SONOGRAPHIC ABBREVIATIONS
Ao Aorta
Bl Bladder
Bwl Bowel
GB Gallbladder
HEM Hematoma
Ip Iliopsoas muscle
IVC Inferior vena cava
K Kidney
L Liver
LHA Left hepatic artery
LHV Left hepatic vein
LPV Left portal vein
MPV Main portal vein
MHV Middle hepatic vein
P Pancreas
PHA Proper hepatic artery
RAt Right atrium
RHA Right hepatic artery
RHV Right hepatic vein
RPV Right portal vein
RK Right kidney
Sp Spine
Spl Spleen
St Stomach
Ut Uterus
KEY WORDS
Abscess. Localized collection of pus caused by pyogenic bacterium.
AIDS. Acquired immunodeficiency syndrome. An immune system disorder caused by the human immunodeficiency virus (HIV) resulting in increased susceptibility to opportunistic infections throughout the body.
Anemia. Too few red blood cells. Causes include decreased blood cell formation, blood cell destruction, and bleeding.
Candidiasis. A fungal infection with the Candida organism (Candida albicans is the most common type) that affects the skin, mucous membranes, lungs, and blood system. Occurs in patients who are immune-compromised or patients who have taken multiple antibiotics.
Cholangitis. Infection of the biliary tree.
Cholecystitis. Infection of the gallbladder.
Cystitis. Inflammation of the bladder commonly associated with urinary tract infections (UTIs).
Cytomegalovirus (CMV). A form of the herpes virus that can become pathogenic with immune-compromised patients including those with AIDS, organ transplants, extensive burns, and underdeveloped immune systems.
Erythrocyte Sedimentation Rate (ESR). This laboratory test determines how far red blood cells settle to the bottom of a specially marked test tube within 1 hour. ESR can be used to screen for a variety of pathogens.
Fever. See Pyrexia.
Gallbladder Fossa. The area located on the inferior aspect of the liver where the gallbladder is situated.
Gossypiboma. A sterile collection of fluid surrounding a sterile surgical sponge inadvertently left in the body postoperatively.
Gutters. See Paracolic Gutters.
Hematocrit. The percentage of erythrocytes in a given volume of blood after centrifugation.
Hematoma. A clot or collection of blood confined to an organ or space within the body.
Hemolysis. Breakdown of red blood cells with release of hemoglobin into the surrounding plasma.
Hemorrhage. An internal or external discharge of blood resulting from damage to the vascular system at the arterial, venous, or capillary levels.
Hypernephroma. Older term for renal cell carcinoma.
Immunosuppressed. A term used to describe the circumstance in which the immune system is not operating on a normal level. Affected patients include those who are being treated with drugs or suffering from an illness that decreases the body’s response to infection. Examples of causes include AIDS, steroids, and anticancer drugs.
Leukocyte. A white blood cell (WBC) that acts as a phagocyte to defend the body against infection and aids in the repair of damaged tissues.
Leukocytosis. An increase in the number of leukocytes (WBC).
Lymphadenopathy. Abnormally enlarged lymph nodes that are an indication that a disease process is present within the lymph system.
Murphy’s Sign (sonographic). Localized tenderness over the gallbladder.
Paracolic Gutters. Areas in the flanks lateral to the colon where ascites and abscesses can form.
Pneumocystis Carinii Pneumonia (PCP). An otherwise rare type of bacterial pneumonia commonly seen in patients infected with the AIDS virus.
Prostatitis. Inflammation or infection of the prostate gland.
Pyelonephritis. Infection of the kidney(s).
Pyogenic. The production of pus caused by a microorganism infecting an organ or body system.
Pyrexia. A rise in body temperature above 98.6°F (37°C).
Sedimentation Rate. See Erythrocyte Sedimentation Rate (ESR).
Sepsis. The presence of pathogenic microorganisms or their toxic products that spread from the originally affected organ into the blood circulatory system.
Septicemia. Infection in the blood.
Staging. Demonstration of the areas that are involved in a malignancy. The more areas that are involved, the more severe the staging grade will be.
Subphrenic. Under the diaphragm.
Subpulmonic. The area located inferior to the lung and superior to the diaphragm.
RELEVANT LABORATORY VALUES
Cultures (aerobic and anaerobic): No range applicable, test indicates type of pathogen
Purified protein derivative (PPD): No range applicable, test is positive or negative. Positive indicates the patient has had exposure to tuberculosis.
Erythrocyte sedimentation rate (ESR): Elevated values are associated with a wide range of infectious and inflammatory diseases.
Men 18 to 50 years 0 to 15 mm/hr
Men ≥50 years 0 to 20 mm/hr
Women 18 to 50 years 0 to 20 mm/hr
Women ≥50 years 0 to 30 mm/hr
Urinalysis: Abnormal values may be associated with kidney or bladder infections.
Specific gravity 1.005 to 1.030
pH 5.0 to 7.5
Urobilinogen 0.1 to 1.0 mg/dL
WBC 0 to 5/hpf; RBC 0 to 2/hpf
Epithelial cells (only squamous) 0 to 2/hpf
Casts 0 to 1 hyaline cast/lpf
WBC: High values are associated with infection.
1 month to 2 years—6.0 to 14.0 K/uL
2 to 10 years—4.0 to 12.0 K/uL
10 to 18 years—4.0 to 10.5 K/uL
> 18 years 3.8 to 10.5 K/uL
The Clinical Problem
Pyrexia, or fever, is defined as an elevation of body temperature above 98.6°F (37°C) oral temperature and is a common symptom associated with numerous types of pathological etiologies. The cause of the fever can usually be narrowed by examining the patient’s history, symptoms, and laboratory results; however, in some cases, this information does not provide sufficient data to explain the fever. If the patient’s condition continues over several weeks, it is classified as a fever of unknown origin (FUO). Before beginning a study in a patient with FUO, the history and laboratory data in the patient’s chart should be checked for evidence suggesting any of the possibilities mentioned (information to follow; see also Key Words). Understanding the patient’s history will help the sonographer concentrate on the most appropriate areas.
The differential diagnosis for patients with FUO relies on a classification based on their clinical history and laboratory results. There are four broad categories of disease that are common in most patients with FUO, including infections, malignancies, autoimmune conditions, and miscellaneous symptoms. Factors affecting the diagnosis include the patient’s individual symptoms, the duration of the symptoms, the patient’s age, and underlying pathologies.
In cases of FUO, radiographs (x-ray “plain” films) and computed tomography (CT) with oral and/or intravenous contrast are usually the first medical imaging tests ordered to detect the underlining cause of the fever. Ultrasound examinations are routinely ordered as follow-up studies to provide additional information on the gallbladder and biliary tract and to better evaluate abdominal and pelvic abscesses that are identified on x-ray and CT. In cases when venous thrombosis is suspected as a potential cause of the fever, lower and/or upper extremity peripheral Doppler examinations may also be ordered. When tumors, abscesses, and ascites are identified, ultrasound-guided invasive procedures (such as paracentesis and biopsy) can be performed to obtain samples that can be analyzed to identify the exact pathogen causing the fever; this type of examination allows appropriate antibiotic therapy to be started.
ABSCESSES
Patients who have recently undergone invasive or surgical procedures are susceptible to abscesses (wound infection) that can spread throughout the chest, abdomen, and pelvis. Symptoms associated with abscess include fever, localized pain, and an elevated WBC count. Infections usually start approximately on the fifth postoperative day and develop into an abscess approximately on the 10th postoperative day. Risk factors include cancer, diabetes, connective tissue disorders, immunosuppression, and existing hematomas.
ORGAN INFLAMMATION
Infection may progress to actual abscess formation or may be limited to organ inflammation. The following conditions may induce fever, yet there may be no localizing clinical signs. Sonographic findings may be present.
1. Hepatitis
2. Pyelonephritis
3. Cholecystitis
4. Cholangitis
5. Pancreatitis
6. Cystitis
7. Prostatitis
Many tumors are associated with fever and leukocytosis and may mimic the characteristics of infections. Common malignant causes include renal cell carcinoma, lymphoma, and hepatoma (Fig. 11-1).
POSTOPERATIVE COLLECTIONS
Patients who have recently undergone surgery may develop a fluid pocket at the incision site. Cesarean section, hysterectomy, liver surgery, and organ transplantation are often followed by collection development that may be a hematoma, urinoma, abscess, lymphocele, biloma, ascites, or seroma. Hematomas also follow anticoagulant therapy. They may be suspected when a drop in the patient’s hematocrit level is present. Any of these fluid collections may become superinfected.
GOSSYPIBOMA
This sterile collection due to a retained surgical sponge has a distinctive appearance on ultrasound (Fig. 11-2).
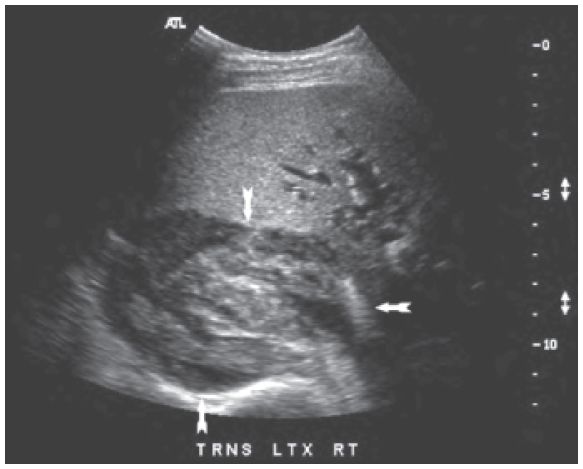
Figure 11-1. ![]() A. Transverse diagram of the female pelvis with a left-sided tubo-ovarian abscess. The abscess contains air, which rises to the top and casts a strong acoustic shadow. Retained sponge (gossypiboma) would be another cause of the same sonographic appearance. B. CT of gossypiboma located in front of the right kidney. Gas bubbles trapped within the cotton surgical sponge will have an echogenic shadowing appearance on ultrasound.
A. Transverse diagram of the female pelvis with a left-sided tubo-ovarian abscess. The abscess contains air, which rises to the top and casts a strong acoustic shadow. Retained sponge (gossypiboma) would be another cause of the same sonographic appearance. B. CT of gossypiboma located in front of the right kidney. Gas bubbles trapped within the cotton surgical sponge will have an echogenic shadowing appearance on ultrasound.
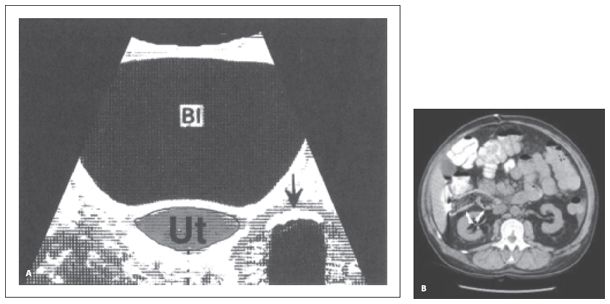
Figure 11-2. ![]() A. Transverse diagram of the female pelvis with a left-sided tubo-ovarian abscess. The abscess contains air, which rises to the top and casts a strong acoustic shadow. Retained sponge (gossypiboma) would be another cause of the same sonographic appearance. B. CT of gossypiboma located in front of the right kidney. Gas bubbles trapped within the cotton surgical sponge will have an echogenic shadowing appearance on ultrasound.
A. Transverse diagram of the female pelvis with a left-sided tubo-ovarian abscess. The abscess contains air, which rises to the top and casts a strong acoustic shadow. Retained sponge (gossypiboma) would be another cause of the same sonographic appearance. B. CT of gossypiboma located in front of the right kidney. Gas bubbles trapped within the cotton surgical sponge will have an echogenic shadowing appearance on ultrasound.
AIDS is a disease transmitted through bodily fluids such as blood and semen. It has many sonographic manifestations and is due to an infection with a virus known as human immunodeficiency virus (HIV). A patient with AIDS does not pose a risk of infection to a sonographer unless blood from the infected individual contacts a bleeding surface or mucous membrane on the sonographer. Infections are alleged to have taken place through the conjunctiva of the eye and the mucous membrane of the mouth from blood that splashed from the patient at the time of surgery or biopsy. It is therefore essential to wear a mask and an eye guard if a puncture procedure is being performed on an AIDS patient. Otherwise, contact with AIDS patients is not dangerous and routine universal precautions are adequate.
AIDS almost exclusively affects members of four groups: (1) homosexuals; (2) intravenous drug abusers; (3) hemophiliacs and those who have had multiple blood transfusions; and (4) individuals who have intercourse with an HIV-infected person (this last mode is becoming increasingly common). AIDS is widespread in Haiti and east Africa.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


