Follicular Bronchiolitis
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Follicular bronchiolitis to nodular lymphoid hyperplasia (pseudolymphoma), LIP, and lymphoma
Imaging Findings
Centrilobular nodules, faint
Diffuse or lower lung zones
Nodules < 3 mm in diameter
Follicular bronchiolitis centered on airways (leads to centrilobular nodules), LIP more diffuse
Unusual: Cysts, mosaic air-trapping
Top Differential Diagnoses
Respiratory Bronchiolitis
Sarcoidosis
Langerhans Granulomatosis
Lymphocytic Interstitial Pneumonia
Hypersensitivity Pneumonitis
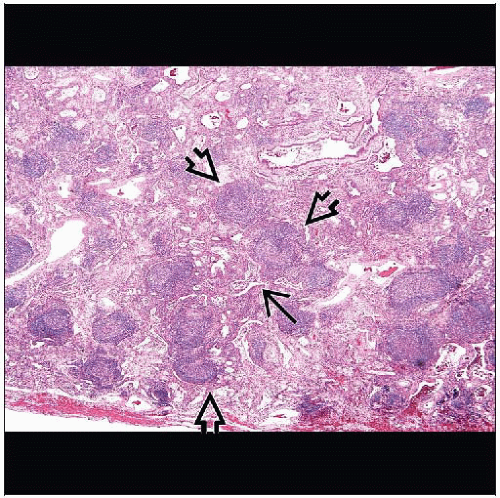
Pathology
BALT extends from nodal clusters in airway bifurcations to lymphocyte clusters at proximity of lymphatics in terminal bronchioles
Idiopathic (but rare, most cases associated with other conditions)
Autoimmune: Sjögren syndrome (25% develop LIP), rheumatoid arthritis
Viral infection: HIV
Immunodeficiency: Common variable immunodeficiency, IgA deficiency
Inhalation: Cigarette smoke, polyethylene-flock, hypersensitivity pneumonitis
Clinical Issues
Diagnosis usually requires surgical biopsy and not transbronchial biopsies
TERMINOLOGY
Abbreviations and Synonyms
Pulmonary lymphoid hyperplasia, lymphocytic interstitial pneumonia (LIP), lymphoid interstitial pneumonia
Diffuse hyperplasia of bronchus-associated lymphoid tissue (BALT), mucosa-associated lymphoid tissue (MALT)
Definitions
Spectrum of lymphoid disorders
Follicular bronchiolitis to nodular lymphoid hyperplasia (pseudolymphoma), LIP, and lymphoma
Nonneoplastic lymphoproliferation must be differentiated from lymphoma by immunologic stains
Monoclonal cell lines in lymphoma, polyclonal in nonneoplastic lymphoproliferative disorders
IMAGING FINDINGS
General Features
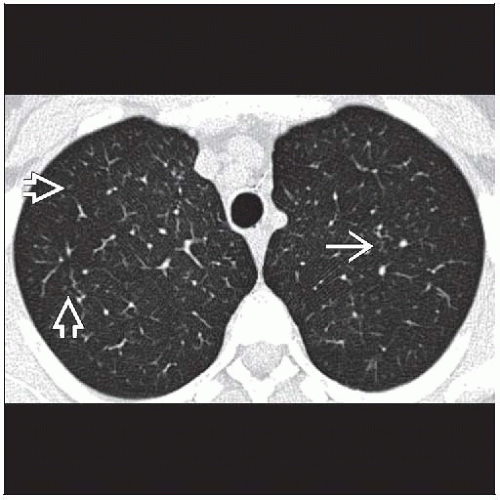
Best diagnostic clue: Centrilobular nodules, faint
Patient position/location: Diffuse or lower lung zones
Size: Nodules < 3 mm in diameter
Morphology: Follicular bronchiolitis centered on airways (leads to centrilobular nodules), LIP more diffuse
CT Findings
Nodules (100%)
Distribution within the lung
Diffuse (66%)
Lower lung zones (25%)
Axial plane: Peripheral lung (70%), central lung (0%), random (30%)
Distribution within secondary pulmonary lobule
Centrilobular (100%)
Peribronchial (40%)
Subpleural (25%)
Size
< 3 mm diameter (100%)
3-10 mm diameter (40%)
> 10 mm diameter (< 10%)
Ground-glass opacities (75%)
Nonsegmental diffuse patchy opacities
Always associated with nodules
As profusion of nodules increases, more likely to have ground-glass opacities
Tree-in-bud opacities (70%)
Less common
Bronchial dilatation (33%)
Bronchial wall thickening (33%)
Emphysema (33%)
Architectural distortion (25%)
Septal thickening (10%)
Mediastinal or hilar lymphadenopathy (50%)
Mildly enlarged, 1-2 nodal groups (will not be large enough to be detected radiographically)
Unusual
Cysts
Mosaic air-trapping
Absent
No honeycombing
No pleural effusions
No “crazy-paving”
Evolution
Relatively stable over time, small series followed mean 4 years
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree