery embolization. She is deemed a suitable candidate. A preprocedure MRI is performed, and large bilateral corkscrew-shaped vessels are identified extending from the aorta to the uterus. Based on this finding, what is the best next step?
A. Uterine artery embolization is contraindicated.
B. Unilateral uterine artery embolization should be performed.
C. Bilateral uterine artery embolization should be performed.
D. Bilateral uterine and gonadal artery embolization should be performed.
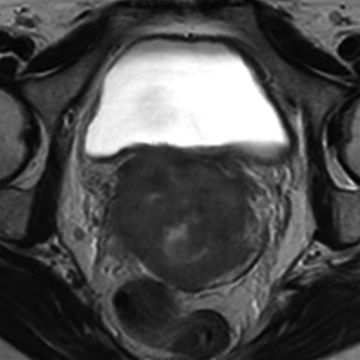
15 A 25-year-old female with primary infertility undergoes a pelvic MRI to assess for congenital anomalies. How should the images be interpreted?

A. Normal examination
B. Uterus didelphys
C. Bicornuate bicollis uterus
D. Septate uterus
16 A 55-year-old female with postmenopausal bleeding is diagnosed with endometrial cancer. A pelvic MRI is performed for staging, and the mass is shown to involve >50% of the myometrial thickness. There is no evidence of cervical, vaginal, nodal, or metastatic disease. According to the FIGO staging system, what is the clinical stage of this neoplasm?
A. IA
B. IB
C. II
D. IIIA
17 Which of the following has a classic association with a “T-shaped uterus”?
A. Diffuse adenomyosis
B. Exposure to a fetal carcinogen
C. Multifocal leiomyomata
D. Endometrial cancer
E. Pelvic inflammatory disease
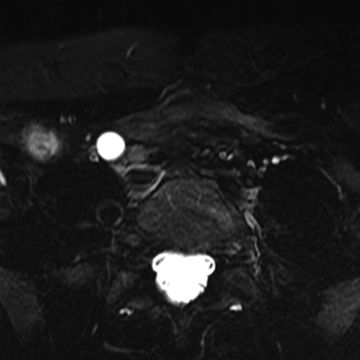
18 A 44-year-old female with pelvic pain undergoes a pelvic MRI, and a large mass is identified. What is the most likely diagnosis?
Axial T1w GRE

Axial T1w GRE

Axial T2w FSE
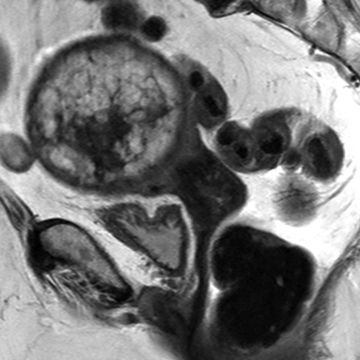
Sagittal T2w FSE
A. Leiomyoma
B. Dermoid
C. Endometrial cancer
D. Uterine sarcoma
19 A 30-year-old G0P0 female with vaginal bleeding and a serum hCG level of 200,000 mIU/mL undergoes a transvaginal ultrasound. What is the most likely diagnosis?

A. Retained products of conception
B. Gestational trophoblastic disease
C. Diffuse adenomyosis
D. Large intrauterine blood clots
20 A 64-year-old female with endometrial cancer presents for staging evaluation with MRI of the pelvis. What is the best pulse sequence for measuring the depth of myometrial invasion?
A. 3D T1w fat-saturated GRE postcontrast
B. 3D T1w fat-saturated GRE precontrast
C. 2D T2w FSE without fat saturation
D. 2D T2w FSE with fat saturation
21 A 30-year-old female with pelvic fullness undergoes a pelvic ultrasound. How should this fibroid be classified?

A. Intracavitary
B. Intramural
C. Pedunculated
D. Submucosal
E. Subserosal
22 A 30-year-old female with menorrhagia undergoes a transvaginal ultrasound, and a Nabothian cyst is identified. Which of the following contributes to the appearance of bright pixels deep to the cyst?

A. Attenuation correction artifact
B. Refraction artifact
C. Reverberation artifact
D. Side lobe artifact
23 A 24-year-old G4P3 female presents with secondary infertility. What is the most likely explanation for the appearance of the fundal endometrial canal?

A. Endometrial cancer
B. Adhesive disease
C. Fetal diethylstilbestrol exposure
D. Uterine fibroids
24 A 32-year-old female with secondary infertility undergoes a hysterosalpingogram. How should the imaging be interpreted?


A. Zero patent fallopian tubes
B. One patent fallopian tube
C. Two patent fallopian tubes
25 A 19-year-old female with pelvic pain undergoes a pelvic MRI. A unicornuate uterus with a rudimentary horn is diagnosed. How should the rudimentary horn be managed?

Left parasagittal T2W FSE
Right parasagittal T2W FSE
A. Operative resection
B. Hysteroscopic recanalization
C. Oral contraceptive pills
D. Endometrial ablation
26 A 40-year-old female with pelvic discomfort undergoes a pelvic ultrasound, and a large myometrial mass is identified. What is the most common way uterine leiomyosarcoma is differentiated from uterine leiomyoma?
A. Detecting intratumoral hemorrhage on T1-weighted images
B. Detecting rapid tumor growth over a short period of time
C. Retrospective histologic analysis after surgical removal
D. Prospective histologic analysis with percutaneous biopsy
27 A 67-year-old female with breast cancer on tamoxifen therapy undergoes a pelvic ultrasound for irregular bleeding. What endometrial thickness is considered an indication for endometrial biopsy in a postmenopausal woman receiving tamoxifen therapy?
A. ≥5 mm
B. ≥6 mm
C. ≥7 mm
D. ≥8 mm
A. Advance the catheter
B. Inject more contrast material
C. Pull back the catheter
D. Drain the contrast material
29 A 25-year-old female with primary infertility undergoes a hysterosalpingogram. What is the most likely explanation for the imaging findings?

A. Normal study
B. Congenital variant
C. Pelvic inflammatory disease
D. Pelvic mass
30 A 30-year-old female desiring sterility undergoes bilateral fallopian tube microinsert placement. She returns for a hysterosalpingogram to document microinsert position and tubal occlusion. What is the best explanation for the small collections of contrast material alongside the endometrial canal?

A. Normal variant
B. Fibroids
C. Venous intravasation
D. Endometrial cancer
E. Adenomyosis
Answers and Explanations
1 Answer B. In a woman with postmenopausal bleeding, further evaluation is required with endometrial biopsy or transvaginal ultrasound to assess for malignancy using the following algorithm:
- If an endometrial biopsy is performed first and yields diagnostic tissue, transvaginal ultrasound is not required.
- If a transvaginal ultrasound is performed first and the endometrial stripe is ≥5 mm, endometrial biopsy is required.
- If a transvaginal ultrasound is performed first and the endometrial stripe is <5 mm, endometrial biopsy is not required.
An endometrial stripe measurement ≤4 mm in the setting of postmenopausal bleeding has a negative predictive value >99% for endometrial cancer. Therefore, transvaginal ultrasound can serve as a triage tool to determine which patients with postmenopausal bleeding require endometrial biopsy.
References: Karlsson B, Granberg S, Wikland M, et al. Transvaginal ultrasound of the endometrium in women with postmenopausal bleeding—a Nordic multicenter study. Am J Obstet Gynecol 1995;172:1488–1494.
The American Congress of Obstetricians and Gynecologists. The role of transvaginal ultrasonography in the evaluation of postmenopausal bleeding. The American Congress of Obstetricians and Gynecologists (ACOG) Committee Opinion 440. 2009 and 2013.
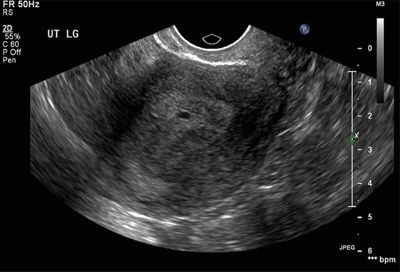
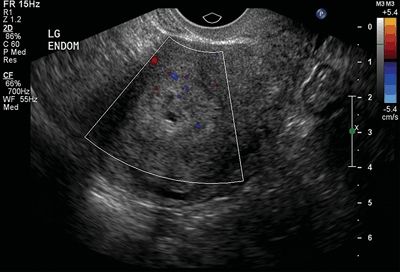
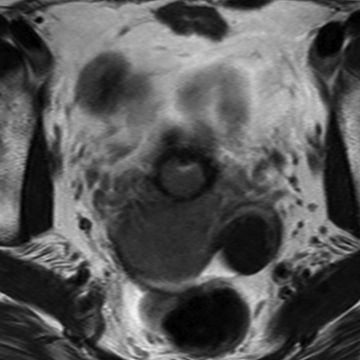
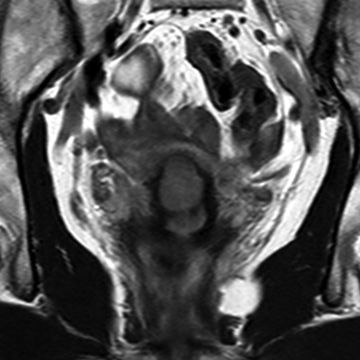
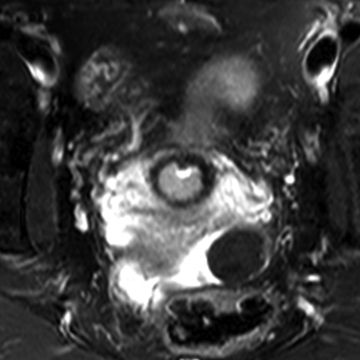
2 Answer C. The image demonstrates a diffusely thickened junctional zone compatible with adenomyosis. A junctional zone measurement >12 mm is specific for the diagnosis. A junctional zone measurement 9 to 12 mm is equivocal for adenomyosis, and a junctional zone measurement ≤8 mm is normal. The diagnosis of adenomyosis is important because adenomyosis is more resistant to catheter-directed embolic treatment compared to fibroids, the operative approach for fibroids and adenomyosis differs, and diffuse adenomyosis can be mistaken for malignancy on imaging.
The imaging findings of fibroids (Answer B) can overlap with those of adenomyosis, but fibroids are typically more well defined with circumscribed margins. Adenomyosis tends to be a diffuse process though focal adenomyomas do occur. Endometrial cancer (Answer D) is not the best choice because the endometrium is normal. A cesarean-section scar (Answer E) would be inferiorly located along the anterior lower uterine segment and would manifest as a thin signal abnormality associated with myometrial volume loss.
References: Popovic M, Puchner S, Berzaczy D, et al. Uterine artery embolization for the treatment of adenomyosis: a review. J Vasc Interv Radiol 2011;22:901–909.
Shwayder J, Sakhel K. Imaging for uterine myomas and adenomyosis. J Minim Invasive Gynecol 2013;21(3):362–376.
Stamatopoulos CP, Mikos T, Grimbizis GF, et al. Value of magnetic resonance imaging in diagnosis of adenomyosis and myomas of the uterus. J Minim Invasive Gynecol 2012;19:620–626.
3 Answer A. The endometrial stripe should be measured in the long-axis view of the uterus during transvaginal scanning. It should encompass the maximum anteroposterior thickness of the endometrium including the anterior and posterior layers and excluding any endometrial fluid. Inaccurate measurement technique can result in an over- or underestimation of the true endometrial thickness and lead to inappropriate management.
References: Davidson KG, Dubinsky TJ. Ultrasonographic evaluation of the endometrium in postmenopausal vaginal bleeding. Radiol Clin North Am 2003;41:769–780.
The American Congress of Obstetricians and Gynecologists. The role of transvaginal ultrasonography in the evaluation of postmenopausal bleeding. The American Congress of Obstetricians and Gynecologists (ACOG) Committee Opinion 440. 2009 and 2013.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree