Abstract
The female pelvis can be difficult to evaluate on FDG PET/CT. The endometrium and ovaries may demonstrate physiologic FDG avidity. Benign leiomyomata of the myometrium may be FDG avid. And physiologic FDG avidity in the adjacent bowel and urinary tract may obscure FDG-avid ovarian or uterine lesions. Nevertheless, FDG PET/CT has demonstrated value for detecting unsuspected nodal and distant metastases in ovarian and uterine malignancies, as well as for evaluation of treatment response and detection of recurrent malignancy.
Keywords
FDG, PET/CT, ovary, uterus, myometrium, endometrium, cervix, ovarian cancer, transposed ovary, leiomyomata, leiomyosarcoma
The female pelvis can be difficult to evaluate on 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT). The endometrium and ovaries may demonstrate physiologic FDG avidity. Benign leiomyomata of the myometrium may be FDG avid. In addition, physiologic FDG avidity in the adjacent bowel and urinary tract may obscure FDG-avid ovarian or uterine lesions. Nevertheless, FDG PET/CT has demonstrated value for detecting unsuspected nodal and distant metastases in ovarian and uterine malignancies, as well as for evaluation of treatment response and detection of recurrent malignancy.
Physiologic FDG Avidity in the Female Reproductive Tract
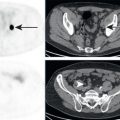
Physiologic FDG avidity has been observed in the endometrium, fallopian tubes, and ovaries. In premenopausal women, FDG avidity in the endometrium is most likely physiologic ( Fig. 19.1 ). Likewise, in premenopausal women, FDG avidity in the ovary/adnexa is likely physiologic ( Fig. 19.2 ). Physiologic FDG avidity in the adnexa may be unilateral or bilateral. In studies with intravenous contrast, a corresponding ring of enhancement may be seen in the adnexa, representing a corpus luteum cyst ( Fig. 19.3 ). Corpus luteum cysts often demonstrate physiologic FDG avidity. Physiologic FDG avidity is also expected in the adnexa of patients who have undergone ovarian hyperstimulation for oocyte retrieval ( Fig. 19.4 ). Hyperstimulated ovaries may be seen on CT as enlarged adnexa with multiple low-attenuation cystic lesions separated by soft tissue septae. In young women with pelvic malignancy, beware of surgically transposed ovaries with physiologic FDG avidity in unexpected locations. If radiation is planned for the pelvis, the ovaries may be surgically transposed to remove them from the radiation port, to preserve their function and fertility ( Fig. 19.5 ). Transposed ovaries may be unilateral or bilateral. In some cases, adjacent surgical clips will provide evidence of transposed ovaries.





Ovary
Ovarian Cancer
Ovarian cancer is one of the most common gynecologic malignancies. The primary malignancy in the adnexa has direct communication with the peritoneum and direct spread with peritoneal disease is common. Ovarian cancer may also demonstrate lymphatic spread to lymph nodes and hematogenous spread to multiple organ systems. Most patients are usually diagnosed with advanced disease. Disease burden in ovarian cancer may be followed by tumor markers in the serum, as well as by imaging.
The imaging techniques of choice for visualizing and local staging of a primary ovarian malignancy are ultrasound and magnetic resonance (MR). FDG PET/CT may complement these imaging modalities through the detection of FDG avidity in the adnexa. Although FDG avidity in the adnexa of premenopausal patients is often physiologic, FDG avidity in the adnexa or postmenopausal patients is abnormal and may prompt further workup ( Fig. 19.6 ). There is no standardized uptake value (SUV) threshold to distinguish malignant from benign adnexal lesions; however, in general, malignant adnexal lesions demonstrate greater FDG avidity.

The imaging technique of choice for visualization and staging of nodal and distant metastases from ovarian malignancy is contrast-enhanced CT. Peritoneal carcinomatosis may be visualized as increased peritoneal opacities on CT. Lymphatic spread of ovarian cancer is most common to the pelvic and retroperitoneal nodes; however, extension to the inguinal and thoracic nodes also occurs, and enlarged nodes in any of these nodal basins may be suspicious for nodal metastases. Distant metastases involve multiple organ systems, most commonly lung, bone, and liver. FDG PET/CT may complement contrast-enhanced CT by detection of unsuspected FDG-avid metastases, such as nodal metastases or implants which are subcentimeter in size and thus overlooked on anatomic imaging ( Fig. 19.7 ). The vaginal cuff is a common site of malignancy recurrence following hysterectomy. Postsurgical changes at the vaginal cuff may obscure recurrent malignancy at this location on CT but may be more readily appreciated on FDG PET ( Fig. 19.8 ). Peritoneal implants may be visible on CT, FDG PET, both, or neither. Small peritoneal implants are difficult to visualize on current imaging modalities and may only be identified during surgical exploration. It is important to remember that peritoneal reflections along the liver surface, such as the falciform ligament, may be involved with peritoneal malignancy. Implants along peritoneal reflections should be recognized as peritoneal malignancy, rather than hepatic parenchymal disease ( Fig. 19.9 ). Patients with hepatic parenchymal disease have a worse prognosis than do patients with disease along peritoneal reflections. There is evidence that FDG PET can predict response to systemic therapy of ovarian cancer metastases. Following treatment, FDG PET/CT may have higher sensitivity for detecting recurrent malignancy than serum tumor markers such as cancer antigen 125 or CT alone.