Abstract
Fine reticular opacities are reliable evidence of interstitial lung disease that requires consideration of a variety of acute and chronic diseases. Acute interstitial disease is most often the result of interstitial edema or pneumonia. Both may spread through the bronchovascular and septal interstitium. Involvement of the interlobular septa in the periphery of the lung are described as Kerley B lines. Kerley B lines are a common finding in patients with interstitial edema, but when they are more chronic they are a clue to suspect lymphangitic spread of a tumor. The collagen vascular and idiopathic interstitial lung diseases cause interstitial scarring that is more disorganized and does not spare the normal interstitial septa. Fine reticular opacities may be evidence of an early stage of these diseases.
Keywords
asbestosis, idiopathic pulmonary fibrosis, interlobular septal lines, interstitial edema, interstitial pneumonia, Kerley A and B lines, lymphangitic carcinoma, lymphoma, rheumatoid disease, sarcoidosis, scleroderma
Questions
- 1.
Kerley B lines ( Fig. 18.1 ) represent which one of the following?
- a.
Thick interlobular septa.
- b.
Dilated lymphatic vessels.
- c.
Dilated venules.
- d.
Thick alveolar walls.
- e.
Fibrosis.
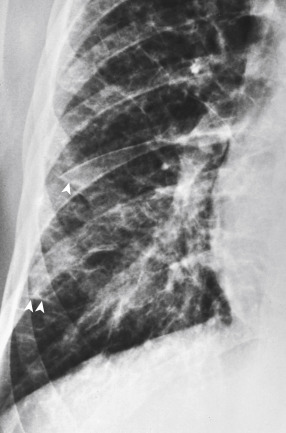
Fig. 18.1
- a.
- 2.
Which one of the following statements is not true?
- a.
Kerley B lines are perpendicular to the pleura.
- b.
Kerley A lines are deep in the lung parenchyma.
- c.
Kerley lines are diagnostic of pulmonary edema.
- d.
Kerley lines indicate interstitial disease.
- e.
Dilated lymphatics are one cause of Kerley lines.
- a.
- 3.
Which one of the following diagnoses is most likely in the case illustrated in Fig. 18.2 ?
- a.
Pulmonary edema.
- b.
Lymphangitic carcinomatosis.
- c.
Lymphoma.
- d.
Sarcoidosis.
- e.
Idiopathic pulmonary fibrosis.
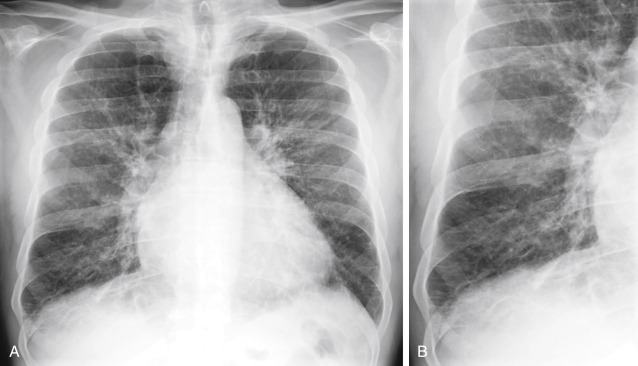
Fig. 18.2
- a.
- 4.
Which one of the following causes of fine reticular opacities is least likely to be associated with pleural effusion?
- a.
Lymphangitic carcinomatosis.
- b.
Lymphoma.
- c.
Scleroderma.
- d.
Rheumatoid disease.
- e.
Pulmonary edema.
- a.
Discussion
The diffuse, fine reticular pattern (see Fig. 18.1 ) is one of the most reliable patterns for identifying diffuse interstitial disease. Because this pattern is linear, the lines must be distinguished from the normal pattern of blood vessels. In the early stages of an interstitial disease, this may be impossible by chest radiography, and high-resolution computed tomography (HRCT) may be required to confirm minimal interstitial disease. Interstitial diseases may spread throughout the bronchovascular or the septal interstitium while fibrotic diseases destroy the normal lung tissues, but both processes cause fine reticular opacities.
Kerley lines are the most reliable radiologic observation for making the distinction of bronchovascular versus septal interstitial disease. 150 , 175 , 235 Kerley B lines are short lines that are perpendicular to the pleura and continuous with it. The latter feature distinguishes the Kerley B lines from small vessels. Kerley B lines are usually observed in the costophrenic angles on the posteroanterior view and, occasionally, on the lateral view in the retrosternal clear space. They were first thought to represent only enlarged lymphatics but, based on pathologic correlations, these lines represent more generalized, enlarged interlobular septa. (Answer to question 1 is a .) Although it is true that the engorgement of septal lymphatic vessels would contribute to Kerley B lines, this has probably been overemphasized. In lymphangitic carcinomatosis, metastatic tumor spreads through dilated lymphatics in the interlobular septa and causes fine reticular opacities. In the other entities listed in Chart 18.1 , dilation of lymphatics is not a sufficient explanation for the presence of Kerley B lines. Furthermore, in congestive heart failure, edema of the loose connective tissue of the interlobular septa accounts for Kerley lines, rather than engorged lymphatics.
- I.
Acute
- A.
Edema
- B.
Infection
- 1.
Viral pneumonia 235 , 475 , 547
- 2.
Mycoplasma pneumonia 170
- 3.
Infectious mononucleosis
- 4.
Malaria 68 ( Plasmodium falciparum )
- 5.
Pneumocystis jiroveci pneumonia
- 1.
- A.
- II.
Chronic
- A.
Chronic edema
- 1.
Atherosclerotic heart disease
- 2.
Mitral stenosis 75
- 3.
Left atrial tumor (myxoma)
- 4.
Pulmonary veno-occlusive disease 529
- 5.
Sclerosing mediastinitis
- 1.
- B.
Granulomatous disease
- C.
Collagen vascular disease 241 , 497 , 541
- 1.
Rheumatoid lung 576
- 2.
Scleroderma lung 19
- 3.
Dermatomyositis and polymyositis 259
- 4.
Sjögren syndrome 307
- 1.
- D.
Lymphangitic carcinomatosis 235 , 258 , 269 , 279
- E.
Lymphocytic disorders
- F.
Environmental disease 182 , 299 , 429
- C.
Drug reactions (see Chart 18.1 ) 18 , 52 , 434 , 489 , 562
- D.
Idiopathic
- 1.
Idiopathic pulmonary fibrosis 104 , 364 , 398 , 440 , 553 , 569
- 2.
Desquamative interstitial pneumonia 355
- 3.
Tuberous sclerosis 24
- 4.
Lymphangioleiomyomatosis 24 , 401 , 510
- 5.
Idiopathic pulmonary hemosiderosis
- 6.
Amyloidosis 246
- 7.
Interstitial calcification (chronic renal failure) 158
- 8.
Alveolar proteinosis (late complication)
- 9.
Gaucher disease 645
- 10.
- 1.
- A.
Kerley A lines are also important and reliable signs of interstitial disease. These lines are linear opacities that appear to cross the normal vascular markings. Heitzman 235 showed that they correspond anatomically to thick interlobular septa. They differ from Kerley B lines only by their location, representing thick interlobular septa that are deep in the lung parenchyma. Kerley A lines may be suspected from the chest radiograph and account for the fine reticular interstitial pattern, but HRCT is often required to confirm the pattern by showing thickened interlobular septa, which outline the secondary pulmonary lobules. 221 , 614 , 617 (Answer to question 2 is c ; pulmonary edema is only one cause of Kerley lines.)
Fibrosis of the interstitium may involve the septal and bronchovascular interstitium but revises and destroys the normal lung architecture as it progresses. The radiologic result is a pattern of irregular fine linear and curvilinear opacities that appear more disorganized. Thickened interlobular septa are not an expected result of fibrosis.
Pulmonary Edema
Pulmonary interstitial edema is the most common cause of fine reticular opacities. (Answer to question 3 is a ). Edema first spreads through the bronchovascular interstitium and later through the septal interstitium, but Kerley B lines are an infrequent observation in patients with congestive heart failure. Kerley lines are most often seen in patients with chronic or recurrent heart failure. The next step in the evaluation of this pattern is to check for other signs that might suggest congestive heart failure. These include an enlarged heart with left ventricular or left atrial enlargement, prominence of upper lobe vessels, constriction of lower lobe vessels (cephalization of flow), peribronchial cuffing, increased width of the vascular pedicle, and signs of pleural effusion, including thickening of the interlobar fissures 75 , 390 ( Figs 18.2 and 18.3 ). Prominence of the left atrium without left ventricular enlargement, in combination with fine reticular opacities and prominence of upper lobe vessels, strongly suggests mitral valve disease. 659 A clinical history of rheumatic fever and a murmur indicating mitral stenosis should be sufficient to confirm the diagnosis. Cardiac ultrasound examination is a reliable noninvasive method for confirming such a diagnosis and for excluding the rare atrial myxoma, which may also produce the classic chest radiographic findings of mitral stenosis.