Perineural tumor spread (PNS) is a mode of neoplastic spread whereby tumor cells use neural conduits to escape the borders of a primary tumor. MRI is generally favored over CT for evaluating PNS, and findings include obliteration of fat within skull base foramina, enlargement and enhancement of the involved nerves, and enlargement and destruction of the bony foramina. Careful examination of the entire course of the nerve allows detection of skip lesions. Recognition of the complete extent of PNS is crucial for correct treatment because it facilitates both surgical and radiotherapy targeting of entire extent of disease.
- •
Perineural tumor may extend in a retrograde or antegrade direction and can have skip lesions. Inspection of the entire course of the nerve should be performed.
- •
Perineural tumor spread (PNS) is most common along branches of the trigeminal and facial nerves.
- •
PNS can spread from the facial to the trigeminal nerve and vice versa via the auriculotemporal or greater superficial petrosal nerves.
Patterns of perineural spread in head and neck cancer
Perineural tumor spread (PNS) is a well-recognized entity in head and neck cancers and represents the dissemination of tumor from the primary site via the nerve and neural sheath. It is important to distinguish between perineural invasion and PNS of tumor. Perineural invasion represents small nerve involvement and is a histologic finding at the primary site, present when tumor cells lie within any of the layers of the nerve sheath or when tumor cells surround more than 33% of the circumference of the nerve. Perineural invasion has significant negative prognostic value and correlates with recurrence. Perineural spread, however, describes extension of malignancy beyond the confines of the primary tumor via neural conduits and represents gross, radiologically evident large nerve involvement. It is a mode of metastasis rather than a histologic feature of the primary tumor. PNS most commonly occurs in a retrograde fashion, toward the central nervous system, but also can occur in an antegrade direction. Like perineural invasion, PNS is also considered a poor prognostic factor and suggests aggressive tumor biology.
The common head and neck tumors that spread via the perineural route include cutaneous malignancies, mucosal primaries such as squamous cell carcinoma and salivary gland malignancies (especially adenoid cystic carcinoma), desmoplastic melanoma, nasopharyngeal carcinoma, myeloma, lymphoma, and leukemia. Various theories have been proposed for why PNS occurs; the nerve may represent the line of least resistance through anatomy otherwise difficult to traverse by tumor, or it may be caused by expression of neurotropic growth factors by tumors of the head and neck. Among patients with PNS, 40% are asymptomatic, which puts the onus on the radiologist to be vigilant to its presence. If symptomatic, the patients present with pain, numbness, burning, and dysesthesia along the course of the affected nerve, and motor denervation changes. The latter is most commonly manifested as weakness of the muscles of mastication or facial paralysis. Another common presentation is multiple cranial neuropathies, which indicate involvement of the cavernous sinus and is an ominous sign.
Detection of PNS has important therapeutic implications. Accurate diagnosis of PNS allows complete tumor resection in some cases, and in others allows recognition of unresectable disease before a major ablative surgery is performed. It enables radiation fields to be expanded for complete tumor coverage. PNS also has prognostic significance; in the case of adenoid cystic carcinoma, perineural invasion detected histologically in a larger “named” nerve and skull base involvement predicted much worse rates of local control at 5 years: 12.5% compared with 90% in patients who were named nerve-negative. However, PNS in adenoid cystic carcinoma does not significantly impact long-term survival, which is more dependant on tumor size, TNM staging, histologic subtype, and expression of p53 .
In general, PNS occurs along branches of the facial and trigeminal nerves, although spread along the sixth cranial nerve and the greater auricular nerve has also been described. The greater auricular nerve originates from the cervical plexus and is composed of branches of spinal nerves C2 and C3. It provides sensory supply to the skin over the parotid gland, mastoid process, and outer ear. Additionally, the facial and trigeminal nerves have various interconnections that serve as conduits for widespread dissemination of neoplasm.
Relevant Anatomy
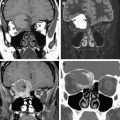
The trigeminal nerve arises from the pons and travels through the prepontine cistern to enter the Meckel cave, a cerebrospinal fluid–filled arachnoidal recess posterolateral to the cavernous sinus ( Fig. 1 ). The trigeminal gasserian ganglion resides along the lateral and anterior wall of the Meckel cave. Within the Meckel cave, the nerve divides into ophthalmic, maxillary, and mandibular divisions ( Fig. 2 ). From the Meckel cave, the ophthalmic and maxillary divisions travel through the lateral wall of the cavernous sinus ( Fig. 3 ). The ophthalmic division (V1), the smallest division of cranial nerve V, divides into the nasociliary, frontal, and lacrimal nerves just before it enters the orbit via the superior orbital fissure. The frontal nerve is the largest branch and divides into the supratrochlear and supraorbital branches, which provide sensory innervation to the skin of the forehead and upper eyelid and the mucosa of the frontal sinus. The nasociliary nerve supplies the nasoethmoid mucosa. The lacrimal nerve provides sensory innervation for the lacrimal gland, conjunctiva, and the lateral upper eyelids. From the cavernous sinus, the maxillary division (V2) enters the pterygopalatine fossa (PPF) via the foramen rotundum ( Fig. 4 ). Within the PPF, V2 gives rise to greater and lesser palatine branches, the zygomatic nerve (sensory to the skin of the temporal region and cheek), and the posterior superior alveolar nerve (supplying the maxillary sinus) before continuing on as the infraorbital nerve in the infraorbital canal ( Fig. 5 ). The infraorbital nerve gives off the anterior and middle superior alveolar nerves to the maxillary teeth and gingiva before emerging from the infraorbital foramen to supply the skin of the midface and lateral nose. The greater and lesser palatine nerves descend from the PPF to the hard palate via the descending palatine canals ( Fig. 6 ).






The mandibular division (V3) exits the skull base via the foramen ovale without entering the cavernous sinus (see Fig. 4 B). It enters the masticator space, giving off branches to the muscles of mastication, the lingual nerve (sensory to tongue), auriculotemporal nerve (sensory to temporal scalp, secretomotor to parotid gland), and buccal nerve (sensory to buccal mucosa and molar teeth), and continues as the inferior alveolar nerve, which enters the mandibular canal and supplies the mandibular teeth and gingiva. At the level of the second premolar, the inferior alveolar nerve gives off the mental nerve, which exits via the mental foramen on the lateral aspect of the mandibular body and supplies the skin of the chin and lower lip. The auriculotemporal nerve anatomy is described in greater detail in subsequent paragraphs. Tumor anywhere within the dermatomal distribution of the trigeminal nerve can perineurally spread via the pathways mentioned earlier through the skull base foramina into the cranial cavity.
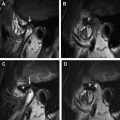
The facial nerve arises from the pons, and its fibers loop around the abducens nucleus to form the facial colliculus in the anterior wall of the fourth ventricle. It crosses the cerebellopontine angle cistern (cisternal segment) and enters the internal auditory canal, where it resides in the superior anterior compartment (canalicular segment). The labyrinthine segment lies between the canalicular segment and the first genu and is so named because of its intimate relationship to the inner ear (labyrinth) ( Fig. 7 A). The tympanic segment travels posterolaterally from the first genu under the lateral semicircular canal (best appreciated on coronal images) (see Fig. 7 B). From the second genu, close to the pyramidal process, the nerve travels straight down in the mastoid bone (mastoid segment) and exits the skull via the stylomastoid foramen to enter the parotid gland. The facial nerve has five branches in the parotid gland: temporal, zygomatic, buccal, marginal mandibular, and cervical. Presence of a perineural venous plexus can cause normal enhancement beyond the first genu of the nerve. If the enhancement is thick and asymmetric, even in the parts of the nerve that can normally enhance, one should suspect pathology in the appropriate clinical setting. Any enhancement of the nerve proximal to the first genu is very suspicious.

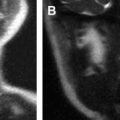
Connections exist between the facial and trigeminal nerve that facilitate tumor traveling between these nerves. The greater superficial petrosal nerve is a branch of the facial nerve that provides parasympathetic innervation to the lacrimal gland, palate, nasal cavity, and nasopharynx. It contains facial nerve fibers originating in the nervus intermedius, exits the geniculate ganglion at the facial hiatus, passes close to the Meckel cave, and joins with the deep petrosal nerve to form the vidian nerve, which passes through the vidian canal to the pterygopalatine fossa where its preganglionic fibers synapse in the pterygopalatine ganglion. Some of the postganglionic fibers join branches of V2 in the PPF ( Fig. 8 ). PNS along the greater superficial petrosal nerve (GSPN) usually occurs after the tumor has reached the PPF, from where retrograde extension via the vidian nerve to GSPN can occur ( Fig. 9 ). Also, tumor in the Meckel cave may extend directly to the GSPN because of their proximity.