Presentation and Presenting Images
A 69-year-old female presents for routine screening mammography.
65.2 Key Images
65.2.1 Breast Tissue Density
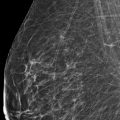
The breasts are heterogeneously dense, which may obscure small masses.
65.2.2 Imaging Findings
The imaging of the right breast is normal (not shown). The left breast demonstrates a focal asymmetry at the 11 to 12 o’clock location in the middle depth, 6 cm from the nipple (circle in ▶ Fig. 65.3 and ▶ Fig. 65.4). There are coarse calcifications nearby but these calcifications have been stable for many years.
Because the screening mammogram was performed without digital breast tomosynthesis (DBT), DBT followed by ultrasound is the next step in the imaging evaluation. DBT can confirm a true mass lesion or determine if the screen-detected asymmetry is the result of parenchymal overlap. If the finding is a true lesion, sonography is recommended for further characterization and biopsy. If the mass is a true lesion and not identified by ultrasound, tomosynthesis-directed stereotactic-guided biopsy can be performed.
65.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
65.4 Diagnostic Imaging
( ▶ Fig. 65.5, ▶ Fig. 65.6, ▶ Fig. 65.7, ▶ Fig. 65.8, ▶ Fig. 65.9, ▶ Fig. 65.10, ▶ Fig. 65.11, ▶ Fig. 65.12, ▶ Fig. 65.13, ▶ Fig. 65.14, ▶ Fig. 65.15, ▶ Fig. 65.16)
65.4.1 Imaging Findings
Slices from the left DBT movies ( ▶ Fig. 65.5, ▶ Fig. 65.6, ▶ Fig. 65.7, ▶ Fig. 65.8, ▶ Fig. 65.9, ▶ Fig. 65.10, ▶ Fig. 65.11, and ▶ Fig. 65.12) demonstrate a focal asymmetry (circle) measuring 7 mm at the 12 o’clock location in the middle depth, 6 cm from the nipple. There is associated architectural distortion.
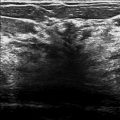
On left breast ultrasound, there is a subtle area of architectural distortion at the 11 to 12 o’clock location, 6 cm from the nipple ( ▶ Fig. 65.13 and ▶ Fig. 65.14), corresponding to the area of architectural distortion on the mammogram and DBT. Ultrasound-guided core needle biopsy is indicated and subsequently performed. Pathology was consistent with ductal carcinoma in situ (DCIS). A postbiopsy mammogram shows mammographic–sonographic correlation and adequate placement of the postbiopsy clip (arrow in ▶ Fig. 65.15 and ▶ Fig. 65.16).
65.5 BI-RADS Classification and Action
Category 5: Highly suggestive of malignancy
65.6 Differential Diagnosis
Breast cancer (ductal carcinoma in situ): D CIS most commonly presents as microcalcifications but may present as a mass, an architectural distortion, and as developing densities.
Breast cancer (invasive carcinoma): Invasive ductal carcinoma is more likely than DCIS to present as a focal asymmetry. This would be a concordant diagnosis.
Pseudomass: DBT can confirm a true mass lesion or determine if the screen-detected asymmetry is the result of parenchymal overlap.
65.7 Essential Facts
The incidence of DCIS rose from 1.87 per 100,000 in 1973 to 1975 to 32.5 in 2004. The increased use of mammography during this time period accounts for some but not all of the increase in incidence.
DCIS typically presents as calcifications on mammography. The morphology of DCIS calcifications on mammography includes amorphous, coarse heterogeneous, fine pleomorphic, and fine-linear or fine-linear branching types.
Not all cases of DCIS present as calcifications. Less common presentations include masses, asymmetries, architectural distortions, dilated retroareolar ducts, or developing asymmetries.
Although unable to perform magnification views of calcifications suspicious for DCIS, DBT can detect, characterize, and localize the less common presentations of DCIS.
65.8 Management and Digital Breast Tomosynthesis Principles
DBT has shown superior performance in the detection of masses and architectural distortions. In this case specifically, the architectural distortion associated with the focal asymmetry was undetected on the conventional two-dimensional (2D) mammogram. DBT imaging can better characterize masses and architectural distortions due to the reduction in breast parenchymal overlap.
Subtle lesions may only be identifiable on DBT and will require DBT-tomosynthesis-directed stereotactic-guided biopsy. Using the breast tomosynthesis unit, one DBT scan is performed, the lesion is targeted, and the x, y, z location of the lesion calculated directly from the three-dimensional (3D) image.
Virnig and colleagues (2010) concluded that further investigation is needed to the determine which DCIS lesions are destined to become clinically problematic. DBT may be helpful in this investigation.
65.9 Further Reading
[1] Evans A, Pinder S, Wilson R, et al. Ductal carcinoma in situ of the breast: correlation between mammographic and pathologic findings. AJR Am J Roentgenol. 1994; 162(6): 1307‐1311 PubMed
[2] Ikeda DM, Andersson I. Ductal carcinoma in situ: atypical mammographic appearances. Radiology. 1989; 172(3): 661‐666 PubMed
[3] Mitnick JS, Roses DF, Harris MN, Feiner HD. Circumscribed intraductal carcinoma of the breast. Radiology. 1989; 170(2): 423‐425 PubMed
[4] Virnig BA, Tuttle TM, Shamliyan T, Kane RL. Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes. J Natl Cancer Inst. 2010; 102(3): 170‐178 PubMed
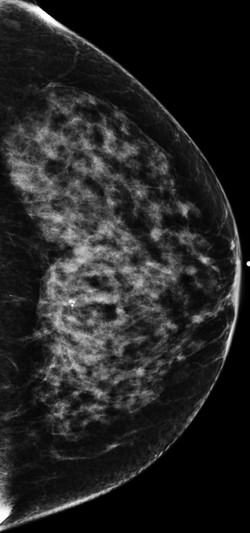
Fig. 65.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree