There has been much progress in contrast enhanced neuroradiologic magnetic resonance imaging in the almost 25 years since the first gadolinium-based contrast agent was approved in the United States. Much of this now focuses on the introduction of significantly higher relaxivity agents into our clinical armamentarium and the addition of T2*-weighted imaging sequences to hyperacute stroke or neoplastic evaluations. All 4 magnetic resonance contrast agents approved in the United States during the past decade have been higher relaxivity agents, suggesting a strong trend in our industry to continue to find more efficient, more powerful, more diagnostic means of increasing contrast on imaging studies.
- •
Because magnetic resonance (MR) imaging is intrinsically multiparametric (ie, it is able to image signal from tissues whose intensities are determined by any of multiple unrelated tissue properties), any agent that has the ability to modify or manipulate any of these variable tissue properties to which the MR imaging process is sensitive can be potentially used as an MR contrast agent.
- •
Due to its associated powerful magnetic field and safety profile (when appropriately bound to its ligand molecules), the vast majority of contrast enhanced studies in clinical MRI today is accomplished via the utilization of a chelated gadolinium ion, wherein the major differences between the various types available today is due to variations in the specific ligand molecule selected to which the gadolinium ion is to be chelated.
- •
The predominant mechanism of action clinically used for contrast enhancement in MR imaging today is that of T1 shortening.
- •
Certain clinical indications, such as hyperacute stroke and/or neoplastic evaluations, may benefit from T2* shortening capabilities of these gadolinium-based contrast agent in what have become known as (contrast-enhanced) perfusion-weighted imaging sequences.
- •
The relaxivity of an agent is that characteristic that describes and quantifies the degree to which a given dose/concentration of the agent shortens the T1 of the tissue(s) that takes it up. Tissue relaxivity properties can be quantified as r1 (describing the magnitude of T1 shortening potentiation relative to delivered dose/concentration in the tissue) and r2 (describing the magnitude of T2* shortening potentiation relative to gadolinium-based contrast agent delivered dose/concentration in the tissue).
Introduction
The first gadolinium-based contrast agent (GBCA) was approved by the Food and Drug Administration (FDA) for use in the United States on June 28, 1988. In the nearly 25 years that have transpired since that time, the magnetic resonance (MR) industry has seen marked growth in the use and applicability of GBCAs in neuroradiologic imaging. Among the numerous hospitals of the author’s institution, the University of Pittsburgh Medical Center, GBCA administration varies from approximately 35% to 60% of all patients who pass through the doors of the MR suite. While early contrast enhanced MR imaging was essentially restricted to post contrast administration spin echo based 2D Fourier transform T1 weighted imaging sequences, we now commonly see contrast administration in conjunction with spin and gradient echo T1 weighted imaging sequences, T2 weighted post Fluid Attenuating Inversion Recovery (FLAIR) imaging, 2D as well as 3D imaging approaches, MR angiography, perfusion weighted MR imaging sequences, and other newer, novel imaging techniques. Unlike computed tomography (CT)- and radiography-based contrast agents, whose only true capabilities essentially lie in producing modification of the linear attenuation coefficient of the tissue(s) taking up those agents, the multiparametric nature of MR imaging itself is ideally suited to taking best clinical advantage of the multifactorial, multiple magnetically active properties, or r1 and r2 relaxivities, of these unique and fascinating agents.
Background
To more fully appreciate the unique nature of these agents as they interact with the magnetic fields used in the MR imaging process, a review of some of the imaging basics and physical properties at play is in order.
Radiography-based studies such as CT detect and differentiate tissues based on variations in their linear attenuation coefficients (LACs), which, in turn, is heavily based on the electron densities of the tissues through which the homogeneous x-ray beam will pass. The greater the electron density, the greater is the degree of attenuation of the x-ray beam and the whiter that tissue/object will appear on the resultant image. Two adjacent tissues with similar LAC values would therefore be difficult to differentiate on studies using x-ray–based technology. However, if these same 2 tissues differ in, for example, the rate at which an intravascularly administered electron dense contrast agent will reach or perfuse these tissues, one could time the x-ray irradiation event/exposure to coincide with a point in time when the relative electron densities, and therefore LAC values (induced by the variably perfusing contrast agent) of these 2 tissues would be markedly different. This would then produce images with greater densities and whiter depicted tissues from those which, at the time of irradiation, were being heavily perfused by this administered agent, and less from the adjacent and less-perfused, less–electron dense tissue. This is the basis of contrast agent use in CT and indeed all radiography-based studies. Note that with or without the use of an exogenously administered contrast agent, CT- and radiography-based physics remain essentially restricted to detecting and differentiating tissues based on—and only on—their LAC values. It is, in essence, a one-trick pony. It does indeed execute that “trick” astonishingly well, but it remains a one-trick pony nevertheless. If, in the end, the tissue LAC values are similar, then the CT (or other radiography-based) study will fail at contrasting and differentiating those 2 tissues from each other. Because contrast between a target tissue and its background tissue(s) is a necessary basis for achieving diagnosis, having or creating tissues with significantly different LAC values de facto is a necessary step for CT/radiography–based technology to successfully diagnose that patient.
MR Contrast Agents
The technology for successfully creating diagnostic images in MR is similar, yet simultaneously dissimilar, to that discussed for radiography technology. It is similar in that here, too, the MR imaging system will be attempting to detect a characteristic property of a tissue, and attempting to contrast it against an adjacent tissue for which that same characteristic property at that same time has a significantly different value. Granted, the LAC value per se will not be the tissue characteristic or property that the MR imaging system will detect because today’s MR imaging systems cannot detect or directly determine tissue LAC values. Nevertheless, it is still similar in that the MR imaging process will also rely on detecting differences in measured values of a given tissue property that the MR imaging system IS able to detect. The dissimilarities between MR-based technology on the one hand and CT- (and all radiogaphy-based) technology in the other, however, become especially fascinating. Whereas CT- and radiography-based studies have been shown to be one-trick ponies, limited in scope and sensitivity to the single tissue property known as LAC, the MR imaging system can be adjusted to provide sensitivity to any of various tissue properties–some of which are still being discovered and developed as this article is being written! Based on how the MR imaging parameters and variables are selected and adjusted, MR images can be acquired wherein the predominant mechanism of image contrast (that which determines whether a tissue is white, or dark, or anything in between) is dependent on such tissue properties known as T1, or T2, or T2*, or relative proton/hydrogen/spin density, or diffusion, or perfusion, or susceptibility, or gross coherent flow/motion, or “fat based,” or “water based,” “elasticity based,” and so on. Since MR first became a clinical tool in the early 1980s, the industry has repeatedly continued to introduce new parameters for which the MR imaging system hardware/software could be made to be sensitive to detect.
To further strengthen—and complicate—the potential to generate image contrast in MR imaging, we have already noted that image contrast may be dependent on any of various tissue properties, as noted earlier. However, image contrast may also be manipulated to be determined not only by any of these various tissue properties in isolation, but modifying the imaging parameters selected in the MR imaging process can result in image contrast being determined by any combination and “weighting” of any/all the mentioned tissue properties simultaneously. These imaging parameters can even be manipulated in such a way as to result in either synergistically additive signal or competitively destructive and signal-negating outcomes! This increases the potential number of ways that image contrast could be produced by virtually a factorial of the number of tissue parameters to which the MR imaging system can be adjusted to be able to detect. By means of illustration, an image could be made to be T1-weighted, whereby the predominant mechanism of contrast is determined by the relative T1 values of the tissues being detected such that the shorter the tissue T1 value, the brighter it would be depicted on the image. In contrast to this, another set of MR imaging parameter selections might result in the production of a set of images that would be referred to as T2 weighted, whereby the longer the T2 of the imaged tissue, the brighter it would be depicted on the image. One might modify these choices yet again to this time produce an image that would be referred to as proton density weighted, whereby the higher the concentration per unit volume, or density, of hydrogen nuclei in the tissues being detected, the brighter it would be depicted on the image. If desired, however, one could modify the parameter selection further to produce images wherein its displayed contrast could be dependent on virtually any mathematical combination of these that are desired, such as an image that is partially T2 weighted and partially relative proton density weighted at the same time. There is thus quite literally virtually no end to the number and types of image contrast combinations and “weightings,” as it were, that are available to the multiparametrically sensitive MR imaging system and its knowledgeable, experienced operator.
In this light, one can rapidly recognize that a contrast agent for an MR study would be any agent that has the ability to modify ANY of the tissue parameters to which MR imaging systems have been demonstrated to be sensitively able to detect—and/or any agent that can modify any combination of such tissue parameters.
Gadolinium-Based Contrast Agents: T1-Shortening Effects
This dizzying potential is brought under some modicum of clinical control by the early clinical availability of very few MR contrast agents. Indeed, at the initial FDA approval and clinical release of MR contrast agents in 1988 and for almost 2 decades thereafter, the clinically available MR contrast agents (at least those used for neuroradiologic imaging, which represented, and still represents, the extreme majority of all contrast-enhanced MR imaging to date) were based on the same “active ingredient,” and therefore all functioned via the same mechanism of action. They all relied on the predominantly T1-shortening property of the gadolinium ion, which has resulted in these GBCAs being used predominantly the same way—as T1-shortening agents, which, when acquiring so-called T1-weighted images, enhanced the signal most from the tissues into which these intravenously administered contrast agents were able to rapidly perfuse and then leak into their extracellular fluid spaces. The higher the administered dose and, most important, the higher the concentration of the agent in the extracellular fluid space of the tissue at the time that it was being imaged, the greater was the T1 shortening and therefore signal intensity of that tissue on T1-weighted images. The various agents released and FDA approved did have some differences, but their similarities—including and especially in efficacies, reported safety profiles, biodistributions, and half-lives—far outweighed any clinically relevant differences between them.
Thus, after these GBCAs were first approved for use in humans, their clinical applicability was moderately simple and straightforward, given that the industry found itself implementing relatively few, fixed types of imaging sequences (ie, tissue parameter sensitivities) for which contrast has been clinically applied to date. Practically speaking, then, for years following the FDA approval of the first GBCA in 1988, MR contrast agents were used for, and only for, shortening the T1 values of tissues that might differentially take up these administered agents, such that the tissue that took up the agent would be depicted as brighter (because of its shortened T1 value and therefore faster longitudinal magnetization recovery rate) than other tissues that either did not take up the administered contrast agent or did so at a notably slower rate. This “T1 weighted imaging” enhancement served as the basis for clinical GBCA administration for almost 2 decades.
GBCAs: T2*-Shortening Effects
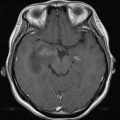
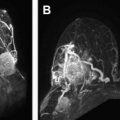
It was just a matter of time until the medical community recognized that there were also T2*-shortening properties inherent in these same magnetically active FDA-approved GBCAs. One could generate an MR imaging procedure that would be intentionally designed to emphasize the T2* properties of the imaged tissues, such that the shorter the T2* of the imaged tissue, the weaker was its signal and the darker it would appear on the resultant image, with longer T2* tissues appearing relatively brighter. On such imaging sequences, if these same GBCAs would be administered before image acquisition, their r2 (and therefore T2*-shortening) properties would produce signal loss from those tissues in whom these agents had achieved greatest concentration at time of imaging, with less signal loss and, therefore, greater relative signal from other tissues in which the GBCA concentration at time of imaging was lower. Further, as with the T1-shortening effect induced by the r1 properties of these agents, the greater the concentration of these agents in the tissues at the time of imaging, the greater was the T2*-shortening effect and, therefore, the greater was the induced signal loss in that tissue on the resultant image. This was found to be most clinically useful in assessing differences in macrovascularity and microvascularity and therefore rates of perfusion between tissues being images. By rapidly injecting a bolus of these GBCAs and ensuring that the image data acquisition transpired during the first passage, and therefore greatest concentration, of the administered GBCAs, the degree of signal loss was maximized in the tissue that perfused most rapidly. This was found to be of greatest clinical benefit in evaluating hyperacute ischemic events in which such perfusion-weighted studies can be rapidly performed and provide near real-time information as to tissue perfusion and, therefore, viability. Such perfusion-weighted imaging (ie, bolus GBCA administration coupled with carefully timed T2*-weighted imaging techniques) has also been successfully clinically applied to neoplastic processes, whereby the degree of vascularity often corresponds to clinically manifest aggressiveness of many malignancies.
Relaxivity
As noted earlier, the predominant application of a GBCA in the medical community was (and remains to this day) to provide T1 shortening and thus signal enhancement to the tissues that take up that agent. Practically speaking, the concept of “relaxivity” was neither discussed nor widely understood. This status quo first began to change around 2005. Again, a bit of introductory background information will prove useful.
Between June 1988 and November 2004, the 4 MR contrast agents for neuroradiologic application in the United States were gadopentetate dimeglumine (Magnevist, Bayer Healthcare, Germany), gadodiamide (Omniscan, General Electric Healthcare, USA), gadoversetamide (Optimark, Covidien), and gadoteridol (Prohance, Bracco Diagnostics, Italy). We have discussed that the administration of any of these GBCAs results in shortening of the tissue T1 properties (for the tissues that take up the agent into their extracellular spaces) and produces faster longitudinal magnetization recovery and therefore greater signal intensity on T1-weighted images for these tissues than they would otherwise have displayed had these GBCAs not been administered. Also noted was that the greater the concentration of any of these GBCAs in the tissue’s extracellular spaces (at the time imaging data are collected), the greater is the T1-shortening effect and, therefore, signal intensity on T1-weighted images. What has not been discussed, however, is the relative behavior of the approved agents. Put another way, if equal doses of these agents would be administered to the patient, would the degree of signal enhancement in that same tissue be expected to be the same—or different—among these agents?
Conceptually, what is being touched on can be thought of as the relative “potency,” in a sense, of the T1-shortening abilities among these GBCAs. If one were to administer the identical dose of each of these GBCAs to the patient, would the resultant acquired T1-weighted images be indistinguishable from each other, or would the degree of signal enhancement produced by the presence of one or more of these agents yield significantly more T1 shortening, and therefore signal, from that tissue than it would from other FDA-approved neuroradiologic GBCAs?
The concept being discussed—namely, the magnitude of T1 shortening (and, most important, signal enhancement) relative to the administered dose—can be summarized by one word: Relaxivity. Specifically, the r1 relaxivity of a GBCA describes how efficiently a GBCA shortens the tissue/sample T1 at a given concentration. Measured in units of per millimoles per second, the greater the r1, the greater is the T1 shortening and, therefore, the greater is the produced signal intensity on T1-weighted images for any given concentration of the agent.
Returning to theoriginal discussion, the reason that relaxivity was an almost unknown quantity among radiologists for nearly 20 years of clinical use of 4 different FDA-approved neuroradiologic GBCAs is because the relative relaxivities of these agents was found to be, from a clinical point of view, interchangeable. Put another way, the degree of clinically observed signal enhancement from similar administered doses of gadopentetate dimeglumine, gadodiamide, gadoversetamide, and gadoteridol was thought to be essentially the same. No claims of competitive signal intensity advantages or increases in diagnostic accuracy from using one of these agents relative to another were made. There are reported differences in the measured relaxivities among the various FDA-approved neuroradiologic GBCAs, to be sure. However, the clinical impact of these reported different relative r1 relaxivities proved to be sufficiently similar such that any differences that might mathematically exist among their measured r1 relaxivities did not reach clinically detectable or significant levels.
In 2004, however, the FDA approved the first GBCA for neuroradiologic application that had a significantly and clinically detectable higher r1 relaxivity than did the others that had been FDA approved to that date. When released, gadobenate dimeglumine (Multihance, Bracco Diagnostics, Italy) reported an r1 relaxivity that was substantially higher at practical clinically commonly used static MR imaging field strengths than the other available GBCAs that had been used to that time. Further, numerous comparative studies began to appear in the peer-reviewed literature that bore out the clinically detectable impact of this more potent T1-shortening ability per unit of administered dose of this agent in the form of increased sensitivity to lesion detection, increased ratio of lesion to background contrast, and improved diagnostic performance for various diseases compared to identical administered doses of lower relaxivity GBCAs.
Since the FDA approval of gadobenate dimeglumine in 2004, all new GBCAs approved by the FDA have been higher relaxivity agents. These include gadofosveset (Ablavar; for contrast-enhanced MR angiographic indications), gadoxetate disodium (Eovist; for hepatic imaging indications), and gadobutrol (Gadavist (Bayer Healthcare, Germany); for neuroradiologic indications). Comparative human studies for neuroradiologic imaging have just started to appear for the more recently approved gadobutrol. Interestingly, despite its higher reported relaxivity in human blood plasma than the 4 lower relaxivity agents just noted (1.5T r1 values of 5.2 L/mmol/s for gadobutrol relative to 4.1 for gadopentetate dimeglumine and 6.3 for gadobenate dimeglumine as reported by Pintaske and colleagues when measured in human blood plasma, or 1.5T r1 values of 4.7 L/mmol/s for gadobutrol relative to 3.9 for gadopentetate dimeglumine and 7.9 for gadobenate dimeglumine as reported by Rohrer and colleagues when measured in bovine plasma), it is reported to have an essential interchangeable diagnostic accuracy compared with gadoteridol, one of the lower relaxivity agents (65.1% accuracy of diagnosis for gadobutrol versus 65.5% for gadoteridol in 229 patients). This seems to document that despite mathematically higher r1 values for gadobutrol than the lower relaxivity agents such as gadoteridol, the magnitude of any r1 differences between gadobutrol and gadoteridol was not sufficiently higher to be of clinical diagnostic accuracy relevance. In a more recent direct comparison of gadobutrol to gadobenate dimeglumine when the same subjects were administered each agent at identical and clinically indicated doses and reexamined a few days apart, significantly increased lesion enhancement and contrast-to-noise ratio was observed between the enhancing pathology/lesion and the nonenhancing brain for the higher r1 relaxivity gadobenate dimeglumine than for the lower r1 relaxivity gadobutrol despite both being labeled as high relaxivity agents.
It should be noted that GBCA relaxivites are not constant and, in fact, may vary considerably under certain conditions, including and especially by field strength. In general, for most GBCAs, relaxivities decrease with increasing static magnetic field strengths. However, as documented so well by Laurent and colleagues and as explained further by Giesel and colleagues, because of the known protein binding property of gadobenate dimeglumine with human serum albumin (HSA) and the lack of significant protein binding for gadopentetate dimeglumine, Dotarem (Guerbet Corporation, France), gadodiamide, gadoteridol, and gadobutrol, this agent specifically exhibits increased r1 relaxivities at all tested field strengths, and especially so from the 0.3T to 1.5T range, compared with that which it would have been predicted to exhibit had there been no significant interactions and protein binding between gadobenate dimeglumine and HSA. The measured increased r1 relaxivities for gadobenate dimeglumine with increasing concentrations of HSA and the lack of significant increased r1 relaxivities with increasing concentrations of HSA for gadopentetate dimeglumine and gadobutrol further confirm the role of protein binding for specifically this agent in creating its higher r1 relaxivity values. Rohrer and colleagues’ observation of a relative decrease in r1 relaxivity advantage of gadobenate dimeglumine relative to gadobutrol or gadopentetate dimeglumine in water as opposed to plasma (4.0 for gadobenate dimeglumine, 3.3 for gadobutrol, 3.3 for gadopentetate dimeglumine at 1.5T) is further evidence of the clinical role that HSA binding plays with this, and only this, neuroradiologic GBCA.
Finally, it should be pointed out that all the arguments presented here explaining and demonstrating the advantages provided by higher r1 relaxivity agents for T1-weighted imaging applications apply in parallel to higher r2 relaxivity agents on T2*-weighted imaging. In such circumstances, at identical administered doses (technically, at higher concentrations in the extracellular spaces of the tissues being studied), the higher the r2, the greater is the signal loss on the same T2*-weighted imaging sequence and thus the greater the signal loss from these tissues. Although not clinically used as much as is postcontrast T1-weighted imaging today, higher r2 relaxivity agents would be expected to demonstrate similar clinical contrast-to-noise ratio advantages relative to lower r2 GBCAs at equivalent administered doses in more powerfully darkening the signal from the tissues that take up these agents compared with lower r2 GBCAs on T2*-weighted MR imaging examinations. This may well be even more evident at higher fields in which the clinical effects of shortening T2* are markedly more pronounced than they are at lower static magnetic field strength MR imaging systems. Further, higher concentrations of GBCA should also prove advantageous in providing for increased signal loss from those tissues taking up the agent compared to those agents with lower gadolinium concentrations. Of all the FDA approved neuroradiologic GBCA today, only gadobutrol is distributed at 1.0 molar concentrations, which is twice that of the 0.5 molar concentration found in each of the other FDA-approved neuroradiologic GBCAs available today.
Dose Versus Volume
One final point that should be stressed is that of the GBCAs FDA approved for neuroradiologic indications today, all but one are distributed in the same concentration, and all but one are approved to be administered at the same, standard dose. Specifically, gadopentetate dimeglumine, gadobenate dimeglumine, gadodiamide, gadoversetamide, and gadoteridol are all distributed as 0.5 Molar solutions. Gadobutrol is distributed at twice that concentration, namely, at 1.0 Molar. However, note that all 6 of these FDA-approved neuroradiologic GBCAs are approved to be administered to humans at 0.1 mmol/kg doses (with the additional exception that under certain specific situations, gadoteridol is also FDA approved to be administered at a total of triple dose, or a total administered dose of 0.3 mmol/kg for 1 MR imaging examination (this will be discussed in greater detail momentarily)). Thus, because all are approved to be administered to humans at the same delivered dose (ie, the same amount of gadolinium ions per patient mass) and because the concentration of gadolinium ions in gadobutrol is twice that of all the other 5 FDA-approved neuroradiologic GBCAs, this would mean that the volume of gadobutrol to be administered to patients for standard-dose administration should be half of that which it would be for any of the other 5 neuroradiologic GBCAs. For example, a 70-kg patient receiving 0.1 mmol/kg of a 0.5 Molar concentration of gadopentetate dimeglumine, gadobenate dimeglumine, gadodiamide, gadoversetamide, or gadoteridol would receive 0.2 mL/kg or 14 mL of any of these agents as a standard-dose administration. At twice the concentration, or 1.0 mol/L concentration of gadobutrol, that same patient, to receive the same approved standard dose, would receive 0.1 mL/kg, or 7 mL, of gadobutrol. Thus, 7 mL of gadobutrol is precisely the equivalent delivered gadolinium dose to the patient as 14 mL of gadopentetate dimeglumine, gadobenate dimeglumine, gadodiamide, gadoversetamide, or gadoteridol, and would all constitute a standard dose for a 70-kg patient.
Note, however, that today the only agent that carries an FDA labeling approving a higher than standard dose administration is gadoteridol, which under specific circumstances is FDA approved to be administered at a total of triple dose, or 0.3 mmol/kg (which is the same as a delivered volume of 0.6 mL/kg of this half molar concentration solution).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree