Chapter Outline
Examination Techniques: Gallbladder
Examination Techniques: Biliary Tract
Rapid advances in technology and refinements in both noninvasive and invasive techniques have improved the ability of imaging methods to make more precise diagnoses in disorders of the biliary tract. Ultrasound and computed tomography (CT), because of wide availability and ease of performance as well as high diagnostic accuracy, are the first-line imaging techniques. Magnetic resonance cholangiopancreatography (MRCP) has assumed a larger role as a rapid, accurate, and noninvasive method of evaluating the bile ducts and has replaced diagnostic endoscopic retrograde cholangiopancreatography (ERCP) in most instances. Modern magnetic resonance (MR) and CT techniques including use of biliary-excreted contrast agents and postprocessing reformation methods, such as multiplanar reformation (MPR), maximum intensity projection (MIP), and volume rendering, allow detailed evaluation of the biliary tract with excellent accuracy and patient tolerance as well as three-dimensional data sets that can be cholangiographically displayed. Percutaneous transhepatic cholangiography (PTC) and ERCP are methods of direct cholangiography used for evaluation of biliary ductal disease. These techniques are invasive, but they are also safe and widely available. Improvements in the technical aspects of PTC and ERCP have led to the development of various interventional biliary procedures performed from both percutaneous and endoscopic routes. Plain radiography plays a minor role in imaging of the gallbladder and bile ducts. The traditional indications for operative and postoperative cholangiography remain unchanged; both techniques allow direct opacification of the biliary tree but require surgical access and have limited diagnostic use. Biliary scintigraphy also has a limited role in biliary imaging, mainly for confirming acute cholecystitis and identifying bile leaks.
Normal Anatomy
Gallbladder
The gallbladder is an elliptical organ located in a fossa on the undersurface of the liver between the right and left lobes. Although size and shape vary, the relaxed gallbladder is approximately 10 cm long and 3 to 5 cm in diameter. Size may increase after vagotomy, in diabetes, or after cystic duct or common duct obstruction. Normal capacity is approximately 50 mL. The normal gallbladder wall is 2 to 3 mm thick, and the mucosa is composed of simple columnar epithelium. The gallbladder is usually apposed to the liver surface by parietal peritoneum. Rarely, the peritoneal reflection may be loose, forming a mesentery that allows the gallbladder enough mobility to extend into the pelvis or left abdomen, herniate into the lesser sac, or undergo torsion. The gallbladder is positioned partially or completely in an intrahepatic location in 10% of cases.
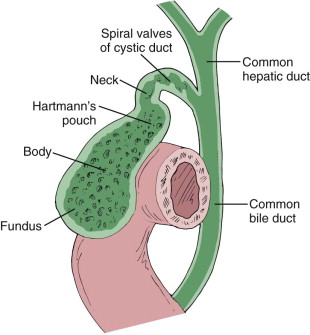
The gallbladder is divided into four parts—fundus, body, infundibulum, and neck ( Fig. 73-1 ). The fundus is the rounded distal tip, which may project below the anterior inferior liver edge ( Fig. 73-2 ). A characteristic deformity associated with septation and partial folding over of the gallbladder, the phrygian cap, may be found in the fundus. The body is the midportion of the gallbladder, which may be in contact with the duodenum and hepatic flexure. The infundibulum (Hartmann’s pouch) is the focally enlarged segment between the body and the neck. The neck of the gallbladder lies between the body and the cystic duct and points toward the porta hepatis. A mucosal fold, the junctional fold, is frequently seen near the gallbladder neck. The gallbladder neck bears a constant relationship to the major interlobar fissure and undivided right portal vein or main portal vein, an important anatomic relationship for imaging.
Cystic Duct
The gallbladder is attached to the common bile duct (CBD) by the cystic duct, which is usually 2 to 4 cm long and contains tortuous folds, the spiral valves of Heister (see Fig. 73-1 ). The cystic duct usually joins the common hepatic duct (CHD) from the right lateral aspect approximately halfway between the porta hepatis and the ampulla of Vater to form the CBD. The point at which the cystic duct joins the CHD is variable, from high in the upper extrahepatic bile duct or one of the intrahepatic ducts (more often the right) to low at the ampulla. The cystic duct usually runs parallel to the CHD at least for a short distance and may insert either anteriorly or posteriorly or spiral around to insert on the medial aspect. The two ducts may have a long parallel course and can be encircled in a common connective tissue sheath ( Fig. 73-3 ).

Bile Ducts
Intrahepatic Ducts
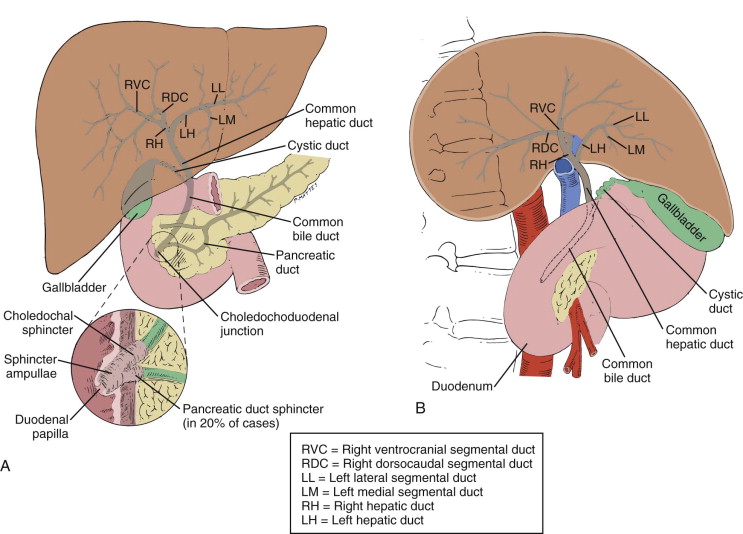
The liver is divided into right and left lobes on the basis of portal vein anatomy and biliary drainage. The right lobe is divided into anterior and posterior segments, and the left lobe is divided into medial and lateral segments by the fissure of the ligamentum teres. The bile ducts generally follow the internal hepatic segmental anatomy; however, marked variation in the branching pattern is common. Small branching interlobar bile ducts merge into larger ducts until the major left and right hepatic ducts are formed. A left medial segment duct and a left lateral segment duct normally join to form the main left hepatic duct. The right hepatic duct branches near its takeoff from the CHD. In approximately 60% of patients, the right hepatic duct has a dorsocaudal branch, with a characteristic hooklike configuration proximally, draining the posterior segment of the right lobe, and a ventrocranial branch, draining the anterior segment of the right lobe. Variations in the anatomic arrangement of the bifurcation branches are common, however, and it may be impossible to differentiate the anterior and posterior segmental branches on frontal cholangiograms. Common bifurcation variations include drainage of either anterior or posterior right lobe segmental ducts into the left hepatic duct, or a trifurcation configuration may occur. The left hepatic duct is more anterior and is usually longer and wider than the right hepatic duct. The left hepatic duct has a longer extrahepatic course and tends to dilate more with obstruction than the right hepatic duct does, presumably because there is less surrounding liver. Ductal drainage of the caudate lobe is variable and may be related to the left or right ductal system.
Extrahepatic Ducts
The right and left hepatic ducts emerge from the liver and unite to form the 3- to 4-cm-long CHD, which then joins the cystic duct to form the CBD. The union of the right and left main hepatic ducts is usually just outside the liver but may be lower, resulting in a shorter CHD or CBD. The CHD courses ventrally and inferiorly from the porta hepatis in the hepatoduodenal ligament accompanied by the portal vein, which lies posteriorly, and the hepatic artery, which lies medially. As the CHD passes inferiorly, it angles anteriorly and then posteriorly, crossing over the right portal vein and joining the cystic duct to form the CBD as it courses behind the postbulbar duodenum (see Fig. 73-1 ). The CBD averages 6 to 7 cm in length and is usually divided into suprapancreatic, intrapancreatic, and ampullary segments. In approximately 70% of patients, the distal CBD courses through the pancreatic head; in a smaller percentage, the CBD is located in a groove on the posterior surface of the pancreas. The CBD enters the posterior medial aspect of the second portion of the duodenum through an oblique, 1- to 2-cm-long intramural tunnel terminating at the papilla of Vater.
The exact union of the CBD and the pancreatic duct at the ampulla varies. Most commonly, the two ducts join in the duodenal wall and have a short common channel (<5 mm). On occasion, separate orifices are present at the ampulla, or the ducts unite, forming a long common channel before entering the duodenal wall ( Fig. 73-4 ). The sphincter of Oddi surrounds the common channel, and the choledochal sphincter (sphincter of Boyden) surrounds the CBD from its entrance into the duodenal wall to its junction with the pancreatic duct. The extrahepatic ducts are sparse in muscle fibers (except in the cystic duct and the sphincter areas) and are composed primarily of elastic fibers. This allows relatively rapid change in size in response to fluctuations in intraductal pressure. With age, loss of elasticity may occur, resulting in enlargement of the duct, so-called ductomegaly of aging.

Anatomic Variations
Anatomic variations and anomalies of bile duct anatomy are common (see Chapter 76 ). Although most are of no pathologic significance, an understanding of these variations is important to avoid misdiagnosis. Anatomic variations have been reported in 23% to 46% of cholangiograms, with the most common sites of involvement at the hepatic bifurcation and in the insertion of the cystic duct. An aberrant right hepatic duct (4.6%) entering at a variety of locations (including low along the CHD or into the cystic duct), an accessory right hepatic duct (1.9%), and a high or low insertion of the cystic duct are congenital anomalies of significance because of the potential for injury at biliary surgery (see Chapter 81 ).
Examination Techniques: Gallbladder
Modern gallbladder imaging involves primarily ultrasound and CT. Although the gallbladder is readily imaged by MR, this technique is less often used in gallbladder diagnosis because CT and ultrasound are accurate, quicker, less expensive, and easier to obtain. MR and MRCP, however, may be used as the initial imaging study in patients with suspected gallbladder carcinoma because of the greater ability to assess extent of disease and vascular involvement. Real-time sonography is the dominant screening method for the detection of gallbladder disease. Multidetector CT (MDCT) is commonly used to initially evaluate gallbladder disease, particularly neoplastic conditions and complicated cholecystitis, because of its ability to rapidly produce isotropic images of the upper abdomen.
Plain Radiography
Plain abdominal radiography is the simplest and least expensive imaging method that may identify gallbladder disease, but the yield is low, and this study is not used as a primary technique for assessment of suspected biliary or gallbladder disease. However, it is frequently the first study obtained in patients with upper abdominal pain, and gallbladder disease is occasionally apparent on the study. The normal gallbladder is not visible on plain radiographs. Only 10% to 15% of gallstones are sufficiently calcified to be visualized on the plain abdominal radiograph. “Porcelain” gallbladder, emphysematous cholecystitis, and milk of calcium bile (see Chapter 77 ) are other pathologic gallbladder conditions with characteristic findings that can be diagnosed on plain radiographs. A soft tissue mass in the right upper quadrant may be seen with hydrops of the gallbladder and gallbladder carcinoma. Rarely, noncalcified cholesterol gallstones are visible on the abdominal radiograph as a result of nitrogen-containing clefts that produce a lucent, triradiate appearance, the “Mercedes-Benz” sign.
Ultrasound
Real-time sonography is the most widely used diagnostic study for the gallbladder and is the primary screening examination for gallbladder disease. The gallbladder is visible on sonograms in virtually all fasting patients despite body habitus or clinical condition. Gallbladder sonography is noninvasive, quick, and easy to perform. The examination can be performed portably and, because no ionizing radiation is used, is safe in pregnant and pediatric patients. Adjacent upper abdominal organs can be imaged simultaneously. The success rate of obtaining a diagnostic study is more than 95%.
By far the most common indication for gallbladder sonography is the detection of gallstones. Overall, the sensitivity, specificity, and accuracy of ultrasound for detection of gallstones is 95% to 99% in most series. The frequency of indeterminate studies with ultrasound is low. False-positive ultrasound findings are uncommon and are due primarily to polyps, folds, or cholesterolosis of the gallbladder. Although ultrasound is excellent for the demonstration of calculi, it does not provide direct information about gallbladder function or cystic duct patency. Sonography does have limitations in assessing the size and number of stones in cases of multiple stones. Sonography is useful to confirm the diagnosis of acute cholecystitis. Ultrasound has been shown to have a positive predictive value of 92% and a negative value of 95% for diagnosis of acute cholecystitis in patients with gallstones and a positive sonographic Murphy’s sign. Complications of cholecystitis, including gallbladder perforation, gangrenous cholecystitis, and emphysematous cholecystitis, are usually readily seen by ultrasound. Gallbladder carcinoma, polyps, metastatic nodules, and adenomyomatosis are uncommon conditions of the gallbladder with characteristic findings on sonography (see Chapters 77 and 79 ).
Technique
The gallbladder is examined after the patient has fasted for at least 6 hours. This allows maximal distention of the gallbladder and enhances the detectability of stones. For most patients, real-time scanning is performed with a 3.5- or 4-MHz transducer. In thin patients or those with an anteriorly positioned gallbladder, a 5-MHz transducer provides superior resolution. A transducer of the highest possible frequency should be used because spatial resolution is improved when the transducer focal zone is the same depth as the gallbladder. The examination is begun with the patient in the supine position. Scanning is performed in the right subcostal region or in one of the lower intercostal spaces, in approximately the anterior axillary line. The gallbladder is located in the longitudinal axis by identifying the major interlobar fissure of the liver ( Fig. 73-5A ). Views are obtained in the longitudinal and transverse planes to allow visualization of the entire gallbladder. Different degrees of inspiration may be necessary to move the gallbladder away from the overlying costal cartilage ( Fig. 73-5B, C ). Various scanning positions are used; decubitus positioning is often helpful in displaying the gallbladder, displacing bowel gas, unfolding kinks, and allowing small stones hidden in the neck to roll into the fundus to become detectable. The dependent portion of the gallbladder, particularly the neck, should be scrutinized for hidden stones ( Fig. 73-5D ). Suspended deep inspiration often serves to move the gallbladder into a more accessible position below the ribs. Magnified views, high-frequency transducers, and upright or Trendelenburg positioning are helpful adjuncts. Color Doppler sonography may be used in assessing cystic artery and wall flow in patients with acute cholecystitis or gangrenous cholecystitis and in evaluation of gallbladder carcinoma and metastatic disease to the gallbladder. If the gallbladder is not readily identified in its usual subhepatic position, other locations must be evaluated to exclude a positional anomaly. Examination of the gallbladder is always accompanied by evaluation of the bile ducts.

Normal Anatomy
The normal gallbladder in the fasting patient appears as an oval sonolucent structure with a thin (2-3 mm), uniformly smooth wall (see Fig. 73-5B, C ). It is located by identifying the major interlobar fissure of the liver, which is apparent as a highly reflective line (because of periportal fat extending into the fissure) (see Fig. 73-5A ). The interlobar fissure is an important sonographic landmark because of its constant relationship to the gallbladder neck. Although gallbladder shape and size vary, the sonographic upper limits of normal size are approximately 8 to 10 cm in length and 4 to 5 cm in anterior-posterior diameter. Folds are commonly seen as echogenic foci adjacent to the wall. The junctional fold is a fold between the body and the infundibulum of the gallbladder, a common anatomic variant seen on sonography. If the gallbladder is not visualized by ultrasound, the most likely cause is prior resection or a scarred contracted gallbladder containing calculi. Agenesis of the gallbladder, calcification of the gallbladder wall, and intramural or intraluminal gas are other causes of nonvisualization (see Chapter 82 ).
Computed Tomography
The gallbladder in fasting patients is nearly always identified on CT scans of the upper abdomen. Although gallstones are frequently visible, CT is not used as a primary examination for detection of gallstones because of its lower sensitivity (80%-85%) and higher cost compared with ultrasound. Calcified gallstones are manifested as high-density foci within the gallbladder lumen, and noncalcified stones are seen as low-attenuation filling defects within the surrounding bile. Although acute cholecystitis is accurately evaluated with sonography or scintigraphy, CT is often used if the upper abdominal pain is nonspecific or if complicated cholecystitis is suspected. CT easily depicts mural thickening, gallbladder dilation, wall edema, septation, and increased bile density, which allows diagnosis. The main indication for CT in gallbladder disease is for the diagnosis and staging of gallbladder carcinoma (see Chapter 79 ) and evaluation of the complications of cholecystitis, such as perforation and pericholecystic abscess. Less common entities, such as porcelain gallbladder, milk of calcium bile, and emphysematous cholecystitis, are readily identified and have characteristic CT findings (see Chapter 77 ).
Technique
The gallbladder is usually scanned as part of a routine upper abdominal examination. Multislice CT scanning of the upper abdomen is performed during a single breath-hold after rapid bolus intravenous infusion of contrast material. This permits visualization of the gallbladder and optimal delineation of the gallbladder wall, intrahepatic biliary ducts, and extrahepatic bile duct by enhancing the contiguous liver and pancreatic parenchyma as well as blood vessels. Volumetric imaging with the latest generation scanners allows reconstruction in multiple planes and different slice thicknesses. Images of 2- to 5-mm slice thickness are used routinely for review. Postprocessing with reconstruction of axial images at 1.5 to 3 mm can be performed and may be helpful in clarifying suspicious areas and in maximizing stone detection. Oral contrast material is routinely used in scanning the upper abdomen. However, in searching for smaller noncalcified stones, scans obtained without contrast material using thin sections filmed at narrow window settings optimize stone detection.
Normal Anatomy
The normal gallbladder on CT scans is a low-density, fluid-filled, elliptical structure in the interlobar fissure of the liver ( Fig. 73-6A ). A thin (2-3 mm) wall is often seen in normal patients and may show contrast enhancement. The gallbladder neck is superior and medial to the fundus. The gallbladder neck is often folded, and a portion may be cut in cross section. More caudally, the fundus of the gallbladder projects anteriorly and laterally and may touch the anterior abdominal wall or the colon. The duodenal sweep, hepatic flexure, and gastric antrum are contiguous structures ( Fig. 73-6B-D ). Significant variations in gallbladder size, shape, and position may be seen; however, the gallbladder neck maintains a constant position relative to the major interlobar fissure. The collapsed gallbladder may be more difficult to identify on CT scans.

Cholescintigraphy
Cholescintigraphy is used primarily for the diagnosis of acute cholecystitis; 3 to 5 mCi of technetium Tc 99m iminodiacetic acid ( 99m Tc-IDA) compounds is injected intravenously, and the tracer is taken up by the liver and rapidly excreted into bile without undergoing conjugation, allowing visualization of the gallbladder and bile ducts ( Fig. 73-7 ). Frequent anterior images are obtained up to 1 hour. Delayed imaging up to 4 hours and possibly 24 hours may be necessary in some instances. Nonfilling of the gallbladder on cholescintigraphy indicates functional obstruction of the cystic duct and is considered diagnostic of acute cholecystitis in the appropriate clinical setting. If the gallbladder fills, the cystic duct is deemed to be patent and acute cholecystitis is not present. This technique is highly sensitive and specific for the diagnosis of acute cholecystitis (95%-98%), and it is the procedure of choice to confirm the diagnosis. Intravenous morphine sulfate and sincalide can assist gallbladder filling. Sincalide is a cholecystokinin analogue that produces gallbladder contraction and empties the gallbladder before the study, allowing the gallbladder to more readily fill with the tracer.

Magnetic Resonance Imaging
The technology of MRI of the gallbladder and biliary ductal system has continued to evolve since the early 1990s. The gallbladder is routinely imaged on conventional MR studies of the liver and upper abdomen with T1- and T2-weighted sequences. Techniques for imaging of the gallbladder or bile ducts may be tailored to delineate either the wall of the gallbladder and bile ducts and the surrounding soft tissue or the biliary fluid within the lumen (see Chapter 75 ).
Imaging of the lumen requires optimal contrast between the biliary fluid and the surrounding tissues. Bright signal fluid techniques are generally used with heavily T2-weighted sequences to produce an MR cholangiopancreatogram. The development of MRCP has expanded the role of MRI as a noninvasive method to examine the biliary system. MRCP is performed with heavily T2-weighted sequences that depict fluid in the biliary ducts, pancreatic duct, and gallbladder as high signal intensity, whereas adjacent solid organs and flowing blood have little or no signal. The images produced resemble those of ERCP ( Fig. 73-8 ). Although the primary goal of MRCP is to delineate the biliary and pancreatic ducts, incidental and intentional imaging of the gallbladder is possible even in the nonfasting patient. In many cases, the cystic duct and its site of insertion into the bile duct are also visualized. Although MRCP results in high-resolution images of the gallbladder, its role relative to ultrasound and CT for evaluation of gallbladder disease is limited primarily to problem solving, not to primary diagnosis, with the exception of gallbladder carcinoma. MR provides comprehensive imaging of the gallbladder and bile ducts as well as of the surrounding structures, a feature most helpful in staging of tumors arising from or involving the gallbladder.

Technique
Conventional MRI of the gallbladder and bile ducts frequently combines the use of T1- and T2-weighted sequences. T1-weighted fat suppression sequences with and without intravenous gadolinium chelates may be helpful in demonstrating the lumen as well as the wall of the gallbladder and the bile ducts. T2-weighted sequences may be used in evaluating the surrounding soft tissues. Heavily T2-weighted MR sequences are used to perform MRCP. A number of sequences have been used since its introduction, including two-dimensional fast spin-echo and three-dimensional fast spin-echo. Technical refinements provided by the half-Fourier rapid acquisition with relaxation enhancement (RARE) sequence allow rapid imaging, such that the entire biliary tract can be imaged during an 18-second breath-hold. A typical MRCP examination comprises multiple acquisitions obtained at variable angles that optimally delineate the biliary tract and gallbladder. The half-Fourier RARE sequence minimizes magnetic susceptibility artifacts, such as those associated with surgical clips and bowel gas. A thin-slab, multislice technique is often used in both axial and coronal planes. From these source images, three-dimensional reconstructions may be generated with an MIP algorithm. No intravenous or oral contrast material is administered.
Normal Anatomy
On MRI, the gallbladder lumen can have a high or low signal intensity, depending on the chemical composition of bile and the pulse sequence used ( Fig. 73-9 ). Concentrated bile is high signal intensity on T1- and T2-weighted images, whereas dilute bile is low in signal intensity on T1-weighted images because of its higher water content. Because concentrated bile has a greater specific gravity than dilute bile, concentrated bile settles in the dependent portion of the gallbladder. On MRCP, gallbladder calculi, regardless of composition, appear as low signal intensity filling defects within the high signal intensity bile ( Fig. 73-10 ). Calculi as small as 2 mm can be identified. In addition to calculi, MRCP can depict neoplastic disease of the gallbladder and its extent. Adenomyosis of the gallbladder may be incidentally identified when the fluid-filled Rokitansky-Aschoff sinuses are seen within the gallbladder wall.


Examination Techniques: Biliary Tract
A number of examination techniques are available for evaluation of the biliary ducts. In selection of an imaging technique, several factors must be considered, including clinical presentation, diagnostic information desired, body habitus, and anatomic alterations from previous surgery. If direct cholangiography with PTC or ERCP is used, the potential for conversion to a therapeutic intervention must be considered.
Ultrasound and CT are frequently used as the primary noninvasive methods for screening of patients with suspected ductal disease, although MRCP is being used more often and is now considered the primary evaluation method of choice for biliary ductal disease. MRCP is noninvasive and can be performed rapidly, depicting the intrahepatic and extrahepatic bile ducts as well as the pancreatic duct and surrounding structures. Although CT cholangiography has been widely used in Europe and on a limited basis in the United States for ductal evaluation, this technique is rarely used in current practice. CT cholangiography provides information similar to that of MRCP but requires intravenous administration of a cholecystographic agent before the CT study. This technique has several limitations, including use of contrast agents with the associated risk of reaction, lack of ready availability of the contrast agents used, inconsistent opacification of the ducts from the contrast agents, and limited opacification of the ducts in patients with biliary obstruction.
Direct opacification of the bile ducts by PTC or ERCP can provide detailed information about ductal anatomy or pathologic changes; however, these are invasive procedures. PTC or ERCP may also serve as a preliminary step to nonsurgical therapeutic interventions, such as biliary drainage, stent placement, stone removal, or stricture dilation. Biliary scintigraphy is occasionally useful in detection of bile leaks, evaluation of biliary enteric anastomoses, or diagnosis of early or segmental biliary obstruction. Operative cholangiography and postoperative cholangiography are standard methods to evaluate the bile ducts after surgical access to the ductal system. Plain radiography has a limited role and is rarely useful in defining bile duct disease.
Plain Radiography
The biliary ductal system is visible on plain radiographs only when it is outlined with air or calcification. Air in the biliary tree most commonly results from a surgically created biliary-enteric anastomosis. Erosion of a gallstone into the gastrointestinal tract and erosion of a peptic ulcer or tumor into the biliary tree are other causes of biliary-enteric fistula that may result in biliary air. Rarely, calcified stones in the bile ducts are visible on plain film.
Ultrasound
Evaluation of the bile ducts in search of stones, mass, or obstruction is one of the main applications for ultrasound. Real-time ultrasound readily depicts dilated biliary ducts, which in most instances is indicative of biliary obstruction. The extrahepatic bile duct can be seen in most patients regardless of body habitus or clinical condition. Because the bile duct is oval in cross section in the majority of patients, measurement of the transverse diameter on axial images correlates more closely with ductal diameters measured on ERCP. The CHD is the most easily visualized portion of the extrahepatic biliary system and can be rapidly visualized and measured in virtually all patients. Intrahepatic ducts are rarely seen unless they are dilated. The distal CBD may be obscured by gas in the duodenum. The primary goal of biliary sonography is the detection of dilated ducts because the size of the extrahepatic duct is a fairly sensitive indicator of the presence of biliary obstruction. Early changes of intrahepatic and extrahepatic ductal dilation are readily seen with ultrasound. Frequently, the lesion causing the biliary obstruction is identified as well. Ultrasound is an accurate and reliable technique to assess the intrahepatic and extrahepatic ducts as well as adjacent structures, such as the pancreas.
Technique
The bile ducts are best evaluated with high-resolution real-time equipment and the highest frequency transducer possible: 3.5 MHz in obese patients and 5 MHz in thin patients. Optimal imaging of the CHD and proximal CBD is obtained by parasagittal scanning with the patient in the supine left posterior oblique or left lateral decubitus position. The CHD is identified as a tubular sonolucency anterior and lateral to the proximal main portal vein or the undivided right portal vein ( Fig. 73-11A ). The right hepatic artery passes between the posteriorly located portal vein and the anteriorly located CHD. In 10% to 15% of patients, the artery is anterior to the CHD. The standard measurement of the CHD is made at this level. The measurement is made from interior wall to interior wall perpendicular to the scan plane. Doppler sonography of the porta hepatis may be needed to distinguish the bile ducts from adjacent vascular structures.

The distal CBD is more difficult and frequently impossible to image because of overlying gas in the duodenum and hepatic flexure. Visualization can be improved by scanning with the patient in the semierect (60 degrees to the vertical) right posterior oblique position in the transverse rather than in the parasagittal plane ( Fig. 73-11B ). This position minimizes antral and duodenal gas, allows fluid to enter the antrum and duodenum, and allows the left lobe of the liver to descend, creating an acoustic window. With this technique, the distal duct can be seen in up to 90% of cases. The specific point of union of the CHD with the cystic duct is usually not seen.
After examination of the extrahepatic ductal system, the proximal ducts and intrahepatic ducts are examined with the patient in the supine or left posterior oblique position. The normal right and left main hepatic ducts can be visualized coursing anterior to the undivided right portal vein and the initial segment of the left portal vein, respectively.
Normal Anatomy
The normal intrahepatic ducts are less than 1 to 2 mm in diameter and are usually not visible. Although visualization of intrahepatic ducts generally implies biliary dilation, larger central intrahepatic ducts can occasionally be visualized anterior to the portal veins in the right and left lobes near the porta hepatis in normal thin patients with use of a 5-MHz transducer. Gross intrahepatic duct dilation is easy to detect sonographically as the “parallel-channel” sign, formed by dilated intrahepatic ducts running anterior and parallel to the portal vein tributaries. Dilated intrahepatic ducts tend to have acoustic enhancement posteriorly, which distinguishes them from veins. The use of color Doppler is helpful to distinguish bile ducts from small hepatic vessels. This is especially so for the left lobe of the liver, where parallel branching hepatic anterior and portal veins may mimic dilated left intrahepatic ducts.
The normal CHD measures 4 to 5 mm or less on sonograms. The CBD measures 4 to 6 mm normally, with a 6- to 7-mm diameter considered equivocal. These measurements reflect the internal dimension of the duct. A diameter of more than 8 mm is indicative of ductal dilation. Sonographic measurements of duct size are smaller than those obtained by direct cholangiography because there is no radiographic magnification or distention resulting from injected contrast material. Some variation in extrahepatic ductal diameter may be due to elastic properties of the bile ducts, which can expand and contract rapidly during normal physiologic filling and emptying, with Valsalva maneuver, or with deep inspiration. There is controversy about whether extrahepatic ductal diameter increases with aging. In a study by Wu and coworkers of 256 normal patients, the CBD size was shown to increase roughly 1 mm per decade after the age of 50 years, indicating that an apparently enlarged CBD may be seen in normal elderly patients. This study also suggested that the upper limit of normal may be up to 10 mm in the elderly population. Two additional studies, one with a cohort of 350 patients and another with a cohort of 45 patients, support these data. These findings, however, were refuted in a study by Horrow and colleagues of 258 patients that did not confirm an association between age and size of the extrahepatic bile duct in an asymptomatic adult population.
Ductal Diameter and Biliary Obstruction: Limitations
Sonography has an overall accuracy of more than 95% in the detection of dilated ducts and diagnosis of biliary obstruction. However, bile duct caliber does not always correlate with the presence or absence of biliary obstruction. Biliary obstruction without dilation may be seen in patients with low-grade or intermittent obstruction resulting from stricture or small stones and in patients with sclerosing cholangitis. Alternatively, dilated ducts may be seen in the absence of obstruction in patients with prior biliary surgery or patients with resolved obstruction. The decreased elasticity of a dilated duct may result in persistent dilation despite relief of the obstruction. Intestinal hypomotility, recent laparotomy, hyperalimentation, and prolonged fasting can cause ductal dilation presumably secondary to factors that inhibit relaxation of the sphincter of Oddi. An enlarged CBD may be seen in normal, unobstructed elderly patients. Ultrasound is accurate in diagnosing the level of obstruction in 92% to 95% of cases and identifying the cause of obstruction in 70% to 88%.
Postcholecystectomy Dilation
Whether dilation of the duct occurs after cholecystectomy has been debated in the literature for years. It has been proposed that in the absence of a gallbladder, the CBD dilates to function as a reservoir. Two studies, however, suggest that if the CBD is normal before surgery, it generally remains so after surgery unless disease intervenes. A reassessment of the effect of cholecystectomy on duct size found that after cholecystectomy, most patients did not have significant compensatory dilation of the duct. Once a duct dilates, it may lose elastic recoil and never return to normal. Accordingly, some postcholecystectomy patients have biliary “dilation” but nonobstructed ducts. The maximal upper limit of the CBD allowed after cholecystectomy is 10 mm. The general recommendation is that further studies are warranted if the CHD measures 6 mm or greater in symptomatic patients.
Fatty Meal or Cholecystokinin Sonography
Administration of a fatty meal followed by sonography is an adjunctive maneuver that provides functional information, helps identify patients who require further evaluation with direct cholangiography, and increases the accuracy of ultrasound in detecting obstruction. This technique is helpful in postcholecystectomy patients with suspected obstruction in the absence of ductal dilation, in patients with equivocal duct size, and in asymptomatic patients with abnormal results of liver function studies suggesting occult obstruction. Magnified views of the CHD are obtained, and the internal diameter is measured at a fixed point. A fatty meal or intravenous cholecystokinin is administered, and another measurement of CHD caliber is obtained 30 to 45 minutes later if a fatty meal is used and 5 to 10 minutes later if cholecystokinin is used. A fatty meal and cholecystokinin cause gallbladder contraction, sphincter of Oddi relaxation, and increased bile flow. The normal, nonobstructed duct decreases in size or does not change in caliber. An increase in caliber—or, if the duct is initially dilated, a failure to decrease in caliber—suggests some degree of ductal obstruction and the need for further evaluation. A true change in ductal diameter occurs only if the size changes by 2 mm or more. Using these criteria, Simeone and colleagues reported 84% sensitivity for fatty meal sonography in predicting the presence or absence of CBD obstruction.
Computed Tomography
Continued evolution of CT technology, including refinements of multidetector scanning technology, has enhanced the utility of CT for evaluation of biliary duct disease. With the use of high-resolution scanners and fine collimation, minimally dilated intrahepatic and extrahepatic ducts are now easily visible. Visualization of the entire CBD is routine on CT scans of the upper abdomen. Imaging is not inhibited by overlying gas. CT is more reliable than sonography in determining the caliber of intrahepatic and extrahepatic ducts. In addition, because of more complete delineation of the total length of the CBD, CT is also more useful than sonography for precisely defining the site and cause of biliary obstruction. Whereas ultrasound has been used to screen patients with biliary obstruction in the past, CT and MR are now the first-line diagnostic studies and are no longer used as a follow-up study after ultrasound to refine the data or to confirm anatomy. CT has an accuracy of 96% to 100% in detecting the presence of biliary obstruction, 90% in determining the level of obstruction, and 70% in identifying the cause of obstruction. The reported sensitivity of CT for detection of bile duct stones is 72% to 88%. In addition, CT can often differentiate benign from malignant causes of obstruction and can provide guidance for biopsy and staging of malignant neoplasms.
Technique
Optimal CT scanning of the bile ducts requires rapid intravenous infusion of a bolus of contrast material combined with rapid scanning in the portal venous phase, usually 70 to 80 seconds after bolus injection of contrast material (100-150 mL). With current volumetric MDCT technology, the entire abdomen, with complete depiction of the intrahepatic and extrahepatic biliary tree, can be imaged in less than 5 seconds. MDCT scanners produce a volumetric data set that can be reconstructed in multiple dimensions for interpretation. Standard reconstruction includes 2- to 5-mm-thick axial images. High-quality multiplanar (MPR) coronal, coronal oblique, and curved planar reformatted images as well as three-dimensional reconstructions of the biliary ductal system may be helpful in defining complex anatomy or to map the ducts for planning of therapy. In cases of biliary obstruction, coronal reconstruction or three-dimensional reformations of the dilated bile ducts from data obtained during routine scanning can be produced successfully by taking advantage of the “negative” contrast effect of low-attenuation bile in dilated ducts relative to the adjacent enhanced visceral organs and vessels. *
* References .
In searching for CBD stones, scanning may be performed initially without oral or intravenous contrast material. Although dense contrast medium in the bowel has the potential to cause streak artifacts across the CBD, obscuring detail, such artifacts are rarely a problem with MDCT scanners. Duodenal contrast medium may obscure an impacted stone in the ampulla, and contrast medium in a perivaterian duodenal diverticulum can simulate a stone. Contrast enhancement of the vasa vasorum of the CBD wall may also mimic choledocholithiasis. Reconstruction in thin slices of 1 to 2 mm or the use of coronal reconstructions may allow better demonstration of calculi. * Proper selection of the correct window width and level is necessary to optimize visualization of the CBD throughout its entire course from the porta hepatis to the intrapancreatic portion.* References .
Multiphase imaging during late arterial and portal venous phase imaging may improve visualization of hypovascular tumors involving the bile ducts. Delayed imaging (10-20 minutes after administration of contrast material) has been shown to be helpful in diagnosis of cholangiocarcinoma. The tumor demonstrates increased retention of contrast material compared with the adjacent liver.Normal Anatomy
On MDCT scans of the liver and upper abdomen, the CHD and CBD are usually visualized throughout their entire course ( Fig. 73-12A-D ). Visualization of intrahepatic ducts on CT has been considered evidence of biliary dilation and obstruction. However, with MDCT scanners, bolus contrast enhancement, and 2- to 5-mm-thick scans, visualization of normal intrahepatic ducts may be seen in 40% of normal individuals. The average size of the normal intrahepatic ducts is 2 mm in the central liver and 1.8 mm in the periphery. Demonstration of intrahepatic bile ducts on CT scans does not necessarily indicate biliary obstruction; however, few normal intrahepatic ducts should be seen. Truly dilated intrahepatic ducts are readily apparent and, when present, indicate biliary tract disease. Bile ducts appear as water-density tubular branching structures converging at the porta hepatis. The left and right hepatic bile ducts course through the porta hepatis and join to form the CHD lying anterior to the portal vein.











