USG should be performed after a minimum of 4 hours of fasting, since ingestion of fatty food stimulates the contraction of the gallbladder (GB). GB also contracts after administration of cholecystokinin.
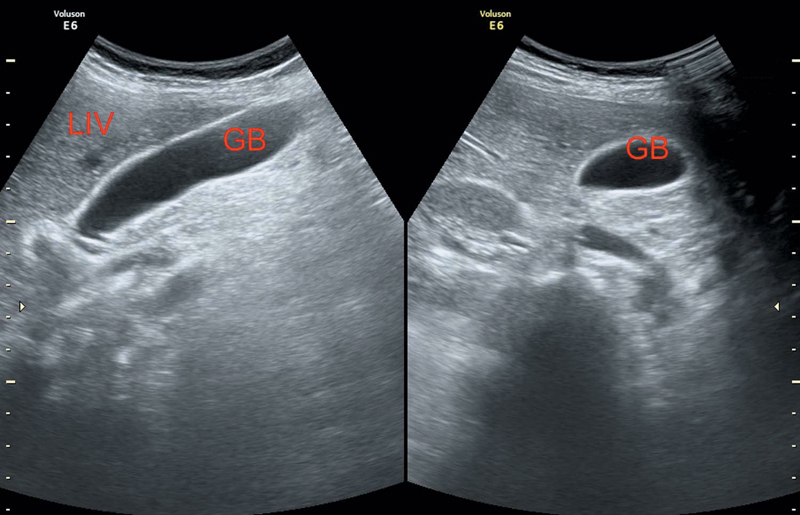
GB lies in the inferior margin of the liver in the same anatomic plane as the middle hepatic vein (MHV) (Figure 3.1).
Interlobar fissure extends from the origin of the right portal vein (RPV) to the GB fossa and used as a landmark.
Parts of GB—Fundus, body, and neck (Hartmann’s pouch, a common location for impaction of stones).
Figure 3.1 Depicting normal gallbladder and liver in different sections.
Valve of Heister: Located in cystic duct, prevents it from collapsing/overdistending.
Hartmann’s pouch: Outpouching of GB neck.
Normal GB wall thickness—3 millimeters.
>5 millimeters is definitely abnormal.
Normal GB demonstrates posterior acoustic enhancement.
Overdistended GB: If transverse diameter >4 centimeters and longitudinal diameter 9–10 centimeters. May be known as gallbladder hydrops, if measurement exceeds the normal.
Reexamine after a fatty meal. If no contraction occurs, look for obstruction in the cystic duct and common bile duct (CBD) by stones, clots, ascariasis, and external compression by lymph nodes or neoplasm.
The contracted GB appears thick walled and may obscure luminal or wall abnormalities.
1. Ectopic GB
2. Septate GB
3. Duplication of GB
4. Phrygian cap (GB fundus folded over the body)
In patients with jaundice
Distended GB is suggestive of CBD obstruction (intra-/extraluminal). Look for intrahepatic biliary radicles (IHBRs).
Nondistended GB suggests nonobstruction of CBD or obstruction above the level of cystic duct.
Curvoisier’s sign—Patients presenting with painless jaundice and palpable gallbladder (RUQ mass) are unlikely to have stones in GB. Pancreatic/biliary neoplasm should be presumed as a cause until proven otherwise.
Risk factors: Fat, fertile, female, pregnancy, diabetes, and so on.
• Mobile, echogenic foci giving posterior acoustic shadowing.
• Stones change in position within the lumen as the patient moves in comparison to nonshadowing polyps, which are constant in position. Calculus may sometimes get impacted at neck.
Scanning with the patient in lateral decubitus or upright position allows the stone to roll within the GB.
Wall-Echo-Shadow (WES) complex: In a GB filled with stones, GB wall is first visualized in the near field. Followed by the bright echo of the stone. Followed by the acoustic shadowing. Commonly mistook for either rib shadow or bowel gas (Duodenum lies posterior to GB and may cause shadowing).
Bile sludge/sand/microlithiasis
Sludge is a precipitate of bile solutes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree