Introduction
Imaging methods of the spine have greatly expanded since the advent of X-rays for the use of plain radiographs (c.1895), providing anatomical clarity for diagnosis and treatment of the cervical, thoracic, lumbar, and sacral vertebrae. The complex anatomy of the vertebrae and irregular contours and geometry of the spinal elements have influenced the rapid development of more precise imaging modalities. Various advancements to two- and three-dimensional (i.e., 2D, 3D, respectively) imaging through plain radiographs, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and EOS imaging along with multiple dimensional views of the spine are continuously optimized. Future developments in imaging may improve the assessment of pedicle screw placement and image definition, reduce radiation, provide quantitative information about disc and other soft tissue composition, and provide autonomous spinal mapping using artificial intelligence (AI).
Future of Plain Radiographs
Plain radiographs utilize a heterogeneous emission of X-rays projected in the direction of a detector, ultimately curating an image established through components of the intervening objects, including composition as well as density. Plain radiographs may see improvements by providing image intensification, digital detectors, and radiosensitive screen amplifications. Although plain radiographs demonstrate a substantial degree of reliability, computed tomography (CT) has become the primary choice in imaging spinal injuries while obtaining similar measurements to plain radiographs. Many may transpose their diagnostic care toward CT imaging over plain radiographs. Computed tomography utilizes a computerized X-ray imaging method in which a beam of X-rays is directed at the patient and rapidly circumvolved around the patient to develop cross-sectional images of the patient’s body. Plain radiographs are increasingly replaced by contemporary imaging methods, including, but not limited to, intraoperative CT (ICT), 3D imaging, and the newfound application of AI and augmented reality (AR). Several reasons exist for the gradual phasing out of plain radiographs. Foremost are the limitations on types of features visible in the image. Such limitations are evident when soft tissue, high image resolution, and 3D characteristics are desired. For example, identification of bone loss on plain radiographs is typically not appreciable until over 30%–40% loss has occurred. Furthermore, these limitations persist when detecting pedicle screws with a “safe” misguided freehand placement. Instead, CT technology boasts a higher accuracy and, therefore, a better-suited imaging technique for the confirmation of suspected incorrect screw positioning. Plain radiographs have also proven inadequate in terms of cervical spine assessment following blunt trauma due to poor visibility of the entire cervical spine. An accompanying CT scan is often required to assay the cervical spine accurately, eliminating the need for a plain radiograph. These circumstances have indicated the urgency to adopt alternative and more modern methods in spinal imaging.
Future of Computed Tomography
The use of CT imaging in the United States has significantly increased in the past two decades, although its growth has slowed in recent years. Additionally, pediatric CT usage has seen a significant decrease due to concerns for excessive radiation exposure. The increase in adult CT usage has brought about concerns about the health risks associated with radiation exposure. Regardless, CT remains an often-used tool for adult patients to obtain detailed images of the spine and, in some cases, even offers reduced radiation doses compared to some standard techniques.
Fluoroscopy and CT are standard techniques for surgical navigation. Computed tomography has been shown to expose physicians to less radiation than fluoroscopy; however, radiation exposure for patients was higher. Intraoperative CT systems have improved accuracy and success in spine surgery. Comparative studies with fluoroscopic-based techniques have repeatedly found intraoperative CT imaging to have superior accuracy and less radiation exposure for the surgeon. Additionally, modifications to amperage, scan, and scout length radiation exposure for patients can also be reduced compared to standard CT imaging. However, a novel technique using a detachable pedicle marker and probe combined with pulsed fluoroscopy has been shown to considerably reduce radiation exposure for both patients and physicians while maintaining comparable accuracy to standard fluoroscopy and intraoperative CT imaging.
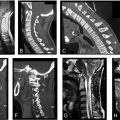
Co-registration or image fusion of CT images with preoperative MRI can enhance navigation for spinal procedures. A problem with attempting to fuse MRI with CT arises from patient positioning changing between the different imaging procedures. The study by Hille et al. utilized a multisegmented approach for image registration to account for this issue. The fusion of MRI with CT using this multisegmented approach may provide the greatest benefit to spinal metastases being targeted by radiofrequency ablations. The multisegmented approach takes significantly less time for registration compared to the landmark-based directive (an average of 24 s per vertebra vs an average of 8 min per vertebra), illustrating that this technique can be integrated practically into the clinical workflow.
A case study of two patients analyzed the usage of co-registered intraoperative CT and MRI for the resection of intradural spinal tumors. For one of the patients, additional preoperative diffusion tensor imaging (DTI) was also co-registered with the other imaging modalities. In each case, the co-registration of intraoperative CT with MRI and DTI enhanced navigation during tumor removal. The study reported that the addition of DTI with intraoperative CT helped with the localization of the tumor and allowed for about 90% removal, which would have been unlikely without the co-registration of DTI.
Machine learning applications for spinal imaging are continually evolving. A team of medical researchers at Pusan National University Hospital in Busan, Korea, developed a machine learning model to predict osteoporosis from Hounsfield units of lumbar CT images. Machine learning models for the identification and classification of vertebral fractures from CT images have also been developed. Deep learning has also been utilized for the automatic segmentation of lumbosacral nerves from CT images to aid in the 3D reconstruction of targeted areas for the viability assessment of transforaminal steroid injection. Compared to manual segmentation, the deep learning model saves considerable time. There are additional models being developed. Machine learning for spinal imaging will be an area of rapid growth in the upcoming years.
Future of Magnetic Resonance Imaging
Magnetic resonance imaging provides high-resolution multiplanar images of vertebral and soft tissue anatomy without posing any risks associated with radiation exposure, proving to be the diagnostic procedure of choice for most spinal pathologies. This imaging modality offers relatively high sensitivity and specificity for the assessment of infections, tumors, disc degeneration, pathologic fractures, and disc herniations. However, MRI is relatively expensive and has a variable degree of utility in obese, claustrophobic, and pacemaker-dependent patients.
Sodium, T1-rho, UTE, and gagCEST MRI
Standard proton MRI lacks the ability to provide direct markers for tissue viability. Sodium MRI takes advantage of sodium-potassium pumps and other biochemical mechanisms maintaining transmembrane sodium gradients by quantifying intracellular and extracellular sodium levels to better identify tissue viability. However, the detection of sodium signals is challenging and requires high field strengths to obtain images of the same resolution as standard MRI. Due to the many constraints, sodium MRI is considered clinically infeasible for routine use. However, many methodological advances are beginning to bring sodium MRI to a level where it can be used in practical clinical settings.
To address the limited signal intensities in cortical bone, ultrashort echo time (UTE) sequences were developed to elicit hyperintense signals of cartilage (e.g., the cartilaginous endplate) and osseous structures. Other methodologies have also used echo time with varying degrees of success. These include short tau inversion recovery protocols, allowing the suppression of adipose tissue.
Magnetic resonance imaging techniques are continuously being developed, involving additional applications that manipulate magnetic field directionality. For example, T1-rho MRI is a technique developed for use in cartilage imaging and takes advantage of directionality manipulation, but has been utilized readily to detect proteoglycan content of the disc to facilitate early identification of degenerative disc changes. With a similar line of thinking in assessing early-stage disc degeneration, Kim et al. aimed to assess the feasibility of quantifying glycosaminoglycan chemical exchange saturation transfer (gagCEST) values in human intervertebral discs using a 3T MRI scanner. The study proved that in in vivo gagCEST, quantification in human lumbar intervertebral discs is feasible at 3T in combination with successful B 0 inhomogeneity correction without significant hardware modifications. However, the clinical applications, in particular in the context of spine surgery, of gagCEST, along with T1-rho MRI are constantly being evaluated and validation on a large scale is needed.
The proliferation of MRI innovations has proven instrumental in the field of spine surgery, allowing increased diagnostic yields for various pathologies. Several studies have demonstrated that quantitative MRI can differentiate between signals in herniated discs and annular tears when compared with discs lacking gross abnormalities. Similarly, Li et al. demonstrated the potential of sodium MRI in identifying the structure of the knee and its association with cartilage degeneration. Such techniques may be applied to the intervertebral discs and their association with low back pain. More recently, evidence surrounding other sequences has gained additional clinical utility. For example, UTE MRI has led to the description by Pang et al. of the “UTE Disc Sign,” a finding represented by a hyperintense or hypointense band across a degenerative disc associated with chronic low back pain and disability. These findings not only highlight the utility of these added sequences but also suggest MRI’s potential to contribute to refined phenotyping of patients, identifying the pain generating source and potentially predicting outcomes after spine surgery.
Synthetic MRI
Synthetic magnetic resonance imaging (MRI) provides an alternative advantage by producing multiple synthetic contrasts from a single sequence. This technique has been mainly used for brain diseases; however, a recent study evaluated its feasibility in spinal imaging. According to Vargas et al., synthetic images of acceptable quality were acquired in 53% less time than those of conventional MRI. Essentially, this decrease in diagnostic time is crucial in retrieving quantitative measurements of the spine much more quickly than current methods. Historically, the spinal cord has presented challenges for MR imaging due to the various differentiated tissue types characterizing spinal fluid, bone, and air. This renders conventional MRI techniques occasionally unable to differentiate between the spinal cord and other tissues accurately. To address this issue, a study by Tsagkas et al. utilized an averaged magnetization inversion recovery acquisitions (AMIRA) sequence to segment the spinal cord from gray matter and white matter. The group found the AMIRA sequence to be a more time-efficient, accurate, and reproducible MR imaging approach within the spinal cord. In a separate article, the group focused on the automatic detection of lumbar vertebrae in MRI imaging. A novel detection algorithm based on deep learning was utilized to produce an accuracy of 98.6% and a precision of 98.9% in detecting vertebras. These results indicated that a lumbar detection network supported by deep learning can be trained to detect its target without annotated MRI images successfully. This can help increase the degree of clinical efficiency when evaluating spinal MRIs.
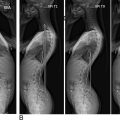
Future of EOS Biplanar X-Ray
The EOS imaging system operates by performing two simultaneous X-rays of the patient from the anteroposterior and lateral views. These 2D images are utilized to reconstruct a 3D model of the spine. Another significant benefit is the reduced radiation dose compared to traditional X-rays and other imaging methods. These benefits make EOS imaging an enticing alternative to other 3D imaging methods. However, since the 3D image is a reconstruction produced from X-rays, the 3D reconstruction does not provide information on soft tissues. Additionally, the 3D model requires manual reconstruction by a radiologist.
EOS boasts high interobserver reproducibility and intraobserver repeatability in its applications for scoliosis and sagittal balance. These involve measurements from the 2D X-rays as well as the 3D reconstruction of the spine. The reproducibility and repeatability of apical vertebral orientation measurements from the EOS 3D spine reconstruction and 3D CT scans showed no statistically significant difference. However, it is essential to note that patient positioning can affect EOS measurements as the apparatus requires patients to be standing upright and facing a particular direction. The patient can be improperly positioned up to ± 10 degrees and still result in acceptable images.
EOS has also been shown to be more accurate for vertebral osteoporosis than dual-energy X-ray absorptiometry. For axial spondyloarthritis, EOS was comparable to conventional radiography. However, the EOS imaging system was not an excellent alternative to MRI for analyzing disc degeneration and other soft tissues. As expected, MRI had greater image visibility and better detection of soft tissue pathology.
X-ray and CT angiography are both typically utilized to garner bone information; however, each comes with its limitations. X-ray provides only 2D images, while CT risks a significant radiation dose. As an alternative, the EOS system provides a method to produce 3D models of the spine with low radiation exposure. As previously mentioned, the 3D image must be manually reconstructed. This requires the radiologist to manually mark the vertebral bodies’ positions, which can take more than an hour, limiting the number of patients that can be imaged daily. This limitation can be overcome using convolution neural networks. By applying a convolution neural network to the acquired X-rays, the 3D reconstruction can be automated and performed much more quickly, allowing for more patients to be imaged each day.
Future of Ultrasound Imaging
Ultrasound imaging employs high-frequency sound waves to image internal organs. Ultrasound can be noninvasive by operating the transducer on the skin. In other cases, invasive ultrasound, such as endoscopic or transvaginal ultrasound, can be performed to obtain better images of the organs of interest. Compared to other imaging modalities, the risk posed to patients by ultrasound is low since it has no ionizing radiation. The few risks involve heating of tissue and cavitation. Due to this overall low risk, ultrasound is an attractive technology to aid in surgical and diagnostic applications for spinal diseases.
Anesthetic Application
Neuraxial anesthesia is widely applied as a means of pain control for surgical procedures as well as labor. Neuraxial anesthesia is typically applied using palpation and surface landmarks as guidance for needle injection. This tends to be a complicated procedure, especially in cases of obesity or prior spinal injury. Errors in injection anesthesia can lead to complications, including permanent neurological damage. Preoperative and intraoperative use of ultrasound can guide the injection, thus reducing these risks. Intraoperative use is even more challenging, requiring the anesthetist to handle the transducer and needle simultaneously. Due to these barriers, the adoption of ultrasound-guided neuraxial anesthesia has been limited.
One novel approach is to use software that automatically marks spinal landmarks as the ultrasound is being performed and then utilizes the marks to triangulate the site and trajectory of the injection. This approach had an excellent first-attempt success rate for neuraxial anesthesia compared to the traditional palpation-based method. Real-time ultrasound guidance can be of better advice as the anesthetist can directly observe the needle during injection. A preliminary study using a paramedian transverse approach with real-time ultrasound guidance found a high first-attempt success rate. There is yet another approach to identify the injection site using machine learning automatically. A support vector machine model was built and trained to identify the injection site based on the classification of the bone/interspinous region.
Intraoperative Ultrasound
Intraoperative ultrasound (IoUS) in spinal surgery has a long history dating back to 1951. However, ultrasound did not immediately become widely used for spinal procedures. It was not until the 1980s, where many applications of IoUS for spinal surgery were reported. In the present, IoUS for spinal surgery enjoys significant usage across many spinal pathologies.
Pedicle screws for the lumbar spine’s stability during fusion or other spinal procedures are generally considered a safe procedure. Still, there remains a risk of screws being malpositioned (with rates reported to be around 10%–15%), leading to potential neurovascular complications and the need for surgical revision. A study analyzed the use of intraosseous ultrasound to determine accurate pedicle screw placement. The ultrasound technique was compared to postoperative CT scanning. The correct interpretation of the ultrasound images by three investigators occurred in 99% of cases with no false negatives. Additionally, one investigator had no prior experience in interpreting intraosseous ultrasound images, thus showing that this technique can be adopted with a low learning curve.
IoUS can aid in visualization during spinal surgery, reducing complications and injuries, and improving success rates. IoUS can be used to observe lumbar spinal surgery, blood vessels and other organs on the approach path and can confirm if they have been adequately displaced. The study performed by Nojiri et al. was able to visualize the organs for all the patients with no organ injury or massive bleeding. Overall, the research shows the utility of IoUS for real-time visualization of blood vessels and organs during surgery, which can help prevent serious injury.
In another case involving the surgery of intradural spinal tumors, IoUS was used to visualize the tumors. IoUS helped determine if laminectomy was sufficient, needed extension, and learning the best myelotomy to be performed. Lastly, IoUS was then used to determine if the total excision of the tumor was achieved. In 7 patients out of 69, laminectomies needed to be extended, and in only 1 case, subtotal excision was observed and needed additional resection. Thus, IoUS can be of great use to determine the extent of excision and incisions required. Furthermore, it can be used to ascertain the success of the surgery and, in cases of incomplete success, lead to an immediate remedy.
Diagnostic Application
The use of ultrasound for diagnostic purposes cannot be understated. Frequent diagnostic imaging can expose patients and physicians to harmful radiation from X-ray. Ultrasound is an imaging modality without ionizing radiation and would thus eliminate this risk if it could be adequately substituted for select diagnostic procedures. Additionally, ultrasound is more accessible to populations in remote or low socioeconomic regions.
Scoliosis evaluation involves the measurement of the Cobb angle obtained from radiographs. This diagnostic evaluation is considered the gold standard but comes with the risks of high exposure to radiation. Several other imaging modalities have been proposed to reduce radiation exposure, but these methods do not eliminate exposure or provide the same level of visualization.
Three-dimensional ultrasound provides an avenue to remove ionizing radiation with excellent visualization altogether. One such ultrasound system developed for scoliosis assessment, Scolioscan, was studied for its reliability and validity for identifying adolescent idiopathic scoliosis. A similar study also analyzed Scolioscan for the best ultrasound angle between the use of the spinous processes and the transverse processes as landmarks for consistent and accurate measurement curve severity. In both studies, Scolioscan was compared to the traditional Cobb angle measurement using radiographs. Both studies observed high reliability as well as an excellent correlation of the ultrasound angles with the Cobb angles. The latter study also found no significant difference in the reliability of validity between the ultrasound angles. Ultimately, this demonstrates the use of ultrasound as a diagnostic modality that can reduce patient exposure to radiation.
The diagnostic use of ultrasound can also aid in treatment procedures. The magnetically controlled growing rod (MCGR) system was developed to treat early-onset scoliosis, compared to a traditional growing rod system where the rod needs to be lengthened periodically via invasive surgery. Alternatively, MCGR requires no surgery and rod lengthening can be performed more frequently. However, this also results in increased amounts of radiation as the spine would need to be imaged by radiography before and after lengthening. To combat this limitation, ultrasound has been employed to assist in rod lengthening with the use of plain radiographs. A prospective study imaged patients using ultrasound to find and lengthen the rods. The new procedure was found to be comfortable and practical to implement. Due to the limitations of ultrasound imaging itself, neither the assessment of complications in the implants themselves nor the assessment of fusion blocks at the proximal and distal fixation points is possible. Hence, periodic radiographs are still required. However, with this method, the number of radiographs can be reduced while allowing frequent lengthening, thereby reducing the risk of complications from radiation, in particular in the young where radiation-induced bone and soft tissue sarcomas may occur.
Decreasing radiation exposure
Radiation is known as the emission of energy and can be either electromagnetic or particulate. Electromagnetic radiation utilizes photons that consist of energy, but without mass or charge. Conversely, particulate radiation contains particles that have mass and energy, but not necessarily an electric charge. Concerns regarding radiation have been well documented and noted previously above. Unfortunately, surgeons and surgical staff must endure the potential for radiation exposure during minimally invasive spine surgeries due to the heightened necessity for intraoperative imaging in these procedures. As concerns over physician and patient radiation exposure increase (due to a rise in minimally invasive spine surgeries requiring such techniques ), the importance of decreasing radiation has been prioritized. This goal has been deemed feasible in particular spine-related surgical procedures, resulting in reduced radiation exposure to patients and no adverse postoperative effects. As the focus toward successful surgeries with reduced radiation becomes increasingly prevalent, numerous methods emerge to assist in making it a reality, including ultra-low-radiation imaging (ULRI) with image enhancement. ULRI is a technique that is just as it sounds, an imaging source that emits radiation but in minimal doses. Image enhancement refers to the process of altering digital images to make results sufficient for proper analysis. ULRI coordinated with image enhancement allows for substantial radiation reduction in minimally invasive procedures while maintaining adequate visualization during surgery and remaining in accordance with procedure safety. Image enhancement software, such as NuVasive’s LessRay , allows surgeons to scale down their dependence on radiation-inducing imaging during procedures. The concept of image enhancement software utilizes full-dose preoperative fluoroscopic images as a reference to form a conglomerated image of the necessary spinal levels, ultimately reducing radiation emissions by approximately 75%. Parallel to ULRI with image enhancement, computer-assisted image-guided spinal navigation (such as ICT) also paves the way for diminished radiation exposure to surgeons. An ICT scanner allows surgeons to utilize the benefits of CT scans during procedures, enabling surgeons to sync preexisting scans with current ones. Ultimately, this supports surgeons in efficiently executing critical decisions in the operating room. The use of ICT in alliance with spinal navigation yields results similar to using traditional fluoroscopy with the supplemental contribution of reduced radiation. Additionally, the utilization of ICT reduces radiation exposure in patients. This is in addition to the benefits of enhanced patient safety from the reduced rate of screw positioning.
Alongside ICT and ULRI with enhanced imaging, the use of pulsed fluoroscopy (PF) paired with detachable pedicle marker and probe (DPMP) has emerged as a technique to decrease radiation. Pulsed fluoroscopy is identified as a tool utilizing a combination of pulse frequency and dose to reduce radiation exposure to patients while simultaneously enhancing image quality. Pulsed fluoroscopy and DPMP have allowed for decreased radiation exposure to both the surgical team and patients, all while maintaining accuracy during the procedure. The reduced radiation approach should be the new standard in the future of spine imaging upon the enlightenment of the proficiency and feasibility of reduced radiation in minimally invasive surgeries.
Assessing Intervertebral Disc Metabolism and Transport for Precision Spine Care
The intervertebral disc is the largest avascular structure in the human body, requiring disc cells to be uniquely suited to survival in a harsh environment, including a low nutrient supply of glucose and oxygen and high metabolite concentration of lactic acid, leading to low pH. Despite the suitability of IVD cells for this environment, changes in disc structure and subsequent small changes in nutrient supply can threaten the survival of endogenous IVD cells as well as transplanted cells. As the cells die, due to a mixture of nutrient limitations, biomechanical problems, and signaling cascades, the ability of the disc to remodel its extracellular matrix (ECM) declines and the disc degenerates. All discs undergo some structural changes with age, including reorganization of ECM components and calcification of the disc endplate, an important part of the disc nutrient supply. Capillaries are lost, and contact with the marrow cavities decreases. Additionally, the ECM changes in the annulus fibrosus (AF) and nucleus pulposus (NP) also cause decreased diffusion in those regions. Mature disc cells use glucose and produce lactic acid. Although they do not require much oxygen to live, cell activity and ECM synthesis are reduced at low concentrations.
Fundamental studies of the disc often focus on regenerative medicine. Disc regeneration strategies focus on targeting molecular pathways of ECM degeneration. This could theoretically be accomplished by supplementing anabolic factors (usually by adding cells), increasing production of anabolic factors (by growth factors), or decreasing production of catabolic factors (through growth factor or cytokine therapy). One major challenge to these approaches is their reliance on increasing cell activity or density in a nutrient-starved environment. In order to make these regenerative treatments successful, there will likely need to be an imaging approach to determine the nutrient capacity for each disc being considered for a biological therapy.
There are several imaging methods that are being used to study disc metabolism and transport phenomena. Magnetic resonance imaging can be used to study water diffusion in the disc in vivo using diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) mapping. In a study of 100 patients’ MRIs, ADC maps of NPs in 435 discs showed diffusion coefficients varied by up to 75% among discs with the same Pfirrmann grade. Recently, DTI studies have investigated diffusion in the disc and detected pathological changes at early stages of cartilage degeneration. There have been a few excellent studies that have answered disc transport phenomena-related questions using medical imaging of small-molecule surrogates in the disc.
Ratio of R1р dispersion and -OH chemical exchange saturation transfer (RROC) imaging is sensitive to pH changes in ex vivo porcine discs without being confounded by variation in GAG concentration. Endogenous glucose changes are apparent on T1р-weighted dynamic glucose-enhanced (DGE) MRI. Glucose changes could also theoretically be determined using [ 18 F]2-fluoro-2-deoxy- d -glucose ( 18 F-FGD) positron emission tomography. Finally, magnetic resonance spectroscopy has been demonstrated to quantify metabolites, specifically lactate and proteoglycans, and has been applied to aid surgeons in identifying painful discs for surgical intervention.
Applications of Artificial Intelligence
Artificial intelligence (AI) is an overarching field that contains subjects, such as machine learning (ML) and deep learning (DL). Machine learning is a statistical method that absorbs data and their results to train a computer algorithm, which may later perform predictions on unseen data, while deep learning has a layered structure that creates an artificial neural network. This artificial neural network has autonomy, which allows it to learn the complexity further, performing intelligent decisions on its own. The applications of AI in spinal imaging are continuously studied and endlessly evolving although the full extent of their applications has yet to be applied. It is well known that the potential of AI may allow for enhancements to existing techniques and modalities of spine care. Machine learning and deep learning, in conjunction with current technologies, augment traditional approaches further to enhance the scope of a clinician’s accuracy, further optimizing pre-, post-, and perioperative treatment. The applications of AI present itself through 3D construction of the spine, enhanced image resolution, improvements to perioperative navigation techniques, and postoperative patient satisfaction outcome predictions.
Three-Dimensional Construction of the Spine
Analyzing MRI and CT images, machine learning identifies spinal markers, creating augmented simulations as well as printable structures, which exhibit an enhanced view of the patient’s spine. Three-dimensional rendering of anatomical structures through image stitching software communicates in conjunction with artificial intelligence to outline necessary anatomy. This novel pairing improves upon stand-alone imaging, sharing insight into both visual and physical aspects of the spine. In a study concerning 3D printing in orthopedic case preparation, it was found that the use of the generated anatomical models significantly increased surgical precision while decreasing intraoperative bleeding, surgical time, and, consequently, the amount of anesthesia required. Further, machine learning may serve in concert with augmented reality for minimally invasive surgical navigation systems through 3D modeling in augmented space. In preparation for pedicle screw instrumentation, the augmented reality surgical navigation (ARSN) was anointed as a replacement to the fluoroscopy-guided minimally invasive method. Although it was found that both offered similar navigation efficiency, the ARSN system did not involve radiation. This potential presents surgeons with the opportunity to perform spine-related operations in a protective lead garment-free environment.
Deep Learning for Lesion Detection and Classification
Deep learning is a subset within machine learning that is designed to automatically and adaptively learn the priority features from data through the backward calculation of weights in a layered structure; this process is known as backpropagation. The method commences with the final layer, traversing in reverse until the initial layer. This approach enhances decision making, filtering, and classifying data into cohorts that would allow the algorithm to make intelligent decisions with improved accuracy compared to the manual feature engineering that ML requires. Computer vision algorithms are DL algorithms, which are applied through a convolutional neural network (CNN) to classify images. The CNN does so using the layered DL structure to differentiate characteristics that would distinguish it from other models. It is believed that CNN algorithms may offer enhancements to traditional diagnostic methods of oncological spinal tumors on MRI. In the case where spinal schwannoma and meningioma were identified on T1- and T2-weighted MRI, diagnosis by both radiologists and the CNN was found to have performed at levels comparable to that of experienced radiologists. Consequently, this has opened avenues to further applications within the scope of spinal oncology for optimized assistance in diagnosis and identification of complex anatomical structures, an issue that ML algorithms often failed to address. Further, the CNN algorithm may be implemented to identify relevant spinal anatomy and degenerative conditions.
The Spine Explorer is a deep learning-based software that automates spinal mapping of vertebral bodies and their intervertebral discs for quantification and analysis of the relative cervical, thoracic, and lumbosacral anatomy. The Spine Explorer was designed to identify degenerative spine conditions for improved speed and precision of data collection. In turn, this standardizes methods that may enhance the quality of research concerning degenerative spinal condition while offering additions to the clinician’s armamentarium of diagnostic tools. Much like the case where spinal tumors were differentiated, neural networks may also possess the ability to grade spinal stenosis in patients suffering from pain, numbness, or weakness in the arms or legs. This is possible through the layered structure of the CNN, which maps the spinal canal and cord. Inevitably, deep learning and convoluted neural networks serve to augment the clinician’s intuition and the precision of their diagnosis for optimal patient satisfaction outcomes.
Conclusions
Improved image quality, decreased radiation exposure, faster imaging and analysis, improved reliability, and intraoperative use have been guiding factors in the evolution of spinal imaging. Less reliance on plain radiographs while exploring new technologies, such as ML reconstructions or using standard tools in novel ways, such as intraoperative ultrasound, has decreased radiation risk while improving surgical techniques. Intraoperative CT provides surgeons with great guidance in real time to assist in navigating challenging anatomy. Magnetic resonance imaging has long been an expensive and time-consuming imaging technology. New MRI techniques being developed improve both image acquisition time and diagnostic information that can be obtained. Novel imaging can further assess metabolism and transport of materials into and out of the disc, allowing for refined patient selection/stratification that can also inform dose and approach for regenerative biologics of the disc as well as facilitate precision spine care. Machine learning is at the forefront of impressive automatic classification, reconstruction, and analysis of spinal features. The quick automatic analysis provided by machine learning can intraoperatively assist navigation during surgery. These developments in spinal imaging are reducing intra- and postoperative complications for both patients and physicians, leading to overall superior satisfaction and outcomes, as well as identifying the source of the pain for operative planning, managing patient expectations, and improved patient outcomes. The utility between advances in imaging coupled with the unraveling and implications of AI and ML approaches toward imaging and predictive modeling will continue to expand in the years to come and usher in a new age of precision spine care.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree