17 Follow-Up and Recurrence The large number of breast cancers diagnosed per year—approximately 200 000 in the United States—and the concomitantly large number of diagnostic and therapeutic interventions carried out each year underscore the important role of follow-up. A local recurrence diagnosed at the average time of 3 years after lumpectomy at or near a lumpectomy site, which is then treated with mastectomy, does not alter the survival outlook of a patient, bleaker when an early chest wall recurrence is found following mastectomy. In addition to follow-up for recurrence, another very important role for clinical and imaging follow-up is to reassure patients that they remain cancer-free. The response to therapy—particularly radiation—will change the appearance of the breast drastically, and post-treatment changes of edema, skin thickening, and a spiculated scar can resemble carcinoma. Monitoring the slow resolution of these breast alterations is very important not only in detection of recurrence but also to allay the nearly constant anxiety and the potentially significant change in life circumstances: psycho-oncology has come to play a major role in the care of breast cancer patients. Because the diagnosis of tumor recurrence initiates a chain of events, one should question whether the detection of certain changes has real therapeutic implications or will merely exacerbate the patient’s fears. Until a few years ago, it was common to conduct intensive pretreatment staging or follow-up programs that included X-rays, radionuclide scans, CT, MRI, ultrasound, and costly laboratory tests to detect metastases to the bone, lung, liver, and CNS. More recent studies have shown, however, that in most cases, particularly when the carcinoma is likely to be Stage 1, the detection of distant metastases and subsequent treatment measures will not improve the prognosis and will at best offer a chance for palliation. Clinical examination remains important in the detection of metastases and can direct the initiation of appropriate palliative treatment. Research continues, however, in identifying successful treatments for advanced cancer patients and there has been recent increased utilization of PET and PETCT when metastatic activity is suspected or highly likely. In the case of local and locoregional recurrences of breast cancer following conservation therapy, however, early detection is meaningful, for it enables the lesion to be treated before it disseminates. Consequently, the use of high-quality imaging equipment is essential in diagnosing this type of recurrence. Recurrent tumors may develop in the chest wall following mastectomy, or within the breast itself following a breast-conserving excision. The contralateral breast may be involved by a second carcinoma or by a metastatic spread from a recurrent tumor. It is equally important to examine the axillary lymph nodes, the supraclavicular and infraclavicular nodes, the internal mammary nodes, and the neck (Table 17.1). A variety of diagnostic methods are available for this (Table 17.2). The selection of diagnostic methods depends on prior treatment and the clinical situation. Mammography is ineffective in evaluating the chest wall following mastectomy, and mammography is unnecessary on the side of mastectomy except for using a spot compression view to alleviate anxiety in a patient who questions a mass or thickening in redundant tissue in the mid-axillary line. The contralateral breast should be screened annually with mammography. Prepectoral recurrences in the subcutaneous tissue or epidermis are diagnosed clinically. Recurrences within or deep to the pectoralis muscle are difficult to detect clinically, however, and ultrasound is the method of choice in these cases. CT or MRI can be helpful as well.
Clinical Significance
Detection of Locoregional Recurrences
|
|
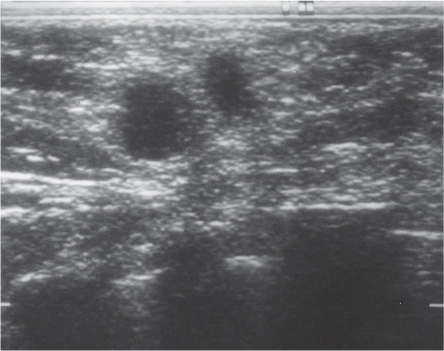
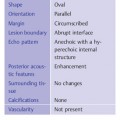
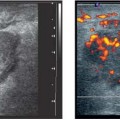
Fig. 17.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Local
Local Intramammary
Intramammary Chest wall
Chest wall Contralateral breast
Contralateral breast Lymph nodes
Lymph nodes Axilla
Axilla Internal thoracic artery
Internal thoracic artery Supra- and infraclavicular
Supra- and infraclavicular Neck
Neck Inspection and palpation
Inspection and palpation Ultrasound
Ultrasound Mammography
Mammography MRI
MRI CT
CT Radionuclide imaging and PET
Radionuclide imaging and PET Fine-needle aspiration or core biopsy
Fine-needle aspiration or core biopsy