Organic
Nuts (peanuts, almonds, walnut, pistachio, etc.)
Seeds (watermelon, sunflower, chickpea)
Fruits (apple, tangerine, peach)
Coffee beans
Dried cereals
Popcorn
Candy
Rhubarb
White cedar
Metallic inorganic
Pins
Hypodermic needles
Bullet
Jewelry: earrings
Dental crowns (Fig. 46.2), implants, bridges
Coins (Fig. 46.4)
Knife and razor blades
Silver Jackson tracheotomy tube
Nail clippers
Nails
Tweezers
Plastic inorganic
Endotracheal tube
Nasopharyngeal Airway
Intubating introducer
Toys and pearls
Condom
Stoma button
Dentures
Plastic wrap
Pen cap
Drug delivery devices (Turbuhaler disc; spray cover)
Mineral
Natural teeth
Bones (chicken, fish, etc.)
Stone
Glass (fragments – Fig. 46.3, cocaine pipe, etc.)
Endogenous
Broncholiths (Fig. 46.5)
Transbronchial erosion
Mediastinal FB: gauze, gauze pledget post-mediastinoscopy
Rib used for tracheoplasty
Esophageal stents
Teflon pledget for reinforcing bronchial stump
Misc
Endoscopic video capsule
Ascaris lumbricoides
Shrimp
Passalid beetle
Medications: ferrous sulfate, aspirin, kaopectate, cholestyramine, phenobarbital, tetracycline, mineral oil, iron sulfate, fentanyl patch
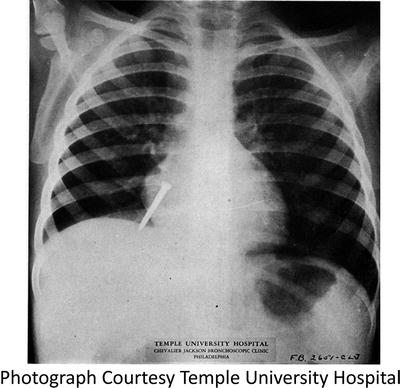
Fig. 46.1
Chest X-ray obtained for Chevalier L. Jackson, M.D. in the evaluation of a suspected foreign body at his bronchoscopy clinic at Temple University Hospital in the 1930s. (Photograph Courtesy Temple University Hospital)
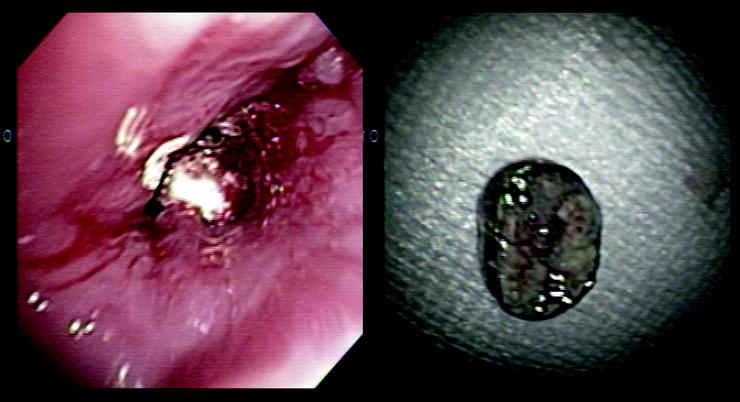
Fig. 46.2
Dental crown impacted in the airway and post removal. (Courtesy H. Colt and S. Murgu, UC Irvine, www.bronchoscopy.org)
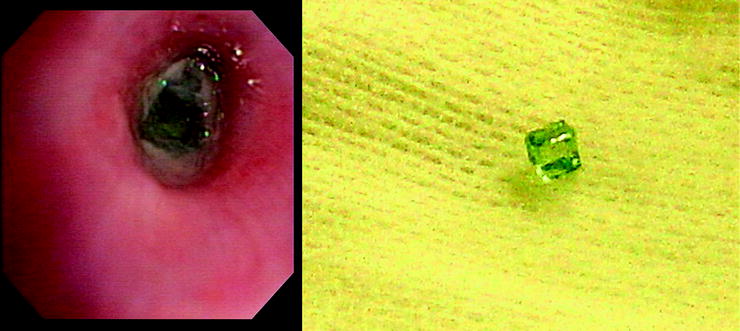
Fig. 46.3
Glass fragment impacted in the airway and post removal. (Courtesy H. Colt and S. Murgu, UC Irvine, www.Bronchoscopy.org)
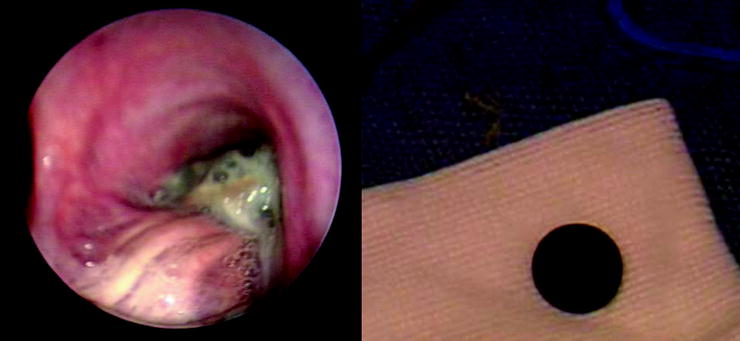
Fig. 46.4
Coin impacted in the airway and post removal. (Courtesy H. Colt and S. Murgu, UC Irvine, www.bronchoscopy.org)

Fig. 46.5
Broncholith eroding into a main stem airway. (Courtesy Daniel Sterman, MD)
The type of foreign body will usually influence the local tissue reaction. While inert foreign bodies may have an irritant effect, the overall inflammatory component is limited. There may be direct tissue injury from aspirated sharp objects such as pins, knife blades, razors, glass shards, or nail clippers. Conversely, some objects particularly organic substances, such as nuts, can create an intense inflammatory response. It has been reported that granulation tissue can result within a few hours of contact with the airway wall. Aspiration of various medications, including tetracycline and iron tablets, can also lead to significant inflammatory responses. Expansion of foreign bodies, both organic material and medications, is caused by rehydration. These rehydrated items can become wedged, thus compounding the difficulties of removal, especially when concurrent granulation tissue is present.
Broncholiths are an endogenous foreign body that can erode into the airway. Other eroding foreign bodies are iatrogenic. Examples have included an autologous grafted rib used for tracheoplasty, gauze pledgets, and esophageal stents. With newer technology, capsule endoscopes are a more common cause of iatrogenic foreign bodies. After snare cautery through the stalk of a pedunculated airway mass, distal escape of the excised tumor acts as a foreign body. These freed tumors may oscillate from side to side and occasionally present difficulties if they are calcified or very large.
Because of their shape and aerodynamic qualities, some foreign bodies may lodge very deep. This can be due to initial aspiration or distal migration. Once distal impaction occurs, as in grass inflorescence, the significant inflammatory response may require surgical wedge or lobar resection.
Clinical Presentation
Upon aspiration of a foreign object, patients present with various acuities and wide-ranging symptoms. Acute asphyxic choking with rapid decompensation and death may occur. Basic life support training suggests evaluating the oropharynx for obstructing material in evaluating a patient with cardiopulmonary arrest. Patients experiencing asphyxia will be unable to talk, usually be unable to cough, and commonly exhibit the universal choking sign of having their hands around their throat. Significant symptoms may also occur in acute non-asphyxic aspiration. If a foreign body is subglottic but extrathoracic, inspiratory stridor may result. Acute dyspnea and the sudden onset of wheezing may also occur with high-grade narrowing of either tracheal or main bronchial lumens. Although these symptoms may persist in many patients, the acute episode is often followed by a rather asymptomatic period. This period may be marked with an intermittent yet persistent cough, recurrent respiratory tract infections, or an asthmatic syndrome. Importantly, 25% of patients may present with no symptoms. Because an extensive history may reveal the likely diagnosis in only half of all patients, the highest index of suspicion must be maintained in order to pursue a proper diagnostic paradigm.
The examination of the patient may not reveal anything suggestive of a foreign body if the material is lodged distally. Alternatively, auscultation may reveal stridor, wheezing, rales, or simply decreased breath sounds.
Significant delay in presentation occurs for any number of reasons in some cases. Although it is not uncommon for delays in diagnosis to extend for weeks to months, years may even pass, with the longest delay reported by Chevalier Jackson at a staggering 45 years. Furthermore, delays in therapy may also arise. An extreme example was a diver who aspirated foreign body while working at a United Kingdom research base during the Antarctic winter that prohibited early removal or evacuation. Most patients do not encounter such hurdles; however, many rural hospitals and facilities do not have the local expertise, therefore necessitating transfer. Depending upon the type of foreign body, its location, and the inflammatory response, even larger centers may not have the experienced team to remove an impacted object, potentiating the delays before removal.
Complications of Long-Standing Foreign Bodies
As noted previously, a foreign body may incite a local inflammatory response or proliferation of granulation tissue. Secondary infectious complications occur due to impacted objects. Recurrent post-obstructive pneumonias or lung abscess can develop. Unusual infections including endobronchial actinomycosis and botryomycosis have been described. Regions subjected to chronic inflammation or infection may develop bronchiectasis or bronchomalacia. Bronchiectasis develops in 25% of children in whom the diagnosis was delayed greater than a month. The inflorescences of many grasses including “Timothy grass” are a well-known cause of bronchiectasis. Erosion through the bronchial wall may create a fistula. Foreign bodies have been reported to have migrated into the pleural space, the pericardium, and even into the intestine. Aspiration of some medications or chronic inflammatory states may cause stricture rather than bronchiectasis. Iron tablets can cause a severe chemical burn to the bronchial tree with subsequent necrosis and cicatricial scarring.
Migration of long-standing extrapulmonary foreign bodies may also cause chronic infection once in the airway. Such was the case of an infantry soldier who was found with a bullet in his airway after being shot 53 years before during World War II.
Yildizeli and associates evaluated an animal model for radiographic and histological correlation. They found a progressive effect of leukocyte infiltration with edema followed by mononuclear cells and macrophages. This infiltrative process created fibrosis and bronchial cartilage destruction. Tang and colleagues showed that foreign bodies may incite airway remodeling via matrix metalloproteinase’s and hydroxyproline.
Radiographic Investigation
While some of the most impressive images of foreign bodies are radiographic, such as knife blade or large screw in the main stem (see Fig. 46.1), most radiographic studies are of limited diagnostic assistance. Radiographic evaluation should never be used to exclude an airway foreign body. Overall, CT scanning is much better for identifying potential airway objects. However, as reported by Zissin, false positives do occur. Routine chest radiography and fluoroscopy may be helpful when looking for indirect evidence of obstruction but must never be used as an independent imaging modality. Most foreign bodies are radiolucent and hence not clearly visible on routine imaging. In the experience reported by Srppnath and later by Mise, only 2–7% of foreign bodies were radio-opaque on routine chest radiography. Indirect evidence to suggest a foreign body includes nonspecific signs such as segmental or lobar atelectasis, air trapping, infiltrates/consolidation, subcutaneous emphysema, or mediastinal shift. Only 4% had normal chest radiographs in Srppnath’s retrospective series. These changes are best seen when comparing full inhalation and expiratory imaging. Newer multi-slice CTs and virtual bronchoscopy may provide clearer insight, as demonstrated by Cho and Sodhi, respectively.
Unusual anatomy may suggest a bronchogenic carcinoma. A mass near the trachea has been reported to be a foreign body with inflammatory changes in a tracheal bronchus. While this is a rare case, multiple reports show endoluminal biopsies for endobronchial cancer with foreign material and inflammation. Therefore, while rare in comparison to lung carcinoma, it is possible for an “endobronchial tumor” or “peripheral lung mass” seen on CT imaging to be a complication of an aspirated foreign body.
When presented with a nondiagnostic imaging evaluation, any history remotely suggestive of an aspirated foreign body warrants an airway inspection with flexible bronchoscopy.
Therapeutic Approaches
Bronchial anatomy predisposes the intermediate bronchus and right lower lobe to the majority of aspirations (see Table 46.2). This is due to its larger size and its more vertical orientation when compared to the left main stem. However, anatomy and body position during the aspiration event may alter this predisposition. In fact, any lobe, segment, or subsegment may be the site of impaction. The seven rules of bronchoscopy should always be considered when dealing with bronchoscopic removal of an airway foreign body (see Table 46.3).
Table 46.2
Location of foreign body
Trachea (%) | Right (%) | RMS/RBI (%) | RUL | RML (%) | RLL (%) | Left (%) | LMS (%) | LUL (%) | LLL (%) | Carina (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Zissin | 74 | 16 | 11 | 47 | 26 | 11 | 4 | 11 | |||
Athanasiadi | 4 | 44 | 35 | 9 | 52 | 30 | 13 | 9 | 5 | ||
Eroglu | 10.90 | 52.70 | 30 |
Table 46.3
Mehta’s seven rules of successful bronchoscopy
1 | Complications occur when a bronchoscopy is performed for unclear reasons or the wrong indication |
2 | Preparation ensures 50% success rate |
3 | Bronchoscopy is a three-handed procedure |
4 | A good bronchoscopist has excellent skills, but an excellent bronchoscopist is surrounded by excellent support and backup |
5 | Time and commitment are essential |
6 | Know your limitations |
7 | Every case should be viewed as a teaching and training opportunity |
In patients who present with stridor or severe dyspnea suggestive of proximal obstruction, heliox should be utilized. The titration of heliox can be based upon the predominant effect on the respiratory system. If the minute volume is most affected, a higher percentage of helium (80:20) may be more useful to reduce the viscosity of the gas. Patients with combined hypoxemia and ventilatory defects benefit from lower percentages of helium and increased oxygen. Use of 30–50% FIO2 may maximally balance oxygen needs and improved gas flow.
Preparation
Should all foreign bodies be removed? Chevalier Jackson reported a success rate of 98% and a consequent reduction in mortality from 24% to 2% using rigid bronchoscopy. As a general rule, all foreign bodies should be removed. Clinical expertise and an experienced team will substantially increase the likelihood of success. With the proper team, correct instrumentation, and an experienced bronchoscopist, virtually all foreign bodies are safely and successfully removed. While a multidisciplinary approach is helpful in most circumstances, the requirement for thoracotomy is minimal.
In many cases, moderate sedation with opiates and benzodiazepines is insufficient. This is particularly true when there may be a need to change from flexible to rigid bronchoscopy. Monitored anesthesia care (MAC) or general anesthesia is frequently more appropriate. Consulting anesthesia is frequently a value-added use of time. Involving anesthesia allows safe titration of the sedation requirements as the procedure warrants. Furthermore, it allows the endoscopist to focus on the task at hand. When compared to inhaled anesthetics, total intravenous anesthesia (TIVA) is very helpful in maintaining a stable level of anesthesia when alternating between airway interventions and the potential tidal volume loss encountered during rigid bronchoscopy.
It is always best to use the oral approach rather than the trans-nasal approach because the foreign body may not traverse the turbinate’s in the nose. Selection of the appropriate airway support is important. The choice of direct bronchoscopy, laryngeal mask airway, or endotracheal intubation should be based upon the medical condition of the patient and the foreign body being removed. In addition, the pre-sedation evaluation of the airway is critical even if intubation is not planned. What difficulties may be encountered if the patient requires urgent intubation or rigid bronchoscopic intubation? Pre-procedural assessment of the Mallampati score, thyromental distance, mandibular opening, and cervical range of motion are all important to the pre-procedural planning. Evaluation for loose teeth is also critical. Notwithstanding the medical-legal need to document their presence, it is important to understand the potential to leave a new foreign body in the airway.
Flexible Versus Rigid Bronchoscopy
Much has been written regarding the proper choice of bronchoscope. The standard of care had been rigid bronchoscopy for all foreign bodies. With the advent of large working channel bronchoscopes and a wider array of instruments, retrieval of impacted objects has become routine with the flexible bronchoscope. A success rate of 86% has been reported with the use of flexible bronchoscopy. There are institutional and practice preferences that drive the approach. For most patients, the decision must be made, taking into consideration both operator comfort and the circumstances presented in each unique situation. In patients with stridor and partially obstructing tracheal foreign bodies, a rigid bronchoscope is often the better instrument. In some cases, pushing the object distally to initially improve airflow is required. This may be difficult with a flexible bronchoscope. Any patient presenting with respiratory failure is best managed with a rigid bronchoscope. Operator inexperience or lack of training must never be the reason for failing to use a rigid bronchoscope when one is required. The patient should be transferred to a center with an experienced team before complications ensue, impairing removal or patient safety.
Removal Procedure
Regardless of which endoscopic approach is taken, an initial surveillance of the entire visible tracheobronchial is required. The exception to this rule is when tracheal foreign bodies are found or the patient is in extremis. If able, the bronchoscopist should understand what other anatomical variations or potential secondary foreign bodies are present that may complicate the primary procedural goal.
Proper preparation is a significant indicator of success, and this includes the airway itself. As noted previously, granulation tissue may initially suggest a tumor or may limit the approach to an impacted foreign body. When presented with exuberant granulation tissue, several potential approaches may be helpful. Preparing the airway is critical in some circumstances. Granulation may be reduced by use of argon plasma coagulation or low wattage use of the Nd:YAG laser. Caution must be observed when using thermal techniques if one is unsure of the foreign body and its inflammability. When available, cryotherapy may also be utilized to reduce the granulation tissue and limit the risk of fire with unknown materials. Endobronchial injections may be beneficial. Use of a 23–25 gauge sclerotherapy needle with 1:10,000 epinephrine can be helpful in preemptively controlling bleeding from these vascular tissues. Intralesional and submucosal injection of triamcinolone acetonide can help reduce the inflammatory response if waiting for a second procedure is a viable option.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree