First Trimester Pregnancy
Ralph C. Wang
R. Starr Knight
INTRODUCTION
Sonography of first trimester pregnancy is a core bedside ultrasound application, and an essential component of the evaluation of patients who present with vaginal bleeding, abdominal pain, syncope or shock in early pregnancy (1). In most cases, bedside ultrasound allows emergency physicians to rapidly and accurately determine whether an intrauterine pregnancy (IUP) is present. Along with other clinical data, ultrasound findings allow emergency physicians to arrive at an accurate diagnosis and appropriate disposition, thus providing efficient care that benefits both patients and emergency department (ED) flow.
CLINICAL APPLICATIONS
The role of emergency physicians is to rule out life threats, and as such, the primary role of bedside pelvic ultrasound in the ED is to exclude ectopic pregnancy (1). Secondary aims include the following:
Detecting abnormal pregnancies, including ectopic pregnancy and nonviable pregnancy
Detecting hemoperitoneum in patients with suspected ectopic pregnancy
Determining gestational age
Detecting fetal heart rate to determine viability
Ectopic pregnancy, a common and potentially fatal condition, should be considered in all symptomatic first trimester patients who present to the ED. History and physical examination are often insufficient to reliably establish the definitive diagnosis of normal (or abnormal) pregnancy (2). Ultrasound is widely used as the most efficient and accurate means to detect and evaluate early gestations. Emergency physicians who are trained to perform and interpret bedside pelvic ultrasound should first answer the focused question: “Is there an IUP?” Ectopic pregnancy can be safely excluded in patients in whom an IUP is visualized, with the notable exception of patients who have received fertility treatments, who are at increased risk for multiple gestations and heterotopic pregnancy (3,4).
Secondary roles for pelvic bedside ultrasound include identification of abnormal pregnancies (including ectopic pregnancy and fetal demise), and detection of hemoperitoneum in ruptured ectopic pregnancy. When an IUP is not visualized, emergency physicians trained in bedside ultrasound may be able to detect specific sonographic findings consistent with ectopic pregnancy (5). Although early recognition of pregnancy loss is often not medically necessary, it remains important to advise a woman of an accurate gestational age, and when possible, to reassure her of the health of the pregnancy at the time of evaluation or to prepare her for the possibility that the pregnancy will not survive. In addition, the timeliness of appropriate follow-up care is made clearer when a viable or a nonviable IUP is detected by bedside ultrasound.
IMAGE ACQUISITION
Pelvic ultrasound image acquisition for patients in the first trimester is similar to the nonpregnant patient. For a full, detailed description of the technique, please refer to Chapter 14, Figures 14.1, 14.2, 14.3, 14.4, 14.5 and 14.6. Briefly, the transabdominal view should be performed with the patient in the supine position and with a full bladder. A low-frequency probe is placed in the sagittal plane above the symphysis pubis. Using the bladder as a sonographic window, the pelvic structures—uterus, cervix, and adnexa—are visualized. The probe is then rotated 90 degrees for the transverse plane. It is important to fan up and down through the pelvis from the uterine fundus to the cervix in the transverse plane, and from side-to-side in the longitudinal plane. The transvaginal view should be performed with the patient in a pelvic bed in the lithotomy position (or with a cushion placed under the buttocks) with an empty bladder. A high-frequency endocavitary probe is placed in the vagina in the sagittal plane just past the bladder to obtain a view of the uterus in long axis. When the uterus is visualized clearly, fan through the uterus from side to side (adnexa to adnexa). Rotate the probe counterclockwise into the coronal plane. The probe should be swept, this time from top to bottom, to image the uterus from fundus to cervix. Special attention should be paid to intrauterine contents, as well as free fluid and the adnexa. In order to optimize image acquisition for first trimester pelvic scanning, select the software setting for OB to access software applications to calculate fetal heart rate and gestational age.
NORMAL ULTRASOUND ANATOMY
The specific sonographic appearance of normal pregnancy depends upon the gestational age. As the gestational age increases, the ability to assess the location and health of the pregnancy improves. Gestational age is linked to the appearance of important findings of IUP, as shown in Table 15.1.
Findings Suggestive of an Early IUP: The Gestational Sac
The appearance of a gestational sac is the earliest sign of an IUP; it is suggestive of, but not definitive for an IUP. The earliest evidence of a gestational sac is seen at 4.5 weeks and appears as a small 2 to 3 mm cystic structure embedded in thickened endometrium (decidua); this appearance has been described as the intradecidual sign (6,7). A distinguishing characteristic of the intradecidual sign is that the thin endometrial stripe passes to one side of the gestational sac, unlike a cyst or intracavitary fluid collection. The intradecidual sign is specific but insensitive for the diagnosis of IUP (7,8). Because this is a subtle finding that is technically difficult to recognize or distinguish from decidual cysts, emergency physicians should depend on finding more definitive evidence of an IUP.
TABLE 15.1 Sonographic Landmarks of Normal Pregnancy | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
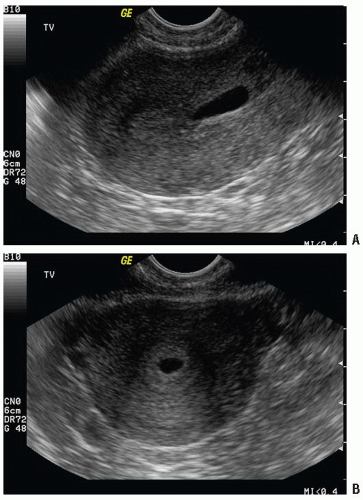
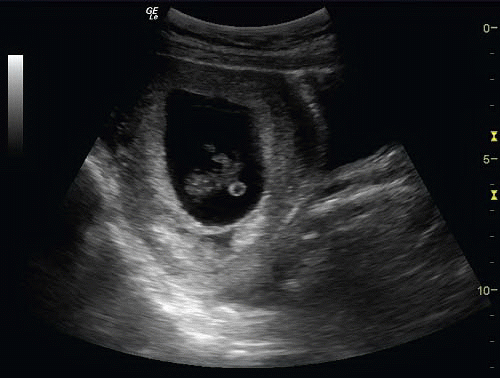
The gestational sac is an anechoic fluid-filled collection surrounded by a thickened decidua within the uterus that represents an early IUP (Figs. 15.1 and 15.2; eFigs. 15.1-15.4;
 VIDEOS 15.1 and 15.2). Unfortunately, what appears to be a gestational sac may in fact be a pseudogestational sac, an intrauterine fluid collection visualized in association with ectopic pregnancy due to hormonal stimulation of the endometrium (Fig. 15.3) (9). Differentiating between a true gestational sac and a pseudogestational sac requires care and experience, and the presence of an intrauterine fluid collection alone should not be considered definitive evidence of IUP (10). Studies in the radiology literature have suggested that the presence of a double decidual sign may aid in the differentiation of gestational sac from pseudogestational sac (11). The double decidual sign is created by the separation of the decidua vera from the decidual capsularis, creating a double echogenic ring around early IUPs (Fig. 15.1B; eFig. 15.5;
VIDEOS 15.1 and 15.2). Unfortunately, what appears to be a gestational sac may in fact be a pseudogestational sac, an intrauterine fluid collection visualized in association with ectopic pregnancy due to hormonal stimulation of the endometrium (Fig. 15.3) (9). Differentiating between a true gestational sac and a pseudogestational sac requires care and experience, and the presence of an intrauterine fluid collection alone should not be considered definitive evidence of IUP (10). Studies in the radiology literature have suggested that the presence of a double decidual sign may aid in the differentiation of gestational sac from pseudogestational sac (11). The double decidual sign is created by the separation of the decidua vera from the decidual capsularis, creating a double echogenic ring around early IUPs (Fig. 15.1B; eFig. 15.5;  VIDEOS 15.3 and 15.4). Although this is considered a useful sign, it is present in the minority of IUPs (12). Gestational sacs are characterized by several sonographic criteria, including size, shape, location within the uterus, and appearance of the border (13,14). Normal gestational sacs are smooth, well defined, rounded or oval, have an echogenic border of decidua that is 2 mm or greater, and are situated in the upper uterine body. Sacs that are low lying (near the cervix), irregularly shaped, or surrounded by thin decidua are suspicious for abnormal pregnancies.
VIDEOS 15.3 and 15.4). Although this is considered a useful sign, it is present in the minority of IUPs (12). Gestational sacs are characterized by several sonographic criteria, including size, shape, location within the uterus, and appearance of the border (13,14). Normal gestational sacs are smooth, well defined, rounded or oval, have an echogenic border of decidua that is 2 mm or greater, and are situated in the upper uterine body. Sacs that are low lying (near the cervix), irregularly shaped, or surrounded by thin decidua are suspicious for abnormal pregnancies.
 VIDEOS 15.1 and 15.2). Unfortunately, what appears to be a gestational sac may in fact be a pseudogestational sac, an intrauterine fluid collection visualized in association with ectopic pregnancy due to hormonal stimulation of the endometrium (Fig. 15.3) (9). Differentiating between a true gestational sac and a pseudogestational sac requires care and experience, and the presence of an intrauterine fluid collection alone should not be considered definitive evidence of IUP (10). Studies in the radiology literature have suggested that the presence of a double decidual sign may aid in the differentiation of gestational sac from pseudogestational sac (11). The double decidual sign is created by the separation of the decidua vera from the decidual capsularis, creating a double echogenic ring around early IUPs (Fig. 15.1B; eFig. 15.5;
VIDEOS 15.1 and 15.2). Unfortunately, what appears to be a gestational sac may in fact be a pseudogestational sac, an intrauterine fluid collection visualized in association with ectopic pregnancy due to hormonal stimulation of the endometrium (Fig. 15.3) (9). Differentiating between a true gestational sac and a pseudogestational sac requires care and experience, and the presence of an intrauterine fluid collection alone should not be considered definitive evidence of IUP (10). Studies in the radiology literature have suggested that the presence of a double decidual sign may aid in the differentiation of gestational sac from pseudogestational sac (11). The double decidual sign is created by the separation of the decidua vera from the decidual capsularis, creating a double echogenic ring around early IUPs (Fig. 15.1B; eFig. 15.5;  VIDEOS 15.3 and 15.4). Although this is considered a useful sign, it is present in the minority of IUPs (12). Gestational sacs are characterized by several sonographic criteria, including size, shape, location within the uterus, and appearance of the border (13,14). Normal gestational sacs are smooth, well defined, rounded or oval, have an echogenic border of decidua that is 2 mm or greater, and are situated in the upper uterine body. Sacs that are low lying (near the cervix), irregularly shaped, or surrounded by thin decidua are suspicious for abnormal pregnancies.
VIDEOS 15.3 and 15.4). Although this is considered a useful sign, it is present in the minority of IUPs (12). Gestational sacs are characterized by several sonographic criteria, including size, shape, location within the uterus, and appearance of the border (13,14). Normal gestational sacs are smooth, well defined, rounded or oval, have an echogenic border of decidua that is 2 mm or greater, and are situated in the upper uterine body. Sacs that are low lying (near the cervix), irregularly shaped, or surrounded by thin decidua are suspicious for abnormal pregnancies.Although emergency physicians are cautioned not to rely on the presence of an intradecidual sign, a double decidual sign, or gestational sac to establish a definitive diagnosis of IUP, it is also important to recognize that the absence of these findings does not exclude the possibility of an IUP (12).
Definitive Findings of IUP
Yolk sac
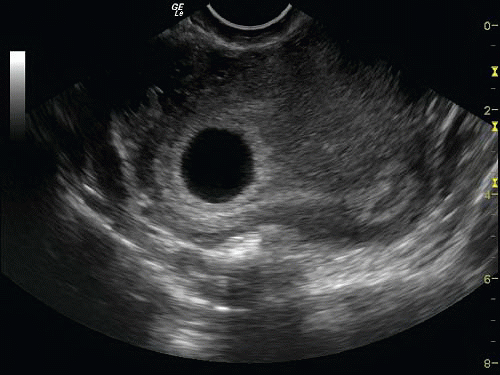
The visualization of a yolk sac is the first definitive sign of an IUP (15). The yolk sac has the appearance of a brightly echogenic ring within the gestational sac (Fig. 15.4; eFigs. 15.6-15.8;  VIDEOS 15.4 and 15.5) (16). Using current transvaginal ultrasound technology, the yolk sac can be seen at a gestational age of approximately 5 weeks (3). The yolk sac may be small (3 mm) and challenging to demonstrate (Fig. 15.5;
VIDEOS 15.4 and 15.5) (16). Using current transvaginal ultrasound technology, the yolk sac can be seen at a gestational age of approximately 5 weeks (3). The yolk sac may be small (3 mm) and challenging to demonstrate (Fig. 15.5;  VIDEO 15.6). The upper size limit of a normal yolk sac is 5 to 6 mm in diameter. In a normal IUP, it is generally accepted that the yolk sac should be observed when a gestational sac measures >8 mm by the transvaginal approach and >20 mm by transabdominal approach (16).
VIDEO 15.6). The upper size limit of a normal yolk sac is 5 to 6 mm in diameter. In a normal IUP, it is generally accepted that the yolk sac should be observed when a gestational sac measures >8 mm by the transvaginal approach and >20 mm by transabdominal approach (16).
 VIDEOS 15.4 and 15.5) (16). Using current transvaginal ultrasound technology, the yolk sac can be seen at a gestational age of approximately 5 weeks (3). The yolk sac may be small (3 mm) and challenging to demonstrate (Fig. 15.5;
VIDEOS 15.4 and 15.5) (16). Using current transvaginal ultrasound technology, the yolk sac can be seen at a gestational age of approximately 5 weeks (3). The yolk sac may be small (3 mm) and challenging to demonstrate (Fig. 15.5;  VIDEO 15.6). The upper size limit of a normal yolk sac is 5 to 6 mm in diameter. In a normal IUP, it is generally accepted that the yolk sac should be observed when a gestational sac measures >8 mm by the transvaginal approach and >20 mm by transabdominal approach (16).
VIDEO 15.6). The upper size limit of a normal yolk sac is 5 to 6 mm in diameter. In a normal IUP, it is generally accepted that the yolk sac should be observed when a gestational sac measures >8 mm by the transvaginal approach and >20 mm by transabdominal approach (16).Fetal pole
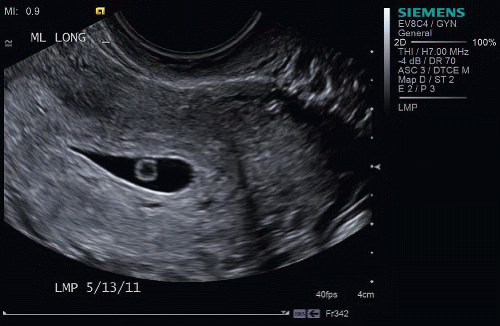
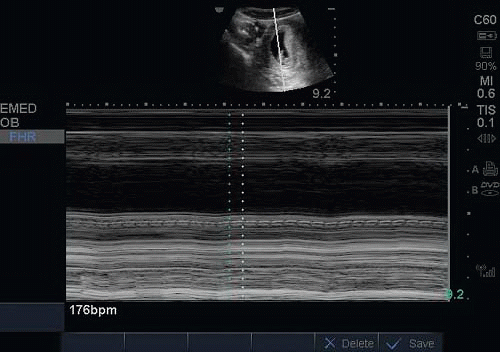
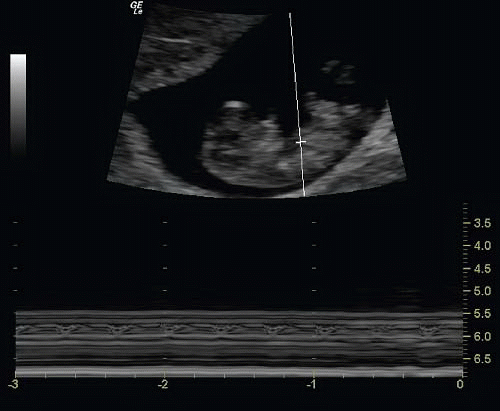
The fetal pole is also a reliable sign of IUP. A fetal pole should be visualized by the time the gestational sac reaches 18 mm by transvaginal approach and 25 mm by the transabdominal approach (Figs. 15.6, 15.7 and 15.8; eFigs. 15.9 and 15.10;  VIDEO 15.5). After the fetal pole has reached 5 mm, a cardiac flicker can be visualized by transvaginal ultrasound and fetal heart rate measured using M-mode (
VIDEO 15.5). After the fetal pole has reached 5 mm, a cardiac flicker can be visualized by transvaginal ultrasound and fetal heart rate measured using M-mode ( VIDEOS 15.7-15.9) (17).
VIDEOS 15.7-15.9) (17).
 VIDEO 15.5). After the fetal pole has reached 5 mm, a cardiac flicker can be visualized by transvaginal ultrasound and fetal heart rate measured using M-mode (
VIDEO 15.5). After the fetal pole has reached 5 mm, a cardiac flicker can be visualized by transvaginal ultrasound and fetal heart rate measured using M-mode ( VIDEOS 15.7-15.9) (17).
VIDEOS 15.7-15.9) (17).Determining Fetal Viability: Fetal Heart Activity
M-mode (motion mode) sonography is useful in measuring fetal heart rate in the first trimester. M-mode detects the motion of reflectors in an ultrasound image with respect to a cursor displayed over time. Fetal heart rate can be documented in M-mode using the built-in fetal heart rate calculators of most current equipment (Figs. 15.9 and 15.10; eFig. 15.11). Several radiology studies have demonstrated the predictive value of fetal heart activity on pregnancy outcome. From 5 to 9 weeks of gestation, the mean heart rate ranges from 110 to 175 beats per minutes. Fetal heart rate increases with increasing size, and abnormally low fetal heart rates are associated
with embryonic demise (18). Several studies have shown a high rate of miscarriage in first trimester patients with fetal heart rates <85 beats per minute (19).
with embryonic demise (18). Several studies have shown a high rate of miscarriage in first trimester patients with fetal heart rates <85 beats per minute (19).
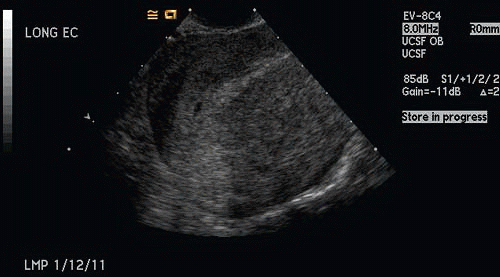
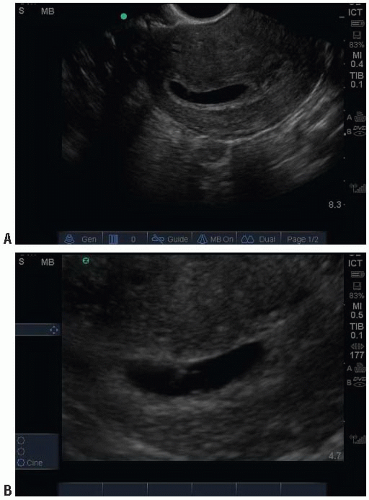 FIGURE 15.5. Transvaginal Ultrasound of an IUP in a Coronal Plane. The yolk sac can be difficult to visualize (A). In the same patient the yolk sac can be better visualized with the zoom feature (B). |
Determining Gestational Age
The gestational age in early pregnancy can be accurately determined based on sonographic measurements at different stages of pregnancy. Standard measurements of gestational age are referenced from the onset of the last normal menstrual period, but may be inaccurate. Underserved populations with poor access to obstetric care may also require ED determination of gestational age. Recent studies have shown that emergency physicians can accurately estimate gestational age using bedside pelvic ultrasound (20,21).
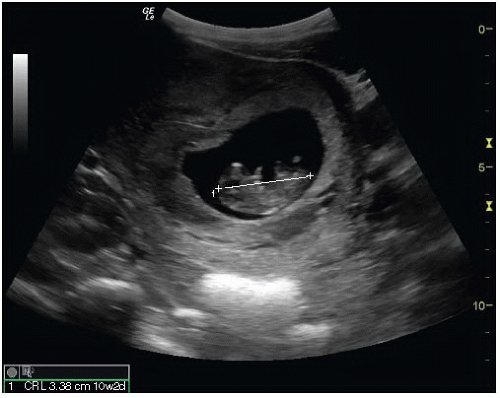
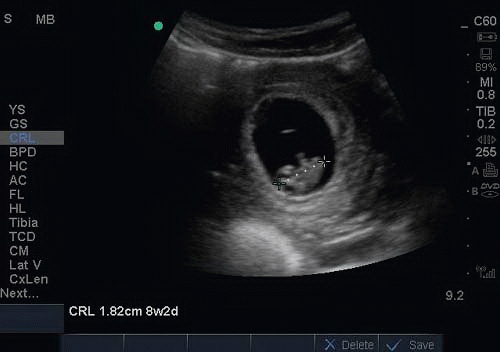 FIGURE 15.7. First Trimester Fetus, 8 Weeks 2 Days Gestation as Measured by Crown-Rump Length (CRL). |
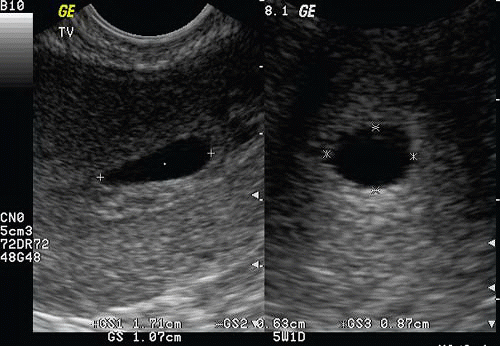
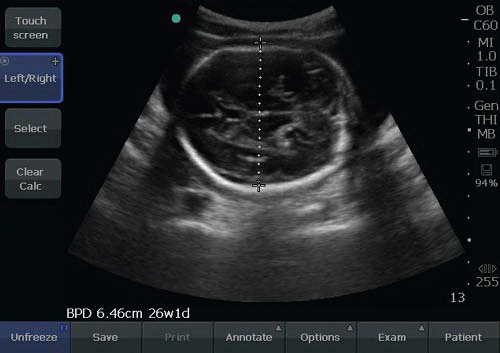
Gestational age may be determined using functions in currently available ultrasound machines. The following measurements can be obtained to provide estimates of gestational age.
Mean Sac Diameter (MSD), or Gestational Sac Size (GSS). In early pregnancy the gestational age can be determined from the diameter of the gestational sac (Fig. 15.11; eFig. 15.12). The earliest that the gestational sac can be visualized by transvaginal ultrasound is at a diameter of 2 to 3 mm, which correlates with a gestational age between 4 and 5 weeks.
Crown-Rump Length (CRL). When an embryo is present, the CRL can be measured with calipers defining the length of embryo (excluding the legs and yolk sac) (Figs. 15.7 and 15.12; eFigs. 15.13 and 15.14).
Once the fetus has reached 13 weeks gestational age, other methods of determining gestational age are used, such as head circumference (HC), biparietal diameter (BPD), abdominal circumference (AC) and femur length (FL) (Figs. 15.13 and 15.14; eFig. 15.15).
PATHOLOGY
The term abnormal pregnancy refers to a number of entities, including ectopic pregnancy, nonviable pregnancy/ embryonic demise and molar pregnancies. These pathologic entities maybe identified on the initial evaluation by ultrasound during the initial ED visit or on subsequent visits. Because the management of IUP, ectopic pregnancy, and embryonic demise differ significantly, it is important to differentiate them accurately and expeditiously. Abnormal pregnancy should be suspected when an IUP is not initially visualized on bedside ultrasound or when the normal appearance of the gestational sac, yolk sac, or the fetal heart rate is absent. Definitive diagnosis of IUP or abnormal pregnancy can be made on the initial visit with ultrasound, β-hCG levels, and surgical evaluation, or on subsequent visits. However, the emphasis of bedside ultrasound should be to identify IUP rather than abnormal pregnancy.
Ectopic Pregnancy
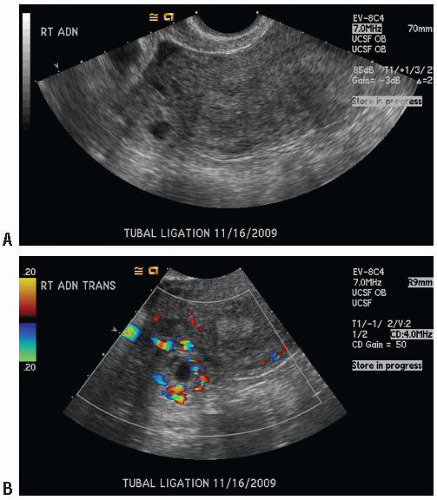
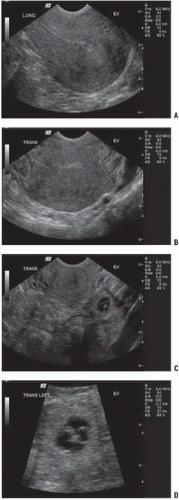
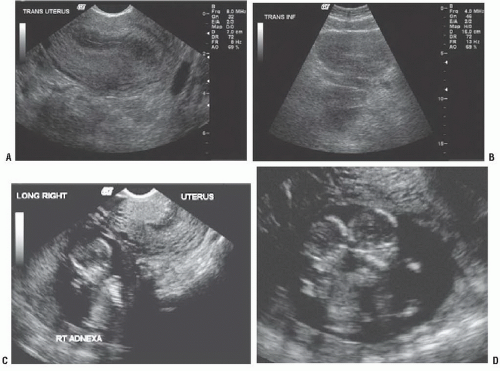
The simplest, albeit nonspecific, finding in ectopic pregnancy is failure to visualize an IUP in a patient who is known to be pregnant (positive pregnancy test). Specific sonographic findings for ectopic pregnancies depend upon location, gestational age, and whether they have ruptured. There are several types of ultrasound findings for ectopic pregnancy that provide varying degrees of certainty. Ultrasound is diagnostic for ectopic pregnancy when an extrauterine gestational sac is visualized containing a fetus or yolk sac, although this is a relatively uncommon finding (Figs. 15.15, 15.16 and 15.17;
eFigs. 15.16 and 15.17; VIDEOS 15.10-15.13). In some cases, the extrauterine gestational sac appears as a tubal ring, a thick-walled echogenic mass surrounding a cystic fluid collection. The tubal ring is highly suspicious for ectopic pregnancy; when seen, the risk of ectopic pregnancy is reported to exceed 95%, although it occurs in only 20% of ectopic pregnancies diagnosed by ultrasound (Figs. 15.15 and 15.18; eFigs. 15.18 and 15.19) (22). A complex adnexal mass separate from the ovary is highly suggestive of ectopic pregnancy, and is seen in 60% of ectopic pregnancies (Figs. 15.19, 15.20, 15.21 and 15.22; eFig. 15.20;
VIDEOS 15.10-15.13). In some cases, the extrauterine gestational sac appears as a tubal ring, a thick-walled echogenic mass surrounding a cystic fluid collection. The tubal ring is highly suspicious for ectopic pregnancy; when seen, the risk of ectopic pregnancy is reported to exceed 95%, although it occurs in only 20% of ectopic pregnancies diagnosed by ultrasound (Figs. 15.15 and 15.18; eFigs. 15.18 and 15.19) (22). A complex adnexal mass separate from the ovary is highly suggestive of ectopic pregnancy, and is seen in 60% of ectopic pregnancies (Figs. 15.19, 15.20, 15.21 and 15.22; eFig. 15.20;  VIDEOS 15.14-15.16). While any adnexal mass other than a simple cyst is less specific than a visualized extrauterine gestational sac or tubal ring, it is the most sensitive for ectopic pregnancy (22). In a study of bedside ultrasound to detect ectopic, emergency sonologists detected the tubal ring and complex adnexal mass in proportions similar to those identified by radiologists (5).
VIDEOS 15.14-15.16). While any adnexal mass other than a simple cyst is less specific than a visualized extrauterine gestational sac or tubal ring, it is the most sensitive for ectopic pregnancy (22). In a study of bedside ultrasound to detect ectopic, emergency sonologists detected the tubal ring and complex adnexal mass in proportions similar to those identified by radiologists (5).
eFigs. 15.16 and 15.17;
 VIDEOS 15.10-15.13). In some cases, the extrauterine gestational sac appears as a tubal ring, a thick-walled echogenic mass surrounding a cystic fluid collection. The tubal ring is highly suspicious for ectopic pregnancy; when seen, the risk of ectopic pregnancy is reported to exceed 95%, although it occurs in only 20% of ectopic pregnancies diagnosed by ultrasound (Figs. 15.15 and 15.18; eFigs. 15.18 and 15.19) (22). A complex adnexal mass separate from the ovary is highly suggestive of ectopic pregnancy, and is seen in 60% of ectopic pregnancies (Figs. 15.19, 15.20, 15.21 and 15.22; eFig. 15.20;
VIDEOS 15.10-15.13). In some cases, the extrauterine gestational sac appears as a tubal ring, a thick-walled echogenic mass surrounding a cystic fluid collection. The tubal ring is highly suspicious for ectopic pregnancy; when seen, the risk of ectopic pregnancy is reported to exceed 95%, although it occurs in only 20% of ectopic pregnancies diagnosed by ultrasound (Figs. 15.15 and 15.18; eFigs. 15.18 and 15.19) (22). A complex adnexal mass separate from the ovary is highly suggestive of ectopic pregnancy, and is seen in 60% of ectopic pregnancies (Figs. 15.19, 15.20, 15.21 and 15.22; eFig. 15.20;  VIDEOS 15.14-15.16). While any adnexal mass other than a simple cyst is less specific than a visualized extrauterine gestational sac or tubal ring, it is the most sensitive for ectopic pregnancy (22). In a study of bedside ultrasound to detect ectopic, emergency sonologists detected the tubal ring and complex adnexal mass in proportions similar to those identified by radiologists (5).
VIDEOS 15.14-15.16). While any adnexal mass other than a simple cyst is less specific than a visualized extrauterine gestational sac or tubal ring, it is the most sensitive for ectopic pregnancy (22). In a study of bedside ultrasound to detect ectopic, emergency sonologists detected the tubal ring and complex adnexal mass in proportions similar to those identified by radiologists (5).There are several indirect findings suggestive of ectopic pregnancy when the extrauterine gestation is not visualized, such as free fluid in the cul-de-sac, or empty uterus. Patients with an empty uterus are five times more likely to have an ectopic pregnancy compared with those with a fluid collection or debris in the uterus (Fig. 15.23;  VIDEOS 15.17 and 15.18) (13). Free fluid, especially large or complex fluid (echogenic, layering, or clotted blood), is strongly associated with ectopic pregnancy.
VIDEOS 15.17 and 15.18) (13). Free fluid, especially large or complex fluid (echogenic, layering, or clotted blood), is strongly associated with ectopic pregnancy.
 VIDEOS 15.17 and 15.18) (13). Free fluid, especially large or complex fluid (echogenic, layering, or clotted blood), is strongly associated with ectopic pregnancy.
VIDEOS 15.17 and 15.18) (13). Free fluid, especially large or complex fluid (echogenic, layering, or clotted blood), is strongly associated with ectopic pregnancy.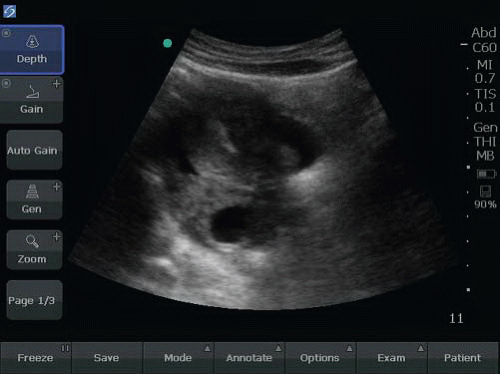 FIGURE 15.18. Transabdominal Sagittal View of an Empty Uterus with Visible Empty Gestational Sac or Tubal Ring Seen Underneath the Uterus. Free fluid can be seen surrounding the uterus. |
Cornual, interstitial, cervical ectopics
The vast majority of ectopic pregnancies are located in the fallopian tubes, but ectopic pregnancies have been identified in interstitial, cervical, ovarian, abdominal, and cesarean scar locations (3,23,24). Pregnancies that are placed eccentrically
in relation to the normal uterine site of implantation may be misinterpreted as an IUP. Pregnancies may implant in any portion of the periphery of the uterus (cornual, interstitial, and cervical) and be easily misdiagnosed as a normal IUP. It is important that the sonographer detects myometrium surrounding the entire gestational sac and it be at least 5 mm thick to help rule out an interstitial ectopic pregnancy (Fig. 15.24; VIDEO 15.19). Rupture may result in massive bleeding. Management of these pregnancies may vary, but in general are treated by surgical resection and usually in an open manner, although more conservative approaches have been suggested (25,26).
VIDEO 15.19). Rupture may result in massive bleeding. Management of these pregnancies may vary, but in general are treated by surgical resection and usually in an open manner, although more conservative approaches have been suggested (25,26).
in relation to the normal uterine site of implantation may be misinterpreted as an IUP. Pregnancies may implant in any portion of the periphery of the uterus (cornual, interstitial, and cervical) and be easily misdiagnosed as a normal IUP. It is important that the sonographer detects myometrium surrounding the entire gestational sac and it be at least 5 mm thick to help rule out an interstitial ectopic pregnancy (Fig. 15.24;
 VIDEO 15.19). Rupture may result in massive bleeding. Management of these pregnancies may vary, but in general are treated by surgical resection and usually in an open manner, although more conservative approaches have been suggested (25,26).
VIDEO 15.19). Rupture may result in massive bleeding. Management of these pregnancies may vary, but in general are treated by surgical resection and usually in an open manner, although more conservative approaches have been suggested (25,26).Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree