Abnormalities of the fetal head and neck may be seen in isolation or in association with central nervous system abnormalities, chromosomal abnormalities, and syndromes. Magnetic resonance imaging (MRI) plays an important role in detecting associated abnormalities of the brain as well as in evaluating for airway obstruction that may impact prenatal management and delivery planning. This article provides an overview of the common indications for MRI of the fetal head and neck, including abnormalities of the fetal skull and face, masses of the face and neck, and fetal goiter.
- •
Magnetic resonance imaging (MRI) is an useful adjunct to ultrasound in the work-up of fetal head and neck pathology. It is a safe and effective imaging modality for which there have been no proven harmful effects to the developing human fetus from limited exposure.
- •
Common indications for fetal head and neck imaging include: lymphatic malformation, teratoma, hemangioma, facial cleft, and goiter.
- •
MRI can be helpful in assessing airway obstruction, which may impact prenatal management and delivery planning.
- •
Cleft lip/palate represents the most common anomaly of the fetal face. A midline defect should prompt one to carefully scrutinize the intracranial contents, as there is an increased association with holoprosencephaly.
- •
Micrognathia is rarely an isolated finding and when detected on fetal MRI, it may serve as the initial clue that the fetus has an underlying syndrome or genetic abnormality.
Introduction
Over the last 3 decades, magnetic resonance imaging (MRI) has become an useful adjunct to ultrasound in the work-up of fetal head and neck pathology. MRI is particularly important in cases where there is concern for airway compromise, as clear delineation of fetal anatomy is crucial, particularly if fetal or perinatal interventional procedures are being considered and for scheduling and deciding on type of delivery. Additionally, given the high association of fetal head and neck pathology and concomitant central nervous system (CNS) abnormalities, MRI allows for detailed structural evaluation of the brain for detecting coexisting pathology and to assess for any intracranial extension of extracranial disease processes. MRI is not limited by the ossified calvarium and skull base, as is the case with ultrasound, particularly later in gestation. Lastly MRI, with its multiplanar imaging ability and high signal-to-noise ratio, provides superior delineation of the anatomically complex areas such as the floor of the mouth and deep neck spaces.
The focus of this article is on the evaluation of fetal head and neck pathology using MRI.
Safety of fetal MRI
Since the inception of fetal MR imaging in the early 1980s there have been no proven harmful effects to the developing human fetus from limited exposure to the changing electromagnetic fields occurring during MRI. Several studies have failed to demonstrate any adverse long-term effects on children who were imaged as fetuses. MRI is a safe and effective imaging modality for further characterizing fetal anomalies that are limited in their assessment by sonography alone.
Given the lack of conclusive data documenting deleterious effects of MRI at 1.5 T, the current guidelines by the American College of Radiology do not stipulate any special consideration regarding MRI of the fetus at any stage of pregnancy. However, in the United States, fetal MRI is generally not performed in the first trimester of gestation given the theoretical concern for teratogenesis. Furthermore, it is difficult to acquire high-quality images in very young fetuses by MRI.
Use of intravenous contrast in MRI in pregnancy is a relative contraindication. Gadolinium crosses the placenta and is considered a pregnancy class C drug (ie, gadolinium administration during pregnancy has not been proven to be completely safe in people).
Safety of fetal MRI
Since the inception of fetal MR imaging in the early 1980s there have been no proven harmful effects to the developing human fetus from limited exposure to the changing electromagnetic fields occurring during MRI. Several studies have failed to demonstrate any adverse long-term effects on children who were imaged as fetuses. MRI is a safe and effective imaging modality for further characterizing fetal anomalies that are limited in their assessment by sonography alone.
Given the lack of conclusive data documenting deleterious effects of MRI at 1.5 T, the current guidelines by the American College of Radiology do not stipulate any special consideration regarding MRI of the fetus at any stage of pregnancy. However, in the United States, fetal MRI is generally not performed in the first trimester of gestation given the theoretical concern for teratogenesis. Furthermore, it is difficult to acquire high-quality images in very young fetuses by MRI.
Use of intravenous contrast in MRI in pregnancy is a relative contraindication. Gadolinium crosses the placenta and is considered a pregnancy class C drug (ie, gadolinium administration during pregnancy has not been proven to be completely safe in people).
Technical aspects
Various types of coils can be used for fetal MRI. A body coil alone or a body phased-array coil in combination with a surface coil situated on the mother’s abdomen is commonly used. Images are acquired in the sagittal, axial, and coronal planes relative to the fetal facial profile. At the authors’ institution, the half-Fourier single-shot turbo spin-echo (HASTE) sequence serves as the mainstay of MRI of the fetus. HASTE sequences provide heavily T2-weighted (T2W) images with low susceptibility weighting in a very short time, enabling good discrimination of fetal facial features. Sequential slice capability and interleaving allows for high-quality imaging despite fetal movement. Susceptibility weighted sequences such as extremely rapid gradient echo, echo planar imaging (EPI) are very useful in the detection of hemorrhage and mineralization, and thus help in characterizing and in distinguishing head and neck masses such as lymphatic malformations, teratomas, and congenital hemangiomas/vascular malformations. T1-weighted (T1W) images have limited utility in the evaluation of fetal head and neck pathology apart from certain specific scenarios such as fetal goiter and in cases of large hemorrhages. Cine imaging is routinely acquired in fetal head and neck imaging, as it is useful in assessing the swallowing mechanism and patency of the aerodigestive tract.
As stated previously, images are acquired in 3 orthogonal planes with respect to the fetal face. Similar to postnatal life, the sagittal view provides a good evaluation of the fetal profile, including the frontal and nasal bones, hard palate, tongue, and mandible. Coronal images are useful in assessing the integrity of the fetal lips and palate as well as providing delineation of the eyes, nose, and ears. Axial images help assess the different compartments of the neck and are also valuable in evaluating the fetal facial structures and variations in cranial morphology.
Many congenital anomalies of the head and neck are associated with concomitant abnormalities of the fetal spine, heart, kidneys, or limbs and digits. Careful inspection of the visualized portions of the fetal body during a head and neck examination may provide additional information to suspect an underlying syndrome, sequence, or association.
On average, a routine fetal neuroimaging examination takes approximately 30 to 40 minutes. At the authors’ institution, no sedation is provided to the mother of the fetus.
Indications for fetal head and neck imaging
MRI of the fetal head and neck is primarily used as a problem-solving technique when fetal anomalies cannot be completely assessed with sonography. MRI is not used as a screening tool. Common indications for fetal head and neck imaging include: lymphatic malformation, teratoma, hemangioma, facial cleft, and goiter. Other less common indications include abnormal shape of cranium, scalp, jaw, and orbital anomalies. As described previously, MRI can be helpful in assessing airway obstruction, which may impact prenatal management and delivery planning.
Abnormal calvarium
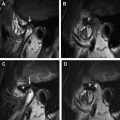
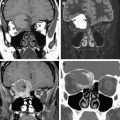
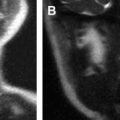
Abnormalities of the fetal skull can be related to calvarial size, shape, and mineralization. There are many causes for an abnormal fetal skull size and shape. Macrocephaly is a common presentation on fetal MRI, often related to an underlying abnormality such as hydrocephalus, abnormal development ( Fig. 1 A), intracranial tumor (see Fig. 1 B), or megalencephaly. Microcephaly can be seen with various syndromes and malformations ( Fig. 2 A, B) and can also be caused by volume loss or brain destruction secondary to infection, ischemia, and hemorrhage. An abnormal fetal skull shape may be related to a variety of causes, many of which have an underlying genetic mutation. Loss of subarachnoid space and collapse of the calvarial bones around the brain produce a characteristic lemon shape that is seen with neural tube defects. A triangular strawberry-shaped configuration to the head is associated with trisomy 18. Spalding’s sign ( Fig. 3 A, B) refers to overlapping of calvarial bones as the brain collapses following fetal demise. The fetal head may also become deformed in cases of severe oligohydramnios or anhydramnios.
The craniosynostoses refer to a collection of disorders all characterized by premature fusion of 1 or more cranial sutures resulting in inhibition of calvarial growth at right angles to the fused suture ( Fig. 4 A, B). This leads to characteristic morphology of both the calvarium and the face. Both syndromal and nonsyndromal forms of craniosynostosis exist. In the context of syndromal craniosynostoses, often times other skeletal findings may help make the prenatal diagnosis. Apert syndrome ( Fig. 5 ) is a craniofacial dysostosis characterized by coronal craniosynostosis plus or minus other sutures, midface hypoplasia, and syndactyly of the hands and feet (mitten hands).
Scalp masses
Causes of fetal scalp masses are many and varied. The most common causes include hemangioma ( Fig. 6 ), lymphatic malformation, and congenital inclusion cysts. Fetal MRI plays an important role in cases where there is concern for a cephalocele both in the confirmation of the calvarial defect, which sometimes may be falsely detected on sonography due to scanning angle, as well as to define the intracranial anatomy in cases of true calvarial defects ( Fig. 7 ). A clue to the fact that one may be dealing with a cephalocele or an atretic cephalocele is to look for abnormalities of the venous sinus anatomy.
Abnormal orbits
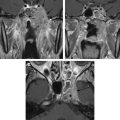
Hypotelorism
Hypotelorism refers to the eyes being abnormally close together, resulting in a decreased interocular diameter (IOD: inner-to-inner margin between orbits) and binocular diameter (BOD: outer-to-outer margin of both orbits). While there are standardized measurements of interocular and binocular diameters, an easy approach to recognizing hypotelorism is that a normal IOD should roughly equal a single orbit width. Findings need to be correlated with ultrasound, which has established standardized measurements. Hypotelorism is rarely seen in isolation and is often associated with midline malformations of the brain, such as holoprosencephaly ( Fig. 8 A, B). Identifying hypotelorism on a fetal MRI should prompt one to scrutinize the intracranial contents for associated brain anomalies. Hypotelorism can also occur with other chromosomal abnormalities, syndromes, and abnormal calvarial development as described previously.