This article presents an overview of liver and biliary contrast agents including their mechanisms of action, dosage and elimination, current clinical indications, and potential future uses.
- •
Hepatobiliary-specific contrast agents can distinguish between hepatocyte- and non–hepatocyte-containing lesions. One important example is the ability of gadobenate dimeglumine and gadoxetic acid to differentiate focal nodular hyperplasia from hepatic adenoma, 2 benign lesions with different follow-up and treatment strategies.
- •
Hepatobiliary-specific agent use is controversial in hepatocellular carcinoma detection and characterization because they do not provide increased sensitivity with respect to the extracellular agents, their uptake may be compromised in the setting of abnormal liver function, and well-differentiated hepatocellular carcinoma may accumulate hepatobiliary-specific agents on delayed hepatocyte imaging, making them indistinguishable from benign hepatocyte-containing lesions.
- •
Contrast-enhanced magnetic resonance cholangiography has exciting potential uses, including troubleshooting abnormalities encountered at T2-weighted magnetic resonance cholangiography, preoperative biliary anatomy assessment, postoperative biliary tree complications such as bile leaks, and functional biliary tree imaging to aid in the diagnosis of choledocholithiasis and cholecystitis.
Introduction
Contrast agents have been used in magnetic resonance (MR) imaging since 1986. Since the clinical approval of gadolinium (Gd) deglumine in 1988, the daily use of MR contrast agents became widespread. MR imaging contrast improves detection and characterization of liver lesions by increasing lesion-to-liver contrast as a result of decreased T1 relaxation times of liver parenchyma and enhancing lesions.
The major classes of MR contrast agents currently used for liver imaging include extracellular Gd chelates, hepatobiliary-specific agents (including hepatocyte-selective and combined agents), reticuloendothelial agents, and blood pool agents. In this article, the extracellular and hepatobiliary-specific agents will be discussed in detail, highlighting clinical indications, mechanism of action, imaging pitfalls, current clinical applications, and potential future uses.
Extracellular contrast agents
Extracellular contrast agents, which are composed of Gd chelated to an organic compound, have been in clinical use the longest and remain the most frequently used MR contrast agents. Several formulations of extracellular agents exist ( Table 1 ); however, their pharmacologic and imaging characteristics are essentially identical. Some of the benefits of the extracellular Gd chelates are that they are considered safe when given at clinically applicable doses in patients without renal failure, they demonstrate other abdominal organ lesions in addition to those of the liver, and they are the least expensive.
| Generic Name | Abbreviated Name | Trade Name | Manufacturer |
|---|---|---|---|
| Gadopentetate dimeglumine | Gd-DTPA | Magnevist | Bayer, Wayne, NJ |
| Gadodiamide | Gd-DTPA-BMA | Omniscan | Nycomed Amersham, Princeton, NJ |
| Gadoteridol | Gd-HP-DO3A | ProHance | Bracco, Princeton, NJ |
| Gadoversetamide | Gd-DTPA-BMEA | Optimark | Mallinckrodt Imaging, Hazelwood, MO |
| Gadoterate meglumine a | Gd-DOTA | Dotarem | Guerbet, Villepinte, France |
| Gadobuterol a | Gd-BT-DO3A | Gadovist | Bayer, Wayne, NJ |
Extracellular contrast agents
Extracellular contrast agents, which are composed of Gd chelated to an organic compound, have been in clinical use the longest and remain the most frequently used MR contrast agents. Several formulations of extracellular agents exist ( Table 1 ); however, their pharmacologic and imaging characteristics are essentially identical. Some of the benefits of the extracellular Gd chelates are that they are considered safe when given at clinically applicable doses in patients without renal failure, they demonstrate other abdominal organ lesions in addition to those of the liver, and they are the least expensive.
| Generic Name | Abbreviated Name | Trade Name | Manufacturer |
|---|---|---|---|
| Gadopentetate dimeglumine | Gd-DTPA | Magnevist | Bayer, Wayne, NJ |
| Gadodiamide | Gd-DTPA-BMA | Omniscan | Nycomed Amersham, Princeton, NJ |
| Gadoteridol | Gd-HP-DO3A | ProHance | Bracco, Princeton, NJ |
| Gadoversetamide | Gd-DTPA-BMEA | Optimark | Mallinckrodt Imaging, Hazelwood, MO |
| Gadoterate meglumine a | Gd-DOTA | Dotarem | Guerbet, Villepinte, France |
| Gadobuterol a | Gd-BT-DO3A | Gadovist | Bayer, Wayne, NJ |
Mechanism of action
Extracellular contrast agents enter the liver via the hepatic artery and portal vein and freely redistribute from the intravascular to the interstitial space. Liver lesion detection and characterization with extracellular agents rely on differential blood flow between the liver and the tumor. Gd is highly paramagnetic and shortens the T1 (longitudinal) and T2 (transverse) relaxation times of adjacent water protons, causing T1-weighted signal enhancement and T2-weighted signal loss. At clinical doses of the extracellular fluid agents, T1 shortening is observed in essentially all tissues. Although iodinated contrast and Gd chelates have similar pharmacokinetics, Gd exhibits an amplification effect as a result of its paramagnetic properties, allowing for depiction of subtle areas of contrast accumulation that may not be seen on contrast-enhanced computed tomography (CT). Gd chelates offer better enhancement of the blood pool on equilibrium-phase images than iodinated contrast agents, enabling better delineation of blood vessels than on contrast-enhanced CT.
Dosage and elimination
The recommended dose of extracellular fluid agents is 0.1 mmol/kg, rendering a dose of 20 mL effective in most adults for liver imaging. Renal elimination predominates with the extracellular agents. In patients with normal renal function, documented adverse effects of the extracellular contrast agents are mild and include headache, nausea, and vomiting. Anaphylaxis is exceedingly rare. Patients with renal failure are at risk for nephrogenic systemic fibrosis after the administration of any Gd-based contrast agent; however, these risks can be minimized by adhering to restrictive Gd-based contrast agent administration guidelines.
All extracellular fluid agents are labeled class C drugs by the Food and Drug Administration (FDA) with a teratogenic effect demonstrated in animal studies; however, no controlled human studies have been performed. Therefore, Gd chelates are typically avoided in pregnancy, particularly in the first trimester. The effect of Gd excreted in breast milk is unknown, but studies have shown that the expected absorbed dose by the infant from ingesting breast milk is less than 0.05% of the recommended pediatric dose.
Imaging protocol
Three- (or more) phase dynamic postcontrast imaging with T1-weighted 2- or 3-dimensional (3D) spoiled gradient echo sequences with chemically selective fat suppression is of paramount importance with the extracellular fluid agents because lesion detection and characterization hinge on differential blood flow between the liver parenchyma and the characteristic enhancement patterns of lesions. A sample contrast-enhanced liver MR protocol is listed in Table 2 .
| Sequence | TR (ms) | TE (ms) | Flip Angle (°) |
|---|---|---|---|
| SSTSE coronal | ∞ | 80 | 90 |
| SSTSE axial | ∞ | 140 | 90 |
| T2 SPIR axial | 1720 | 80 | 90 |
| T1 GRE axial | |||
| In phase | 180 | 4.6 | 80 |
| Out of phase | 180 | 2.3 | 80 |
| Diffusion axial b = 0 and b = 600 | |||
| ADC d map | |||
| 3D T1 GRE with SPIR | 3.5 | 1.7 | 15 |
| Precontrast | |||
| Arterial phase – obtained using a test bolus | |||
| Portal venous – acquired approximately 30 s after the arterial phase | |||
| Equilibrium – acquired approximately 30 s after the portal venous phase | |||
| Hepatocyte phase | |||
| Gadobenate dimeglumine –acquired 60–240 min after initial administration | |||
| Gadoxetic acid – acquired 10–20 min after initial administration | |||
| Subtraction images of the arterial, portal venous, and equilibrium phases | |||
Timing of the arterial phase of dynamic MR imaging
To accurately capture the arterial phase of enhancement, which is critical for vascular imaging and assessment of arterially enhancing masses, it is imperative to match the peak of the contrast bolus with the acquisition of the central lines of k-space, which encode tissue contrast. To achieve this, several different methods are available. The first uses a fixed scan delay that is constant from patient to patient. This method produces erratic contrast timing because of physiologic differences (especially cardiac output) between patients and is considered to be the least accurate. A second method uses MR “fluoroscopic” triggering, which involves administration of the entire volume of contrast and acquisition of multiple low-resolution MR images through a prescribed region, such as the aorta. Acquisition of a high-resolution breath-hold sequence begins immediately after a certain intensity threshold has been reached. This method is potentially problematic if the patient is unable to breath-hold once the threshold value has been reached because the entire contrast bolus has already been administered. The most reliable method for capturing the arterial phase involves the use of a small test bolus of Gd, usually 2 mL, followed by a 20- to 30-mL saline chaser. A low-resolution image, which repeats every second, is chosen through a specific anatomic region near the target organ. For liver imaging, the upper abdomen is customarily chosen. The technologist measures the time to peak enhancement after giving a 2-mL test bolus. Subsequently, determination of proper timing depends on the k-space acquisition strategy of the particular sequence. If the contrast-encoding center lines of k-space are acquired first (contrast-enhanced, centric reordered 3D MR angiography), the scan delay will then be equivalent to the time to peak enhancement as determined by the test bolus. If a linear k-space strategy is used, whereby the peripheral lines of k-space, which encode for detail, are acquired first, followed by acquisition of the center lines of k-space at the half-way point of the scan, then a timing run equation should be used to match the bolus peak with acquisition of the center lines of k-space:
where AT is acquisition time, IT is injection time, and TTP is time to peak aortic enhancement.
Extracellular contrast agent pitfalls
Malignant and benign liver lesions can demonstrate overlap in their enhancement patterns with the extracellular contrast agents given their nonspecific mechanism of action. In addition, timing of the dynamic phase postcontrast sequences can be challenging in patients who are unable to hold their breath. In situations in which a free breathing protocol is necessary, the arterial phase along with its diagnostic information is severely compromised.
Hepatobiliary agents
To overcome some of the limitations of extracellular contrast agents, hepatobiliary agents were developed. The hepatobiliary agents are paramagnetic compounds that are taken up to varying degrees by functioning hepatocytes and excreted in bile, causing T1 shortening and, thus, increased signal intensity of the liver and biliary tree and hepatocyte-containing lesions. By extension, non–hepatocyte-containing lesions appear hypointense on T1-weighted images. There are 2 types of hepatobiliary-specific agents: hepatocyte-selective (mangafodipir trisodium) and combined (extracellular and hepatocyte-selective) agents (gadobenate dimeglumine and gadoxetic acid) ( Table 3 ). Mangafodipir was removed from the US market in 2006; however, much of the experience with hepatobiliary-specific agents has been with this contrast agent and it shares delayed phase imaging characteristics with the other hepatobiliary-specific agents. Hepatocyte-selective agents are more expensive that the nonspecific extracellular agents, but improved liver lesion detection and characterization can avoid additional imaging tests or even biopsy.
| Generic Name | Abbreviated Name | Trade Name | Manufacturer |
|---|---|---|---|
| Mangafodipir trisodium a | Mn-DPDP | Teslascan | GE Healthcare, Princeton, NJ |
| Gadobenate dimeglumine | Gd-BOPTA | MultiHance | Bracco, Princeton, NJ |
| Gadoxetic acid | Gadoxetic acid | Eovist b | Bayer, Wayne, NJ |
a Taken off the US market in 2006.
b Eovist is the trade name in the United States. Primovist is the trade name in the European Union, Australia, and Japan.
Indications/uses
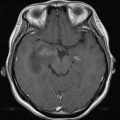
Hepatobiliary-specific agents allow for improved liver lesion detection in the hepatobiliary phase, characterization of lesions as hepatocellular or nonhepatocellular, and evaluation of biliary tree anatomy and function. Given their robust biliary excretion (≥50%), mangafodipir and gadoxetic acid provide good delayed hepatic and biliary tree imaging, whereas gadobenate dimeglumine with its 5% biliary excretion can only depict the central biliary tree reliably. Mangafodipir is taken up only by hepatocytes; thus, its major indications for use are to characterize lesions as hepatocellular or nonhepatocellular ( Fig. 1 ) and for liver metastasis surveillance, particularly in patients with colorectal adenocarcinoma. Mangafodipir only allows for delayed phase imaging. If an extracellular contrast is administered in conjunction with mangafodipir for the same MR examination, dynamic postcontrast imaging of the liver can also be performed. Of note, the biliary applications of hepatobiliary-specific agents are not approved for clinical use in the United States.
Mechanism of action
Hepatocyte-Selective Agents
Mangafodipir is a manganese chelate that is taken up by hepatocyte vitamin B6 receptors as a result of its chemical similarity to vitamin B6. Extrahepatic uptake of mangafodipir is observed when some manganese dissociates from its ligand within the blood circulation. Mangafodipir shortens the T1 and T2 relaxation times of water protons, and at low concentrations, T1 shortening predominates, resulting in T1 high signal intensity.
Combined Agents
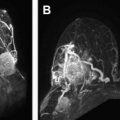
The combined agents, gadobenate dimeglumine and gadoxetic acid, have extracellular Gd chelate, hepatocyte-selective, and blood pool characteristics, allowing for dynamic phase imaging for liver lesion detection and characterization similar to the extracellular contrast agents. Their uptake into hepatocytes from the blood and excretion into the bile via the organic anion transport protein are analogous to bilirubin uptake. In their hepatocyte-selective phase, these agents provide prolonged opacification of liver parenchyma. At dynamic phase imaging, the Gd-based hepatobiliary-specific agents (gadobenate dimeglumine and gadoxetic acid) have been shown to be equivalent to the extracellular agents for liver lesion characterization. Although the dynamic phases of the extracellular contrast agents and gadobenate dimeglumine are similar, gadoxetic acid does not demonstrate a pure arterial phase and its equilibrium and hepatobiliary phases overlap, altering the typical enhancement pattern of several lesions, including high-flow hemangiomas ( Fig. 2 ).
Dosage and Elimination
The recommended adult dosagee of mangafodipir is 0.5 μmol/kg injected slowly at a rate of 2 to 3 mL/min. Hepatic enhancement peaks at 15 minutes and persists for several hours. More than 50% of the injected mangafodipir is eliminated through the biliary system, with the remainder eliminated by the kidneys. Mangafodipir is a class C drug and should not be administered to pregnant women. The effect of excreted mangafodipir in breast milk on nursing infants in not known.
The recommended adult dosage of gadobenate dimeglumine is 0.1 mmol/kg administered in a bolus injection (2 mL/s). Dynamic imaging can be performed, and peak hepatic enhancement occurs at 1 to 2 hours with peak biliary excretion, which is necessary for functional biliary imaging occurring at approximately 1 hour. Up to 5% of gadobenate dimeglumine is excreted via the biliary system with 95% being eliminated through the kidneys. The recommended adult dosage of gadoxetic acid is 0.025 mmol/kg administered in a bolus injection (1–2 mL/s). If gadoxetic acid is administered more rapidly, a ring artifact around the aorta may appear. As with gadobenate dimeglumine, dynamic imaging can be performed; however, hepatic enhancement peaks between 10 minutes to hours with peak biliary excretion, which is necessary for functional biliary imaging occurring at approximately 10 minutes. Gadoxetic acid undergoes approximately 50% biliary excretion and 50% renal excretion.
Gadobenate dimeglumine and gadoxetic acid are labeled class C drugs by the FDA and should not be administered to pregnant women. The effect of excreted Gd in breast milk on nursing infants is unknown.
Side effects of the hepatobiliary-selective agents are mild and include flushing, nausea, dizziness, raised blood pressure and heart rate, injection site pain, and taste perversion.
Imaging Protocol
As mentioned previously, the combined agents have the same features as the nonspecific extracellular agents paired with the advantage of hepatocyte specificity. Given this, gadobenate dimeglumine and gadoxetic acid use the same imaging protocol as the extracellular agents with the addition of a delayed hepatobiliary sequence obtained at approximately 120 and 20 minutes, respectively. Because of the 120-minute delay between gadobenate dimeglumine injection and the hepatobiliary phase, the patient must be scanned twice. With gadoxetic acid, all of the imaging is performed at once with acquisition of the T2-weighted or diffusion-weighted images between the dynamic and hepatobiliary phases to shorten the examination time. Given the prolonged hepatobiliary phases of enhancement of both gadobenate dimeglumine and gadoxetic acid, additional imaging to assess for enhancement on the hepatobiliary phase. Gadobenate dimeglumine has applications in MR angiography because of its transient binding to serum albumin and resultant increased T1 relaxivity of gadobenate dimeglumine compared with other Gd chelates.
Hepatobiliary-Specific Agent Pitfalls
The T2 shortening effect of hepatobiliary/combined agents necessitates routine T2-weighted MR cholangiopancreatographic (MRCP) images to be obtained before contrast administration because the bile ducts become hypointense on T2-weighted images with these contrast agents. Hyperintense signal intensity on T1-weighted images of a hematoma or of iodine may mimic a bile leak on contrast-enhanced cholangiography. Hepatic insufficiency may require a delay in image acquisition.
The attractive feature of gadoxetic acid is the ability to perform both dynamic and hepatocyte phase imaging in a reasonable time-frame in the same examination, which cannot be done with gadobenate dimeglumine. The Gd-based contrast agents carry a risk of nephrogenic systemic fibrosis (NSF). To the best of our knowledge, gadoxetic acid has not been related to NSF. However, gadobenate dimeglumine has shown an association with several reported confounded NSF cases. The hepatocyte phase can be performed as early as 10 minutes after gadoxetic acid injection in noncirrhotic patients. In cirrhotic patients or in patients with elevated bilirubin levels, a longer delay (>20 minutes) is necessary.
Liver Lesion Characterization
Benign liver lesions occur commonly in the general population, making accurate characterization of liver lesions important. At dynamic imaging, the hepatobiliary-specific agents have been shown to be equivalent to the nonspecific extracellular agents at liver lesion characterization based on enhancement characteristics. As previously mentioned, gadoxetic acid does not have a pure arterial phase and the equilibrium and hepatobiliary phases overlap, altering the typical enhancement patterns of several lesions such as high-flow hemangiomas. Because the hepatobiliary agents are taken up by functioning hepatocytes in the delayed phase, they are useful in distinguishing between lesions that are of hepatocellular or nonhepatocellular origin and, thus, benign and malignant lesions because malignant lesions typically do not take up hepatocyte-specific contrast agents. Furthermore, the addition of hepatobiliary phase imaging to the dynamic series increases the sensitivity and accuracy for detection of focal hepatic lesions. Table 4 is a summary of the typical MR appearance of common solid benign and malignant focal liver lesions.