Key points
- •
Fungal sinusitis is classified into invasive and noninvasive forms based on histopathologic evidence of tissue invasion by fungi.
- •
The invasive category includes acute invasive, chronic invasive, and granulomatous forms.
- •
The noninvasive category includes allergic fungal sinusitis and mycetoma.
- •
Each of the subtypes of fungal sinusitis has a different clinical presentation, distinct from the other forms, is associated with unique radiologic features, and a specific treatment plan.
Introduction
Among causes of sinonasal inflammatory disease, fungal sinusitis is a relatively uncommon but well-established clinical entity. Fungi are ubiquitous in the environment, and can colonize the upper respiratory tract mucosa when fungal spores are inhaled. In people with normal immune function, the fungal growth is kept in check. With impaired host immunity, fungi can invade host mucosa and cause invasive disease. Clinicians should therefore maintain a high index of suspicion of fungal sinusitis in immunocompromised patients with sinusitis, and those with chronic sinusitis. Fungal sinusitis consists of a heterogeneous group of disorders, with diversity in the affected patient population, offending agents, mechanism of disease, clinical presentation, histopathology, imaging appearances, treatment, and overall prognosis.
Fungal sinusitis is broadly classified into two major groups: invasive and noninvasive forms. Although fungal sinusitis can be caused by any fungus, most result from Aspergillus infection. The invasive form is distinguished from the noninvasive variety depending on the presence of fungal elements outside the paranasal sinuses. It should be noted that although the distinction between invasive and noninvasive forms is suggested based on the clinical presentation, imaging evidence and/or histopathologic confirmation is required. Patients with noninvasive form typically present with chronic sinusitis that fails to respond to repeated courses of antibiotics and surgeries. Invasive fungal sinusitis usually occurs with an acute onset characterized by fever, cough, and occasionally nasal mucosal ulceration. Usually this invasive form is seen in immunocompromised patients. There are chronic forms of invasive disease that can have an innocuous presentation, but usually demonstrate progressive worsening of symptoms suggestive of involvement of adjacent structures, such as associated visual disturbance suggesting orbital invasion.
This article first explains the classification of fungal sinusitis, and then evaluates separately the different entities with a particular focus on the radiologic appearance, and the information that the clinician needs to know to institute an appropriate therapy.
Introduction
Among causes of sinonasal inflammatory disease, fungal sinusitis is a relatively uncommon but well-established clinical entity. Fungi are ubiquitous in the environment, and can colonize the upper respiratory tract mucosa when fungal spores are inhaled. In people with normal immune function, the fungal growth is kept in check. With impaired host immunity, fungi can invade host mucosa and cause invasive disease. Clinicians should therefore maintain a high index of suspicion of fungal sinusitis in immunocompromised patients with sinusitis, and those with chronic sinusitis. Fungal sinusitis consists of a heterogeneous group of disorders, with diversity in the affected patient population, offending agents, mechanism of disease, clinical presentation, histopathology, imaging appearances, treatment, and overall prognosis.
Fungal sinusitis is broadly classified into two major groups: invasive and noninvasive forms. Although fungal sinusitis can be caused by any fungus, most result from Aspergillus infection. The invasive form is distinguished from the noninvasive variety depending on the presence of fungal elements outside the paranasal sinuses. It should be noted that although the distinction between invasive and noninvasive forms is suggested based on the clinical presentation, imaging evidence and/or histopathologic confirmation is required. Patients with noninvasive form typically present with chronic sinusitis that fails to respond to repeated courses of antibiotics and surgeries. Invasive fungal sinusitis usually occurs with an acute onset characterized by fever, cough, and occasionally nasal mucosal ulceration. Usually this invasive form is seen in immunocompromised patients. There are chronic forms of invasive disease that can have an innocuous presentation, but usually demonstrate progressive worsening of symptoms suggestive of involvement of adjacent structures, such as associated visual disturbance suggesting orbital invasion.
This article first explains the classification of fungal sinusitis, and then evaluates separately the different entities with a particular focus on the radiologic appearance, and the information that the clinician needs to know to institute an appropriate therapy.
Classification of fungal sinusitis
The first attempt to classify fungal sinusitis was made in 1965, when two subtypes were recognized: a noninvasive form, clinically similar to chronic bacterial sinusitis; and an invasive form, where the infection mimicked a disease similar to a tumor with bone erosion with invasion into adjacent tissues. The most commonly accepted classification system, based on International Society for Human and Animal Mycology Group, February 2008, categorizes fungal sinusitis into invasive and noninvasive types based on histopathologic evidence of tissue invasion by fungi. The noninvasive subtypes include allergic fungal sinusitis (AFS) and mycetoma; the invasive subtypes include acute invasive fungal sinusitis, chronic invasive fungal sinusitis, and granulomatous invasive fungal sinusitis.
General imaging considerations
There are certain characteristic computed tomography (CT) and MR imaging findings that are highly suggestive of fungal sinusitis. Imaging overall therefore plays a key role in evaluating patients with suspected fungal sinusitis. Noncontrast CT remains the initial imaging study of choice in the work-up of fungal sinusitis. In cases of complicated especially invasive fungal sinusitis, MR imaging can be performed for a more definitive evaluation. CT in general is better in assessing for hyperattenuation within the opacified sinus, which in an appropriate clinical setting can suggest fungal infection. MR imaging is better at evaluating disease extension into adjacent soft tissues, including soft tissues of the neck, such as pterygomaxillary fissure, orbit, intracranial compartment, and vasculature.
On CT, inflammatory watery secretions are seen as low-attenuation. As the inflammatory sinus disease persists, the secretions become inspissated and demonstrate a higher attenuation than muscle. In cases of fungal sinusitis, calcium and magnesium salts become deposited in areas of fungus growth and fungus-infected mucin. These fungal concretions appear hyperdense on noncontrast CT.
MR imaging appearance of secretions depends on their protein content, viscosity, and presence of calcifications. Watery secretions usually contain less than 5% protein content; they appear as low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. As they become inspissated, the secretions contain higher percentage of protein content (between 5% and 25%). Increasing T1 signal intensity is noted on T1-weighted images and a variable signal is seen on T2-weighted images. Within sludge or mycetoma where protein content can be between 25% and 40%, low signal intensity on T1-weighted images, and low signal or signal void on T2-weighted images are seen. This last pattern has been described to be highly suggestive of fungal sinusitis.
Noninvasive fungal sinusitis
Allergic Fungal Sinusitis
AFS is the most common form of fungal sinusitis, and is common in humid climates. The overall incidence of AFS is estimated at 5% to 10% of all hypertrophic sinus disease cases going to surgery. It was first reported as allergic aspergillosis by Millar and colleagues in 1981 who noted the similarity of the fungal-containing sinus exudate characteristic of this condition to the one found in the bronchi of patients affected by allergic bronchopulmonary aspergillosis.
AFS refers to noninvasive collection of impacted mucus and cellular debris, resulting from an allergic response to fungal colonization within the sinus cavity. It should be noted that the amount of fungal elements within the opacified sinus is variable, often times scanty. The secondary inflammatory process that results does not depend on the quantity of fungus present. Hence, the role of fungi in initiating or promoting this disease is controversial and by some, thought to be circumstantial.
The typical patient with AFS is young, atopic, immunocompetent, and presents clinically with hypertrophic sinus disease experiencing chronic headaches, nasal congestion, and chronic sinusitis for several years. Fungal-specific IgE as detected by type I hypersensitivity skin testing is a constant feature. Total serum IgE is elevated, up to 5000 IU/mL, with a mean of 600 IU/mL commonly seen. Originally considered to be caused solely by Aspergillus species, other causative fungi commonly reported include dematiaceous fungi, such as Bipolaris , Curvularia , Alternaria , and Fusarium .
Within affected sinuses, “allergic mucin” is found, characterized by a purulent, yellow-green and sometimes black mucus, which at histopathologic analysis reveals the presence of eosinophil granulocytes and Charcot-Leyden crystals, which are eosinophil degradation products. Fungal hyphae are sparse and noninvasive, and may be identifiable by special stains, such as Gomori methenamine silver stain. Given the specific histopathologic findings, the presence of allergic mucin is virtually diagnostic for AFS, sometimes even in the absence of fungal identification.
Imaging features
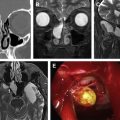
On imaging, there is unilateral or asymmetric involvement of the sinuses. Characteristically, multiple sinuses are involved. Maxillary and ethmoid sinuses are most commonly involved. Noncontract CT shows hyperdense areas within the sinus cavities outlined by hypodense-appearing thickened and inflamed mucosa ( Fig. 1 ). Depending on the contents of the material, the MR imaging signal is variable, ranging from isointense to hypointense signal to signal void on T1- and T2-weighted images. This signal heterogeneity is related to the presence of deposited heavy metals, such as iron and manganese. On contrast-enhanced studies, the intrasinus contents usually demonstrate no masslike enhancement. Because of the expansive nature of allergic mucin, and its propensity to incite local inflammatory response, sinus expansion along with osseous remodeling and erosive changes of the sinus walls are seen.
Treatment
Endoscopic removal of polyps and inflammatory material, including mucin, to re-establish aeration and drainage of involved sinuses is essential for successful treatment. Following surgery, additional measures including the use of topical steroids for immune response suppression is important to prevent recurrences; this concept was actually derived from experience with allergic bronchopulmonary aspergillosis. Other therapies, such as immunotherapy, antihistamines, oral antileukotrienes, oral steroids, and nasal irrigation, are helpful in certain clinical situations.
Fungus Ball
Fungus ball, also referred to as a fungal mycetoma or aspergilloma, is reported as a distinct clinical entity and a discrete form of noninvasive fungal sinus disease. It refers to an indolent growth of fungal hyphae in a sinus cavity until a masslike lesion is formed. Affected patients are immunocompetent, nonatopic, and otherwise healthy. Some studies have reported the disease to be more common in older women. However, patients of all ages are affected. The maxillary sinus by far is the most common site of occurrence. It has been postulated that the host’s deficient mucociliary clearance mechanism is accountable for the disease. This allows the uncleared fungal elements to colonize and proliferate in the retained secretions within the sinonasal cavity, inciting an inflammatory response. Previous endodontic treatment and radiotherapy are sometimes implicated in the development of a mycetoma. Aspergillus fumigatus is the most commonly implicated pathogen.
Clinical diagnosis
Typically, medical attention is sought for mild sinus pressure. In some cases, patients are asymptomatic and the diagnosis is made incidentally on imaging. A surgical specimen of a fungal mycetoma has been described as a thick, semisolid mass with “claylike” consistency. Histopathologic examination reveals tightly packed fungal hyphae without allergic mucin, a feature distinct from AFS. Calcium oxalate deposition often accompanies the growth of Aspergillus , and appears as radiating clusters of birefringent crystals on histochemistry.
Imaging features
Characteristic imaging findings are critical to the diagnosis. Typically, a single sinus cavity is affected, a distinct feature from other forms of fungal sinusitis. Maxillary sinuses are most commonly affected, followed by sphenoid, frontal, and ethmoid sinuses. Another unique feature is the lack of sinus expansion. Because of its chronic nature, osseous remodeling of the sinus wall can be seen, noted as thickening and sclerosis. There is opacification of the involved sinus with central areas of high density and fine, round-to-linear matrix calcifications ( Fig. 2 ). T1-weighted images demonstrate low signal intensity of the thick, solid, mycetomatous mass, although the signal can be heterogeneous depending on the content. Because of the presence of calcifications and paramagnetic metals, such as magnesium, iron, and manganese, low T2 signal intensity is also observed. Contrast-enhanced studies demonstrate thickening and enhancement of the surrounding inflamed mucosa. There is no involvement of the soft tissues surrounding the involved sinus cavity.