Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Introduction
There are multiple imaging modalities to evaluate the spine. The type of imaging tool for the spine depends on the type of disease, the amount of radiation hazard, as well as contraindications and any allergy to contrast.
Among the multiple imaging strategies, computed tomography (CT) is a reliable method to evaluate the spine and has better sensitivity for bony abnormality than radiography or magnetic resonance imaging (MRI). In the past, the time factor limited the use of CT. However, owing to the development of fast spiral CT and multidirectional CT (MDCT), the whole spine can be examined in a very short time. However, CT is less sensitive to a patient’s movement than MRI. Now, it is widely applied to assess trauma, deformity, metastasis, and pre- and postoperative analyses.
MRI is one of the most sensitive and specific modalities to visualize the spine. Furthermore, there are no risks of radiation hazard. It provides information about the spinal neural structures including cord, cauda equina and roots, the vertebral bodies, and intervertebral disc. Multiple sequences can be obtained in different planes and each sequence helps in evaluating various changes of the spine. The most commonly using sequences include sagittal and axial T1 and T2, and a sagittal STIR (short tau inversion recovery). Postcontrast T1-weighted images are useful for evaluating spinal infections, postoperative complications, vascular malformation, primary spinal tumors, and metastases. STIR sequences are beneficial in assessing marrow edema, which demonstrates an increased signal on these sequences.
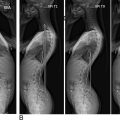
In most cases, spine CT and MR images are obtained to focus on the region of interest where the pathology exists. However, full-length spine examination can be helpful for a more comprehensive evaluation and early detection of disease and trauma ( Fig. 1 ). Therefore, the aim of this chapter was to describe when and how full-length spine evaluation through CT and MRI is applied.

Methodology
A literature review using PubMed and Google Scholar was performed. To identify relevant studies, search was conducted on studies in English published between 2000 and February 2020 using various combinations of the following key words: “full-length spine,” “entire spine,” “whole spine,” “imaging,” “computed tomography,” and “magnetic resonance imaging.” Based on this search, 127 studies were initially detected. After excluding articles about rare disease, technical aspects of CT and MRI, measurement, and imaging protocol, 56 articles were selected. After an internal peer review with all the authors of this article and a supplementary search that involved bibliographic screening and citation tracking associated with individual spine pathology, 24 articles of interest were finally selected ( Fig. 2 ). Those articles are categorized as “trauma,” “deformity,” “infection,” “axial spondyloarthropathy,” and “spinal metastasis” described in the following sections.

Contributions of Full-Length Spine CT and MRI
Trauma
When trauma to the spine occurs, based on physical examination and simple radiography findings, targeted CT and/or MRI is performed specifically at the region of the affected spine for further imaging workup. However, if the patient sustains high-energy trauma or multiple trauma, that regional imaging can be insufficient. In high-energy or polytrauma patients, once the patient’s condition is deemed stable, unforeseen injuries to the spine should be delineated accurately as symptoms of a spine injury may be masked by concomitant injuries, patient’s state of consciousness ( Fig. 3 ), spinal cord injury or shock. In these situations, full-length spine evaluations with CT and/or MRI are essential.

In patients with high-energy blunt trauma, Deunk et al. reported that the nontargeted CT detected 8.2% more spine injuries unrevealed by simple radiographs than the targeted CT. In a prospective study, spinal fractures were prevalent in 30.2% of the cases of high-energy trauma. Among patients with a cervical fracture, 37.5% had a fracture that unrevealed on radiographs of the cervical spine but were first diagnosed by a CT scan. Patients with a thoracolumbar fracture did not have clinical symptoms of a fracture in 14% of cases but had a fracture revealed by CT in those 14%. Therefore, Takami et al. postulated that the full-length spine CT should be taken to evaluate all high-energy trauma patients.
The application of full-length MRI in spine trauma patients remains controversial. Atsina et al. described that full-length MRI is not usually recommended in patients with spine trauma. When the full-length MRI is performed in patients with blunt trauma after full-length spinal CT, most additional spinal injuries detected on MRI were bone contusions and mild compression fractures. These additional spinal diagnoses are unlikely to change the management or treatment. Therefore, the targeted MRI is more useful in patients with high-energy blunt trauma. However, Kanna et al. reported that full-length sagittal T2-weighted images help diagnose multilevel noncontiguous spinal injuries in spinal trauma patients and can be performed in approximately 4 min without radiation hazard.
Deformity
Spinal deformity is a complex disease with different three-dimensional abnormalities that often involve the entire spine. In cases with a complex or severe spinal deformity, full-length spine CT should be taken of the entire spine as plain radiography alone is insufficient to visualize complicated abnormalities of the deformity. Furthermore, in comparison with radiography, full-length spine CT scanning provides additional information about extent of rotation of the spine; segmentation defects; three-dimensional reconstruction and detection of bony spurs in diastematomyelia; and associated congenital anomalies of ribs, scapula, and pelvis.
Full-length spine CT is also useful for surgical planning. Current surgical techniques for deformity correction allow surgeons to effectively correct coronal, sagittal, and rotational aspects of spinal deformity. Multiplanar reconstruction of the axial CT images is important, especially when trying to understand the anatomy of deformity, and allows visualizing levels where osteotomies or resections are planned. The CT scan allows surgeons to understand the pedicle anatomy including the width, depth, and trajectory of the pedicles. During a deformity surgery, caution must be placed when placing screws in the pedicles, especially on the concave side of curvature where pedicles are extremely narrow and the spinal cord is vulnerable to iatrogenic injuries due to restricted epidural space. Preoperative full-length spine CT in this context has been recommended because of the high probability of the presence of narrow pedicles. It also allows surgeons to identify pseudarthroses if the patients underwent previous fusion surgery. Postoperative full-length spine CT is considered for patients with a new neurologic deficit after surgery. Specifically, a postoperative CT can identify potential pedicle screw malposition that may be causing postoperative neurological symptoms.
Full-length spine MRI can be obtained for deformity patients who develop neurologic symptoms or for preoperative planning. The MRI provides visualization of neurological structures, helps determine appropriate levels of surgery, and can assist in the evaluation for adjacent-level pathology when fusion extension is considered. MRI is also essential for the patients with an unusual curve pattern and for those patients who should be assessed on the neural axis. It is important to identify whether syrinx, tethering of the spinal cord, intramedullary tumors, or Chiari malformations are present. The presence of those intraspinal anomalies without neurological findings in idiopathic scoliosis has been estimated between 4 and 26% and associated with neurological complications resulted from correction surgery. Stenosis or cord impingement secondary to severe deformity can be visualized by full-length MRI. In kyphoscoliosis, the level of cord compression should be identified preoperatively and always on the concave pedicle. These regions of compression may require a resection of that pedicle with the remaining body during deformity surgery.
Infection
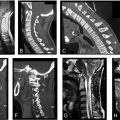
The diagnosis of spinal infection can be difficult and even delayed because clinical manifestations widely vary and, at times, may be equivocal. Physicians have relied heavily on imaging modalities due to difficulty in detecting spinal infection. Among imaging modalities, MRI plays a pivotal role in the diagnosis and management of spinal infection with a sensitivity, specificity, and accuracy above 90%.
If the spinal infection is likely localized, it may not be necessary to obtain imaging along the full length of the spine. However, identification of one infected site in the spine cannot rule out the infection in multiple regions of the spine. The areas adjacent to anterolateral vertebral endplates have abundant vascular supply and are the most common regions where pyogenic, tuberculous, and other spinal infections can present. Associated edema is commonly pronounced and affects the entire vertebral body and intervertebral disc. If there is epidural involvement associated with neurologic symptoms, it is recommended to obtain full-length spine MRI to assess for epidural abscess spread. Among spinal infections caused by various organisms, mycobacterium tuberculosis is notorious for multifocality, and the subligamentous spread of infection to multiple levels is an imaging hallmark of the disease. The infection typically starts in the anterior aspects of the vertebral body adjacent to the intervertebral disc and then spreads to the vertebral bodies under the anterior longitudinal ligaments involving multiple adjacent vertebrae. Through valveless vein system, noncontiguous lesions at additional levels may be impacted.
The incidence of multifocal spinal infection has varied from around 4% to 23%. Mann et al. evaluated 24 patients with spondylitis and found 21 patients had single-level infections , while 1 (4%) had multisegmental infection. Ledermann et al. found 7 (16%) out of 44 patients with disc infection had involvement at several spinal levels. Cox et al. reported that 82 patients with single-level infection performed full-length MRI examination and 19 (23%) patients had additional noncontiguous sites of infection. Remote levels of spondylodiscitis were also present in 11 patients (13%). In cases of multifocal spinal tuberculosis, the reported incidence varies, ranging from 1.1% to 71.4%. Kaila et al. reported a very high incidence of 71.4%, but their data are likely overestimated due to the small number of cases presented. According to a retrospective study, 47 (25.1%) out of 187 patients with spinal tuberculosis had multifocal spinal tuberculosis.
In the setting of spinal infection, full-length spine MRI can be used as a diagnostic screening test to detect multifocal lesions, even if the patients do not have clinical symptoms, and provides early detection of spinal infection, thus preventing progression of osteomyelitis. In regard to the management and treatment of spinal infection, the detection of an epidural abscess or other infective lesions remote from the site of a known uncomplicated spinal infection may result in a change of management.
Axial Spondyloarthropathy
In the management and treatment of axial spondyloarthropathy(SpA), of great importance is the benefit of early detection before the structural damage begins. However, clinical findings of early axial SpA are not specific and assessment can be challenging. Furthermore, current imaging modalities such as radiographs, CT, and bone scintigraphy have shown limitations for use in early detection of axial SpA. Both CT and bone scintigraphy expose the patients to high levels of ionizing radiation; bone scintigraphy showed low specificity and CT cannot detect until structural bone changes have progressed. On the contrary, MRI has shown high sensitivity and specificity to evaluate prestructural early inflammatory changes, specifically in observation of bone marrow edema adjacent to joints and discs, entheses, and ligaments.
Although MRI of the sacroiliac (SI) joints has traditionally been used in suspected axial SpA, this localized technique may be inadequate. Inflammatory lesions in the spine have been found most commonly in the thoracic spine in addition to the SI joints. Full-length spine MRI can reveal the involvement of the thoracic spine, with emphasis on the most lateral sagittal aspects of vertebral endplates and costovertebral junctions. About 23% of the ankylosing spondylitis patients with the clinically active disease only have inflammatory spinal lesions and no evidence of active inflammatory sacroiliitis, even in very early disease. Cervical spine involvement is also common in ankylosing spondylitis. For these reasons, full-length spine MRI of the whole spine including SI joints is an essential tool in the diagnosis, management, and prognosis of axial SpA.
Full-length spine MRI has been integrated into recommendations for the staging and therapeutic response evaluation in ankylosing spondylitis. It has been used to evaluate the therapeutic response showing the transition from active enthesitis with bone marrow edema to quiescent fatty infiltration of the bone marrow.
Spinal Metastasis
Plain radiography, CT, and MRI comprise the core imaging modalities for patients with vertebral metastases. The CT provides cross-sectional images, allows for entire spine imaging, visualization of cortical and trabecular bone, and is more sensitive than conventional radiography. CT scans can detect a bony metastatic lesion up to 6 months earlier than a plain radiograph. However, when compared to MRI, Buhmann et al. found the diagnostic accuracy of MRI (98.7%) to be significantly superior to MDCT (88.8%) for the detection of osseous metastases. Sensitivity was significantly lower for MDCT (66.2%) than for MRI (98.5%). Moreover, cortical destruction may be difficult to assess on CT when osteoporosis or degenerative changes are present. There is also an inherent associated risk of radiation exposure. Changes in the bone marrow are fundamental to the sensitivity of MRI in the detection of skeletal metastases to the spine. The combination of unenhanced T1-weighted spin echo and STIR sequences has shown to be the most useful for the detection of bone marrow abnormalities and is able to discriminate benign from malignant bone marrow changes.
Therefore, contrast-enhanced MRI of the entire spinal axis is the current standard for the diagnosis and evaluation of spinal column metastases. If the MRI examination is limited to the spine region of interest, and bone marrow metastases outside the image, other areas of spinal disease can be missed. Full-length spine MRI is often imperative to visualize multiple levels of spinal involvement with asymptomatic disease or the large amount of bone destruction on plain radiography. Full-length spine MRI including pelvis has been used to detect bone metastases and hematologic malignancies. In prostate cancer, full-length spine MRI including the pelvis is highly sensitive for the detection of metastases in the axial skeleton ( Fig. 4 ). In multiple myeloma, the axial skeleton approach with entire spine and pelvis is recommended in the staging system.