Introduction
The evaluation of spinal pathologies is dependent upon careful history, clinical examination, and appropriate full-length spine radiographs. Appropriate full-length spine radiographs should be obtained when evaluating a patient for suspected coronal, sagittal, or combined imbalance. Full-length spine should ideally include C7 and both femoral heads. This ensures that important landmarks used for parameter calculations are readily available. Plain radiographs can be obtained either through a standardized method using long-film acquisitions with a radiographic source located 72 inches away from the subject or, more recently, through the use of an EOS™ system. The EOS™ system is a slot-scanning device that allows simultaneous acquisition of full-length spine radiographs both in the PA (or AP) and in the lateral position with a significant dose reduction when compared with traditional digital radiography acquisitions.
The thoracic spine is typically composed of 12 thoracic vertebrae each bearing a pair of ribs. The lumbar spine is typically composed of 5 lumbar vertebrae. Normal variations include 11 or 13 thoracic vertebrae and 4 or 6 lumbar vertebrae, and can be seen in as much as 10% of the population. The spine is normally straight in the coronal plane with an accepted variation up to 10° before being considered a scoliosis. In the sagittal plane, the thoracic spine is normally in kyphosis (normal range 20–50°) and the lumbar spine is in lordosis. Lumbar lordosis is usually well correlated with pelvic incidence.
Radiographic imaging of the spine is a static representation of the patient’s everyday posture. It doesn’t take into consideration gait compensatory mechanisms or one’s functional limitations such as spasticity or limited range of motion. A careful evaluation of the patient’s gait is of critical importance to better understand the subtle variations in the patient’s sagittal and coronal profiles. Postural control is also highly dependent on integration at the central nervous system level of external stimuli, including proprioception, vestibular information, and visual information. This information is processed centrally, and posture derives from this complex and intricate process. Horizontal gaze (vision) is a central part of posture and plays an important role in the patient’s ability to stand with a normal posture. The other determinant of sagittal alignment is pelvic morphology, which dictates how the lumbar spine and, to some extent, how the thoracic spine will be aligned.
Image Acquisition
Radiographs should be acquired with the patient standing in a natural physiological load-bearing position. Hips and knees should be in their natural position for the patient but don’t need to be fully extended. These compensation mechanisms should, however, be noted during physical examination. If possible, head-to-toe image acquisition (as is possible with the EOS™ system) will give an insight into these compensation mechanisms. The arms should be positioned in a way allowing a good assessment of the thoracic spine. Classically, this is done either through a hands-on-clavicle (or hands-on-cheek) position or with the arms holding a support. More recently, a hands-on-wall in the EOS™ system has been advocated with the added benefit of being able to determine the bone age for adolescents. Jackson et al. evaluated the hands-on-clavicle vs. hands resting on a support with their arms at 30° and 45°, and found little difference between these positions. Ideally, to allow for comparison between images taken at different times, there should be some standardization in the position and the acquisition method. The images should span the whole spine from the base of the skull to the pelvis and include both femoral heads. This allows for specific spinal alignment parameters to be determined without repeat imaging.
Radiographic Parameters
Most parameters are either linear measurements or angular measurements. The remainder will involve ratios between angles or a proportion of deformity by level (deformity angular ratio—DAR). These parameters can be useful in understanding a patient’s spinal balance, preoperative assessment of the deformity, and operative planning. Postoperatively, these parameters can also be used to determine sagittal and coronal balance restoration as well as to monitor the long-term adjacent deformity. One should, however, be cautious when using linear measurements as they are highly dependent on calibration. The EOS™ images being acquired in a rigid calibrated environment are more precise and less subject to linear measurement errors.
Coronal Parameters
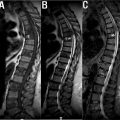
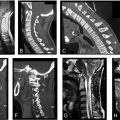
Normal spinal alignment usually refers to a thoracic and lumbar curve devoid of any significant curvature. A deformity is considered significant only when a Cobb angle of more than 10° can be measured on the PA or AP standing radiograph. The Cobb angle measures the maximal curve of a particular region of the spine formed by the most angled superior vertebra and the most angled lower vertebra. Parallel lines to the superior and inferior endplates are used to measure the Cobb angle. Although not always present, a proximal thoracic (PT), main thoracic (MT), and a thoraco-lumbar/lumbar (TL/L) curve can be measured ( Fig. 1 ). The upper-end vertebra (UEV) and the lower-end vertebra (LEV) are the proximal and distal vertebra composing a structural curve. The center sacral vertical line (CSVL) is a vertical line drawn from the center of S1. It helps in determining the position of the different components of the curve relative to the coronal mid-axis. The neutral vertebra is usually the vertebra that appears to have the least rotation on a coronal radiograph distal to the main structural curve. The stable vertebra (SV) is usually the most cephalad vertebra directly distal to the major curve that is most closely bisected by the CSVL ( Fig. 2 ).


The sagittal balance (C7-plumbline) can be drawn in the both PA and lateral radiographs. In the coronal and the sagittal plane, it is a vertical line drawn from the center of the C7 vertebral body.
The deformity angular ratio (DAR) is an indirect measure of the severity of a curve as it represents a ratio between the total deformity (maximal Cobb angle) divided by the number of levels comprised in a curve. The DAR can be measured globally, in the coronal plane (C-DAR) or in the sagittal plane (S-DAR). It gives a better perspective of the severity of a specific curve with higher DAR being more angular. The DAR may affect the surgical plan ( Fig. 3 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree