A. Superior-to-inferior
B. Inferior-to-superior
C. Right-to-left
D. Left-to-right
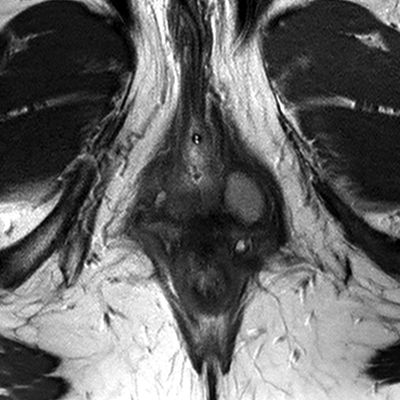
2 A 50-year-old female undergoes a pelvic MRI, and chemical shift artifact of the first kind is identified along the margins of an ovarian cyst. Assuming a receiver bandwidth of ±64 kHz (128 kHz) and a frequency matrix size of 128, what is the expected size of the pixel shift at 1.5 Tesla?
A. 0.2 pixels
B. 0.4 pixels
C. 2.0 pixels
D. 4.0 pixels
3 A 22-year-old female with right lower quadrant pain undergoes a contrast-enhanced CT of the abdomen and pelvis. What is the most likely cause of the dominant abnormality?


A. Infection
B. Ischemia
C. Inflammation
D. Malignancy
4 A 32-year-old G1P1 female presents with secondary infertility. Which of the following best characterizes the role of ultrasound in the diagnosis of polycystic ovary syndrome (PCOS)?
A. Numerous bilateral ovarian cysts are a highly sensitive marker of PCOS.
B. Numerous bilateral ovarian cysts are a highly specific marker of PCOS.
C. Ultrasound has only a supportive role in the diagnosis of PCOS.
D. Ultrasound has no role in the diagnosis of PCOS.
5 Why is STIR never used for fat suppression in T1-weighted contrast-enhanced pulse sequences?
A. Gadolinium variably shortens T1, resulting in unpredictable tissue suppression.
B. Gadolinium variably shortens T2, resulting in unpredictable tissue suppression.
C. Fat protons are not affected by the 180-degree inversion pulse.
D. Fat protons are not affected by the 90-degree inversion pulse.
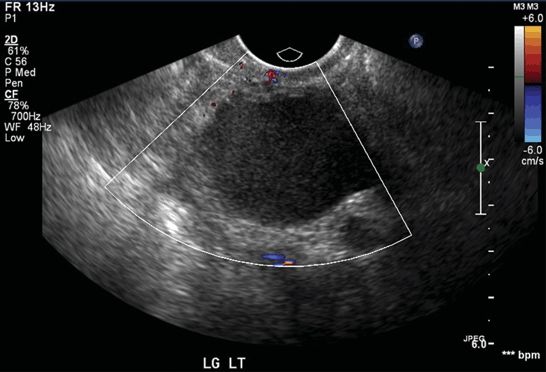
6 A 38-year-old female with a negative urine pregnancy test and recurrent left lower quadrant pain undergoes a pelvic ultrasound with color Doppler imaging. A 3.5-cm abnormality is identified in the left ovary. Her symptoms persist, and follow-up ultrasound performed 2 months later is unchanged. What is the best next step?
A. Further imaging: follow-up ultrasound in 2 months
B. Further imaging: contrast-enhanced pelvic MRI now
C. Percutaneous biopsy
D. Cystectomy performed by a gynecologist
E. Cystectomy performed by a gynecology oncologist
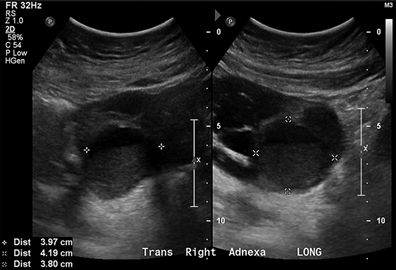
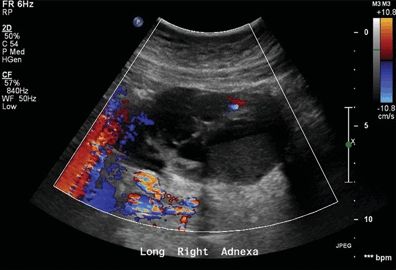
7 A 28-year-old female with fever, leukocytosis, and adnexal pain undergoes a pelvic ultrasound. The serum bHCG level is 0 mIU/mL. What is the best next step?
A. Ignore (benign finding)
B. Imaging follow-up
C. Intravenous antibiotic therapy
D. Intravenous antibiotic therapy and drainage
E. Surgical resection
8 The management of asymptomatic ovarian and adnexal cysts is in part dependent on whether a cyst is detected in a premenopausal or a postmenopausal patient. What is the definition of postmenopause in patients who have not had a hysterectomy?
A. Two cycles of amenorrhea after the age of 50 years
B. Six cycles of amenorrhea from the last menstrual period
C. One year of amenorrhea from the last menstrual period
D. One year of amenorrhea after the age of 50 years
9 A 32-year-old female with no past medical history undergoes a transvaginal pelvic ultrasound for menorrhagia. A 3.5-cm left adnexal cyst is identified. The patient has no pelvic pain. How should this finding be dictated in the radiologist’s report?


A. The finding should not be mentioned.
B. The finding is likely benign with no follow-up recommended.
C. The finding is likely benign with 1-year follow-up recommended.
D. The finding is possibly malignant with 1-year follow-up recommended.
E. The finding is possibly malignant with surgical consultation recommended.
10 A 72-year-old female with no past medical history undergoes a transvaginal pelvic ultrasound for postmenopausal bleeding. A 3.5-cm simple left adnexal cyst is identified. The patient has no pelvic pain. How should this finding be dictated in the radiologist’s report?
A. The finding should not be mentioned.
B. The finding is likely benign with no follow-up recommended.
C. The finding is likely benign with 1-year follow-up recommended.
D. The finding is possibly malignant with 1-year follow-up recommended.
E. The finding is possibly malignant with surgical consultation recommended.
11 A 40-year-old female undergoes a transvaginal ultrasound, and a cystic adnexal mass is identified. A repeat study performed 2 months later shows no interval change. Which of the following imaging findings most strongly suggests a malignant etiology?
A. Two 4-mm-thick septations
B. Diffuse low-level internal echoes
C. Tubular configuration with a “waist sign”
D. Solid-appearing area with concave margins and no internal flow
12 A 35-year-old female with lower abdominal pain undergoes a contrast-enhanced CT of the abdomen and pelvis. A 6-cm mass is identified in the left pelvis. What is the most likely diagnosis?

A. Mature cystic teratoma
B. Immature teratoma
C. Liposarcoma
D. Lipoma
13 A 22-year-old female with pelvic inflammatory disease complicated by infected peritoneal fluid presents for transgluteal catheter drainage. Of the following routes of access, which is most likely to result in successful drainage with the least risk of complication?
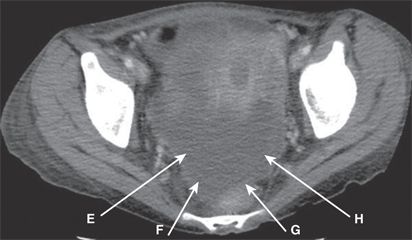
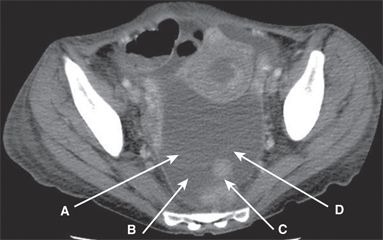
A. A
B. B
C. C
D. D
E. E
F. F
G. G
H. H
14 In utero diethylstilbestrol exposure has a strong association with which of the following malignancies?
A. Uterine sarcoma
B. Endometrial adenocarcinoma
C. Vaginal clear cell adenocarcinoma
D. Ovarian carcinosarcoma
15 Which of the following is a risk factor for Actinomyces israelii infection of the fallopian tubes?
A. Unprotected sexual intercourse
B. Intrauterine device placement
C. Oral contraceptive use
D. Uterus didelphys
16 A 32-year-old G2P2 female undergoes hysteroscopic placement of bilateral fallopian tube occlusion devices. Three months later, a hysterosalpingogram is performed. How should the resulting imaging be interpreted?

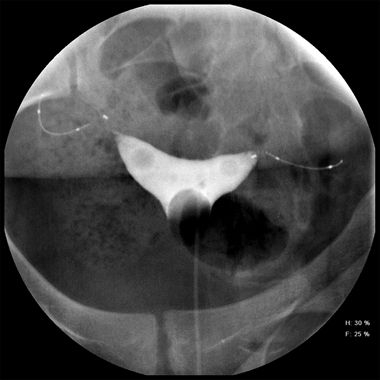
A. Normal device position, bilateral tubal occlusion
B. Normal device position, insufficient tubal occlusion
C. Abnormal device position, bilateral tubal occlusion
D. Abnormal device position, insufficient tubal occlusion
17 A 40-year-old G1P1 female who recently immigrated to the United States from a third-world country presents with incontinence. She has no known surgical or cancer history, and a pelvic examination is normal. A cystogram is performed, and a vesicovaginal fistula is identified. Which of the following risk factors best explains the imaging findings?
A. Multistrain human papillomavirus infection
B. Recurrent Clonorchis sinensis infection
C. Childbirth complicated by prolonged labor
D. Low-fiber, high-carbohydrate diet
18 A 57-year-old female presents with vaginal cancer. What is the most common cell type and risk factor for vaginal cancer in the United States?
A. Squamous cell carcinoma; pelvic radiation therapy
B. Squamous cell carcinoma; human papillomavirus infection
C. Adenocarcinoma; in utero diethylstilbestrol exposure
D. Adenocarcinoma; Chlamydia trachomatis infection
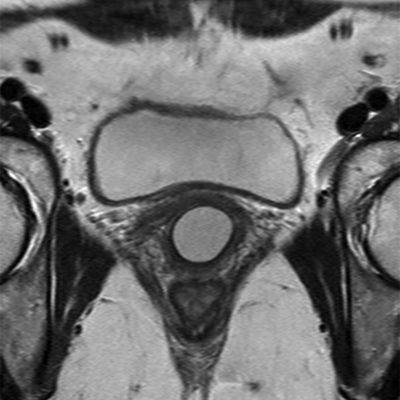
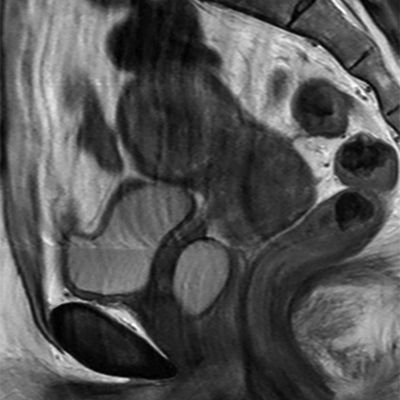
19 A 50-year-old female with pelvic discomfort undergoes a pelvic MRI, and a left ovarian mass is identified. Other images (not shown) reveal bilateral pleural effusions and ascites. Her serum CA-125 level is elevated. The following images are representative of the entire ovarian mass. Which of the following best characterizes this patient’s prognosis and expected treatment course?
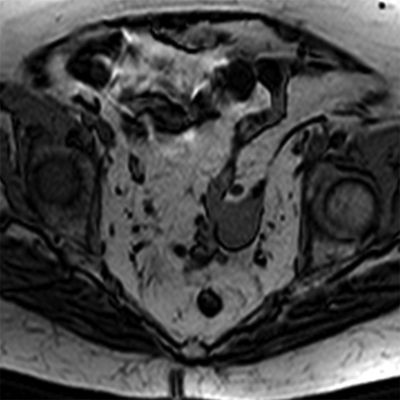
Axial T1w GRE with fat saturation
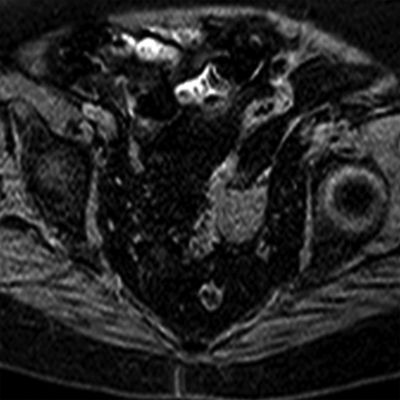
Axial T1w GRE with fat saturation postcontrast
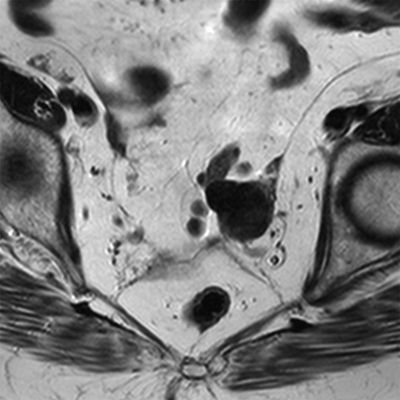
Axial T1w GRE
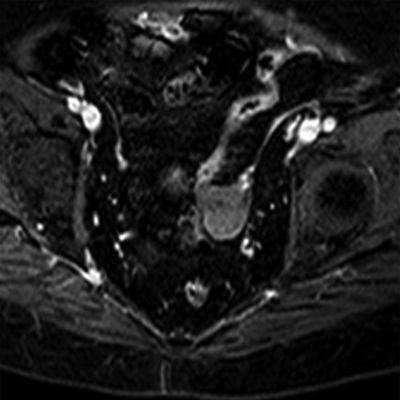
Axial T2w FSE
A. Excellent prognosis following systemic chemotherapy
B. Excellent prognosis following ipsilateral oophorectomy
C. Dismal prognosis despite systemic chemotherapy
D. Dismal prognosis despite ipsilateral oophorectomy
20 A 55-year-old female requests information about the combined use of serum CA-125 and transvaginal ultrasound for ovarian cancer screening. Which of the following statements best summarizes the current consensus on ovarian cancer screening in average-risk patients?

A. Neither CA-125 nor pelvic ultrasound is effective for screening average-risk patients.
B. CA-125 is effective for screening average-risk patients, but pelvic ultrasound is not.
C. Pelvic ultrasound is effective for screening average-risk patients, but CA-125 is not.
D. CA-125 and pelvic ultrasound are effective for screening average-risk patients but only in combination.
21 A senior investigator at a major academic institution is interested in detecting new treatments for ovarian carcinomatosis. He plans to make thickness measurements of the omental cake by CT in affected patients 1, 3, 6, and 12 months after the initial laparoscopic diagnosis in the absence of intercurrent systemic therapy. He plans to use this information as a control against which he can compare the effect of novel therapeutic agents. However, most patients with ovarian carcinomatosis at his institution receive standard-of-care systemic therapy, so he is having difficulty identifying a control group for his study. Which of the following approaches is most appropriate?
A. He should ask his gynecology colleagues to delay systemic chemotherapy for at least 12 months in patients newly diagnosed with ovarian cancer, and then use this group as his control.
B. He should randomize patients newly diagnosed with ovarian cancer to receive either standard-of-care systemic therapy or no therapy for 12 months, and then use the “no therapy” group as his control.
C. He should instead contrast the growth rate of ovarian carcinomatosis in the setting of one IND- and IRB-approved novel therapeutic agent against that of another IND- and IRB-approved novel therapeutic agent.
D. He should instead contrast the growth rate of ovarian carcinomatosis in the setting of standard-of-care systemic therapy against that of an IND- and IRB-approved novel therapeutic agent.
22 A 24-year-old female presents for MR imaging of the pelvis after her primary care physician discovered an ovoid soft palpable mass. What is the most likely diagnosis?
A. Bartholin gland cyst
B. Gartner duct cyst
C. Urethral diverticulum
D. Skene gland cyst
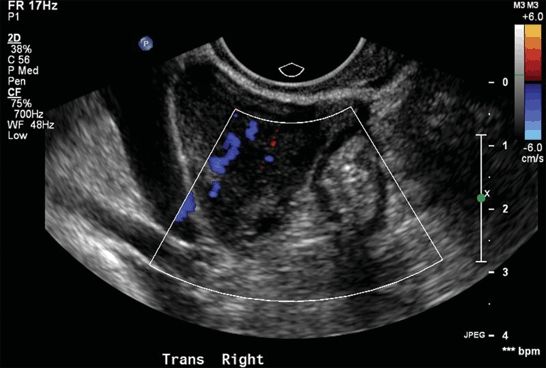
23 A 25-year-old female with right lower quadrant pain undergoes a transvaginal ultrasound to “rule out torsion.” Her right ovary measures 2 × 3 × 2 cm, and her left ovary measures 2 × 3 × 2 cm. How should the images be interpreted?
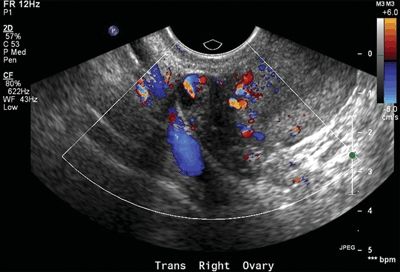
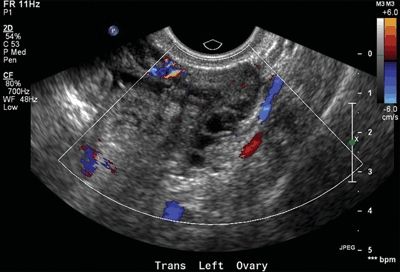
A. Normal ovaries; the apparent diminished flow in the left ovary is likely technical.
B. There is diminished flow in the left ovary that is equivocal for ovarian torsion.
C. There is diminished flow in the left ovary consistent with acute ovarian torsion.
D. There is diminished flow in the left ovary consistent with chronic ovarian torsion.
24 A 22-year-old female with right lower quadrant pain and a positive pregnancy test undergoes a transvaginal ultrasound. Which of the following is a risk factor for tubal ectopic pregnancy?
A. Human papillomavirus infection
B. Neisseria gonorrhoeae infection
C. Prior uncomplicated vaginal delivery
D. Prior uncomplicated cesarean section
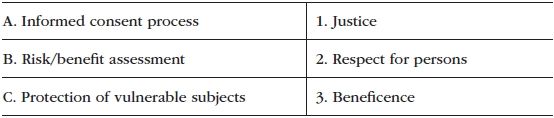
25 A young investigator is designing a clinical trial comparing two imaging modalities for cervical cancer staging. Prior to Institutional Review Board submission, she is required to attest that she will conduct her research in an ethical fashion. Match the following research practices (lettered) with the appropriate guiding ethical principle (numbered) as outlined in the Belmont Report.
26 A 28-year-old female with hypotension and severe pelvic pain presents for pelvic ultrasound. A urine beta-HCG is positive, and no normal pregnancy is identified. If this patient has an ectopic pregnancy, where is it most likely to be located?
A. Uterus
B. Fallopian tube
C. Ovary
D. Cul-de-sac
E. Cervix
27 A 24-year-old female presents for MR imaging of the pelvis after her primary care physician discovered an ovoid soft palpable mass. What is the most likely diagnosis?
A. Bartholin gland cyst
B. Gartner duct cyst
C. Urethral diverticulum
D. Skene gland cyst
28 A 24-year-old female with primary infertility undergoes a hysterosalpingogram for tubal evaluation. Which of the following best explains the imaging findings?
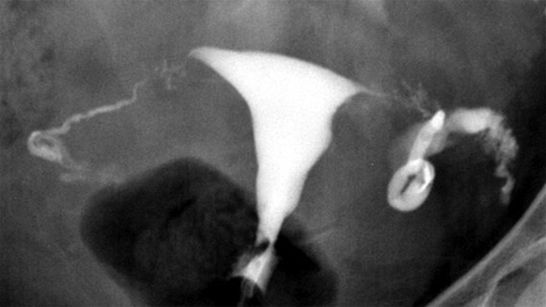
A. Normal study
B. Prior Chlamydia trachomatis infection
C. Congenital mesonephric duct abnormality
D. Fetal diethylstilbestrol exposure
29 A 40-year-old female with chronic pelvic pain undergoes a transvaginal pelvic ultrasound. A repeat study performed 2 months later shows persistent findings. What is the most likely diagnosis?
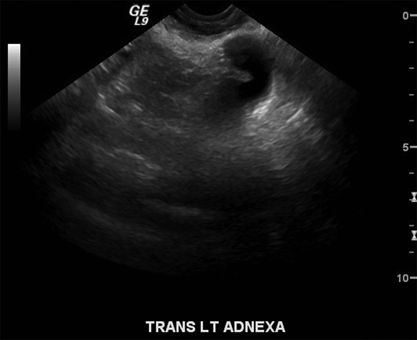
A. Ovarian serous cystadenoma
B. Ovarian mucinous adenocarcinoma
C. Hydrosalpinx
D. Endometrioma
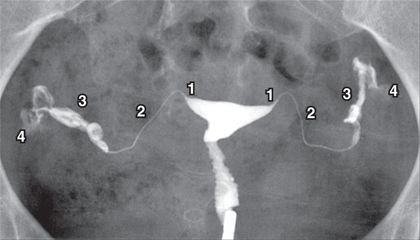
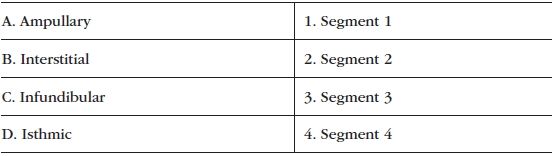
30 The fallopian tube is composed of four major segments. Match the segments of the fallopian tube (lettered) with the labels shown in the figure (numbered).
Answers and Explanations
1 Answer A. The frequency-encoding gradient in this image increases from superior to inferior. This cyst in the center of the image demonstrates chemical shift artifact of the first kind along the superior and inferior margins; with this artifact, the spatial mapping of fat is erroneously shifted relative to water. Chemical shift artifact only occurs along the frequency-encoding axis. Therefore, Answer C and Answer D are incorrect. The black line where fat pixels were shifted away from the wall of the cyst is along the superior margin, and the white line into which pixels were shifted from fat into the cyst is along the inferior margin. This indicates that the frequency-encoding gradient increases from superior to inferior (from the black line toward the white line). An explanation of this is provided below. Chemical shift artifact of the first kind occurs along fat–fluid and fat–tissue interfaces. The width of the artifact increases with increasing field strength and lower receiver bandwidth.
Spatial location along the frequency-encoding axis is determined by precessional frequency. The frequency-encoding gradient assigns protons along each line of the frequency-encoding axis a unique precessional frequency that can be used later to determine its spatial location. Because fat protons do not precess at the same frequency as do water protons, the mapping is erroneous, with the slower fat protons being erroneously shifted downward along the frequency-encoding gradient (slower precession frequency than expected). Look at the graph below and imagine that the x-axis voxels labeled “water” represent the cyst from the image, and the x-axis voxels labeled “fat” represent the adjacent fat from the image. The y-axis is gradient frequency; two different frequency-encoding gradients are shown as red and blue lines. These lines show the frequencies assigned (by position) to the different voxels.
The graph shows that the steepness of the frequency-encoding gradient is a reflection of the width of the receiver bandwidth. The receiver bandwidth is basically the range of frequencies encoded by the frequency-encoding gradient for a given matrix size. Therefore, a higher receiver bandwidth (e.g., the red line, steep slope) will be less affected by a small frequency shift (e.g., 220 Hz at 1.5 Tesla) because the shift may occur entirely within a single voxel. Choose a spot on the red line and trace backward 220 Hz using the y-axis. Notice that this new position may remain within the same voxel. As the receiver bandwidth decreases (e.g., blue line), the shift will cross voxels, moving signal intensity contributed by fat from one voxel into another. Choose a spot on the blue line and trace backward 220 Hz using the y-axis. Notice that this new position will be within a different voxel.
The direction of the chemical shift of the fat protons will be from high to low frequency because fat protons precess slower than do water protons. Therefore, the fat–water interface at the high end of the gradient will experience a shift of fat protons into the cyst (creating a bright band of added signal), and the fat–water interface at the low end of the gradient will experience a shift of fat protons away from the cyst (creating a black band of absent signal). Why not always maximize the receiver bandwidth? High receiver bandwidths have more noise per pixel. Therefore, high receiver bandwidths come at the cost of reduced SNR (signal-to-noise ratio).

References: Kamel IR, Merkle EM. Body MR Imaging at 3 Tesla, 1st ed. New York: Cambridge University Press, 2011.
Mamourian AC. Practical MR physics, 1st ed. New York: Oxford University Press, 2010.
McRobbie DW, Moore EA, Graves MJ, et al. MRI: from picture to proton, 2nd ed. New York: Cambridge University Press, 2007.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree