Chapter Outline
Esophagus, 124
Stomach, 131
Types of Barium Studies, 131
Upper Gastrointestinal Series, 131
Percutaneous Gastrostomy, 132
Normal Appearance, 132
Types of Gastric Lesions, 133
Peptic Ulcer Disease, 133
Ménétrier Disease (Giant Hypertrophic Gastritis), 134
Eosinophilic Gastroenteritis, 134
Gastroduodenal Crohn Disease, 135
Zollinger-Ellison Syndrome, 135
Gastric Polyps, 135
Gastric Carcinoma, 135
Gastric Lymphoma, 136
Metastases, 136
Carney Triad (Rare), 136
Benign Tumors, 136
Gastric Volvulus, 137
Gastric Varices, 137
Benign Gastric Emphysema, 137
Duodenum and Small Bowel, 137
Colon, 147
Liver, 160
General, 160
Diffuse Liver Disease, 162
Infections, 165
Tumors, 166
Trauma, 171
Vascular Abnormalities, 171
Transplant, 173
Biliary System, 174
General, 174
Biliary Lithiasis, 176
Inflammation, 178
Tumors, 181
Cystic Diseases, 183
Interventions, 183
Pancreas, 185
General, 185
Congenital Anomalies in Adults, 187
Pancreatic Trauma, 187
Pancreatitis, 187
Transplant, 194
Spleen, 195
Peritoneum and Abdominal Wall, 197
Differential Diagnosis, 200
Esophagus, 200
Stomach, 202
Duodenum, 203
Jejunum and Ileum, 204
Colon, 208
Liver, 210
Biliary System, 212
Pancreas, 213
Spleen, 215
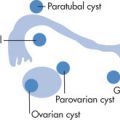
Peritoneal Cavity, 215
Other, 215
Esophagus
General
Anatomy
Normal Esophageal Contour Deformities ( Fig. 3.1 )
- •
Cricopharyngeus
- •
Postcricoid impressions (mucosal fold over vein)
- •
Aortic impression
- •
Left mainstem bronchus (LMB)
- •
Left atrium (LA)
- •
Diaphragm
- •
Peristaltic waves
- •
Mucosa: thin transient transverse folds: feline esophagus (vs. thick folds in chronic reflux esophagitis); tiny nodules in older adults: glycogenic acanthosis

Gastroesophageal Junction (GEJ) Anatomy ( Fig. 3.2 )
- •
Phrenic ampulla: normal expansion of the distal esophagus; does not contain gastric mucosa
- •
A-ring (for a bove; Wolf ring): indentation at upper boundary of the phrenic ampulla
- •
B-ring (for b elow): indentation at lower boundary of the phrenic ampulla; normally not seen radiologically unless there is a hiatal hernia
- •
Z-line ( z igzag line): squamocolumnar mucosal junction between esophagus and stomach; not visible radiologically
- •
C-ring: diaphragmatic impression
- •
The esophagus lacks a serosa. Upper one-third has striated muscle; lower two-thirds has smooth muscle.

Peristaltic Waves
- •
Primary contractions: initiated by swallowing; distally progressive contraction waves strip the esophagus of its contents; propulsive wave
- •
Secondary contractions: anything not cleared from the esophagus by a primary wave may be cleared by a locally initiated wave; propulsive wave
- •
Tertiary contractions: nonpropulsive, uncoordinated contractions; these random contractions increase with age and are rarely of clinical significance in absence of symptoms of dysphagia; nonpropulsive wave; only peristaltic activity in achalasia
Peristalsis should always be evaluated fluoroscopically with the patient in a horizontal position. In the erect position the esophagus empties by gravity.
Swallowing ( Fig. 3.3 )
| Swallowing Phase | Tongue | Palate | Larynx | Pharyngeal Constrictors |
|---|---|---|---|---|
| Dorsum controls bolus; base assumes vertical position | Resting | Resting | Resting |
| Strips palate and moves dorsally | Velopharynx closure | Epiglottis deflects, larynx moves anterosuperiorly | Middle constrictors |
| Meets relaxing palate | Begins descent | Vocal folds close, epiglottis retroflexes | Inferior constrictors |
| Returns to resting | Resting | Returns to resting | Completion of constriction, resting |

Esophageal Ultrasound (US) ( Fig. 3.4 )
Endoscopic esophageal transabdominal or gastric US is performed mainly for staging of cancer or detection of early cancer. Most mass lesions and lymph nodes (LNs) appear as hypoechoic structures disrupting the normal US “gut signature,” consisting of different layers of hyperechogenic and hypoechogenic lines.

Esophageal Disease
Schatzki Ring
Thin annular symmetric narrowing at the junction of esophagus with the stomach (B-ring level). Present in 10% of population, 30% of whom are symptomatic. Symptoms (dysphagia, heartburn) usually occur if rings cause esophageal narrowing of ≤12 mm. Now considered a consequence of reflux.
Esophageal Webs and Rings
Mucosal structures (web = asymmetric, ring = symmetric) may occur anywhere in the esophagus.
Associations
- •
Iron-deficiency anemia (cervical webs): Plummer–Vinson syndrome
- •
Hypopharyngeal carcinoma
Hiatal Hernia
There are two types:
Sliding hernia (axial type), 95%
- •
GEJ is above the diaphragm.
- •
Reflux is more likely with larger hernias.
- •
“Mixed” variant when hernia and esophagus are not in straight axis.
- •
Paraesophageal hernia, 5%
- •
GEJ is in its normal position (i.e., below diaphragm).
- •
Part of the fundus is herniated above the diaphragm through esophageal hiatus and lies to the side of the esophagus.
- •
Reflux is not necessarily associated.
- •
More prone to mechanical complications; prophylactic surgery a consideration
- •
Usually nonreducible
- •
Imaging Features ( Fig. 3.5 )
Criteria for diagnosing sliding hernia:
- •
Gastric folds above diaphragm
- •
Concentric indentation (B-line) above diaphragm
- •
Schatzki ring above diaphragm
- •

Associations
- •
Esophagitis, 25%
- •
Duodenal ulcers, 20%
Approach
- •
Maximally distend distal esophagus in horizontal position; distention can be achieved by sustained inspiratory effort
- •
Determine the type of hernia
- •
Determine if there is reflux by Valsalva maneuver or Crummy water-siphon test (patient in supine right posterior oblique (RPO) position continually drinks water to see if barium refluxes into midesophagus or above)
Diverticula
Lateral Pharyngeal Pouches
AP esophagram at level of pharynx demonstrates lateral outpouchings through weakness in thyrohyoid membrane. Large in glassblowers and wind instrument players.
Zenker Diverticulum ( Fig. 3.6 )
Pulsion diverticulum originates in the midline of the posterior wall of the hypopharynx at an anatomic weak point known as Killian dehiscence (above cricopharyngeus at fiber divergence with inferior pharyngeal constrictor). During swallowing, increased intraluminal pressure forces mucosa to herniate through the wall. The cause of Zenker diverticulum is not firmly established, but premature contraction and/or motor incoordination of the cricopharyngeus muscle are thought to play a major role. Complications include:
- •
Aspiration
- •
Ulceration
- •
Carcinoma

Killian-Jamieson Diverticulum ( Fig. 3.7 )
- •
Below cricopharyngeus
- •
Off midline
- •
Lateral to cervical esophagus

Epiphrenic Diverticulum
- •
May occasionally be recognized on chest radiographs (CXRs) by presence of soft tissue mass (often with air-fluid level) that mimics a hiatal hernia.
- •
Large diverticulum can compress the true esophageal lumen, causing dysphagia.
Traction Diverticulum
- •
Outpouching of midesophagus as a result of adjacent inflammatory process (e.g., tuberculosis [TB]).
- •
Calcified mediastinal LNs
Pseudodiverticulosis
Numerous small esophageal outpouchings representing dilated glands interior to the muscularis. Usually occur at >50 years of age. Dysphagia is the presenting symptom. Underlying diseases include candidiasis, alcoholism, and diabetes.
Associated Findings
- •
Esophageal stricture may occur above and/or below stricture.
- •
Esophagitis
Imaging Features
- •
Thin flask-shaped structures in longitudinal rows parallel to the long axis of the esophagus
- •
Diffuse distribution or localized clusters near peptic strictures
- •
Much smaller than true diverticula
- •
When viewed en face, the pseudodiverticula can sometimes be mistaken for ulcers. When viewed in profile, however, they often seem to be “floating” outside the esophageal wall with barely perceptible channel to the lumen; esophageal ulcers almost always visibly communicate with the lumen.
Esophagitis
Esophagitis may present with erosions, ulcers, and strictures and rarely with perforations and fistulas.
Types
Infectious (common in debilitated patients)
- •
Herpes
- •
Candidiasis
- •
Cytomegalovirus (CMV)
- •
Chemical
- •
Reflux esophagitis
- •
Corrosives (lye)
- •
Iatrogenic
- •
Radiotherapy
- •
Extended use of nasogastric (NG) tubes
- •
Drugs: tetracycline, antiinflammatory drugs, potassium, iron
- •
Other
- •
HIV
- •
Scleroderma
- •
Crohn disease (rare)
- •
Dermatologic manifestations (pemphigoid, dermatomyositis bullosa)
- •
Imaging Features
- •
Thickening, nodularity of esophageal folds
- •
Irregularity of mucosa: granularity, ulcerations
- •
Retraction, smooth, tapered luminal narrowing, stricture just above GE junction
Infectious Esophagitis ( Fig. 3.8 )
Herpes simplex
- •
Small ulcers, <5 mm
- •
Normal mucosa between ulcers
- •
More diffuse than reflux ulcers
- •
Candidiasis
- •
Plaque like, reticular
- •
Shaggy margins
- •
Often involve entire esophagus
- •
CMV and HIV
- •
Typically, elliptical large ulcers but may be tiny ulcers such as herpes
- •
Etiologic distinction between CMV and HIV ulcers is important because therapies are different.
- •
Behçet disease may have a similar appearance.
- •
Mycobacterial
- •
Ulcers, sinus tracts
- •

Inflammatory Eosinophilic Esophagitis
- •
Dysphagia may be chronic, history of allergies, eosinophilia
- •
Segmental proximal or midesophageal mild narrowing
- •
May involve entire esophagus
- •
Increased risk of iatrogenic tear
- •
- •
Responds to steroids
Barrett Esophagus ( Fig. 3.9 )
Esophagus is abnormally lined with columnar, metaplastic acid-secreting gastric mucosa. It is usually due to chronic reflux esophagitis. Because there is an increased risk of esophageal cancer, close follow-up and repeated biopsies are recommended.

Imaging Features
- •
A reticular mucosal pattern, which may be discontinuous in the distal esophagus (short segment), is the most sensitive finding.
- •
Suspect the diagnosis if there is:
Upper or midesophageal stricture accompanied by reticular mucosal pattern below transition or ulcer
Low strictures: the majority cannot be differentiated from simple reflux esophagitis strictures, and biopsies are required
Boerhaave Syndrome ( Fig. 3.10 )
Spontaneous perforation of the esophagus as a result of a sudden increase in intraluminal esophageal pressure. Severe epigastric pain. Treatment is with immediate thoracotomy. Mortality, 25%.

Imaging Features
- •
Pneumomediastinum
- •
Pleural effusion (left > right)
- •
Mediastinal hematoma
- •
Rupture immediately above diaphragm, usually on left posterolateral side (90%)
Mallory-Weiss Tear
Mucosal tear in proximal stomach, across GEJ, or in distal esophagus (10%), usually caused by prolonged vomiting (alcoholics) or increased intraluminal pressure. Because the tear is not transmural, there is no pneumomediastinum.
Imaging Features
- •
Radiographs are usually normal.
- •
Intravasation rather than extravasation
- •
There may be subtle mucosal irregularity.
Achalasia
The gastroesophageal (GE) sphincter fails to relax because of degeneration of Auerbach plexus. The sphincter relaxes only when the hydrostatic pressure of the column of liquid or food exceeds that of the sphincter; emptying occurs more in the upright than in the horizontal position.
Types
- •
Primary (idiopathic)
- •
Secondary (destruction of myenteric plexus by tumor cells)
Metastases
Adenocarcinoma invasion from cardia
- •
Infectious: Chagas disease
Clinical Findings
- •
Primary occurs predominantly in young patients (in contradistinction to esophageal tumors); onset: 20–40 years
- •
Dysphagia, 100% to both liquids and solids when symptoms begin
- •
Weight loss, 90%
Diagnosis
- •
Need to exclude malignancy (fundal carcinoma and lymphoma destroying Auerbach plexus), particularly in older adults
- •
Need to exclude esophageal spasm
- •
Manometry is the most sensitive method to diagnose elevated lower esophageal sphincter (LES) pressure and incomplete relaxation.
Imaging Features ( Fig. 3.11 )
- •
Two diagnostic criteria must be met:
Primary and secondary peristalsis absent throughout esophagus
LES fails to relax in response to swallowing
- •
Dilated esophagus typically curves to right and then back to left when passing through diaphragm.
- •
There may be minimal esophageal dilation in the early stage of disease.
- •
Beaked tapering at GEJ
- •
Tertiary waves
- •
Air-fluid level in esophagus on plain radiograph
| Parameter | Esophageal Spasm | Achalasia |
|---|---|---|
| Symptoms | ||
| Dysphagia | Substernal | Xiphoid or suprasternal notch |
| Pain | Common | Rare |
| Weight loss | Rare | Common |
| Emotional | Common | Common |
| Motility | ||
| Waves | Simultaneous | Tertiary |
| LES relaxation | Present | Absent |
| Imaging Features | ||
| Esophageal contraction | Vigorous | Discoordinated |
| Esophageal emptying | Efficient | Poor |
| Response to Therapy | ||
| Pneumostatic dilation | Not indicated | Good |
| Surgery | Long myotomy | Low cardioesophageal myotomy |

Complications
- •
Recurrent aspiration and pneumonias, 10%
- •
Increased incidence of esophageal cancer
Treatment
- •
Drugs: nitrates, β-adrenergic agonists, calcium blockers (effective in <50%)
- •
Balloon dilatation (effective in 70%)
- •
Myotomy: procedure of choice
Scleroderma ( Fig. 3.12 )
Collagen vascular disease that involves the smooth muscle of esophagus, stomach, and small bowel (SB).

Imaging Features
- •
Lack of primary waves in distal two-thirds
- •
GEJ patulous unless stricture supervenes
- •
Reflux esophagitis (common)
- •
Strictures occur late in disease
- •
Esophagus dilates most when stricture supervenes
| Achalasia | Scleroderma | |
|---|---|---|
| Esophagus | Massively dilated | Mildly dilated |
| GEJ | Closed, tapers to beak shape | Open; stricture late |
| Horizontal swallow | Tertiary contractions | Primary in proximal third, tertiary contraction in distal two-thirds |
| Reflux | No | Yes |
| Complications | Aspiration pneumonia | Early: esophagitis Late: stricture, interstitial lung disease |
Diffuse Dysmotility ( Fig. 3.13 )
Characterized by intermittent chest pain, dysphagia, and forceful contractions. Diagnosis is diffuse esophageal spasm with manometry.

Types
- •
Primary neurogenic abnormality (vagus)
- •
Secondary reflux esophagitis
Imaging Features
- •
Nutcracker corkscrew esophagus
- •
Nonspecific esophageal dysmotility disorders
Chagas Disease (American Trypanosomiasis)
Caused by Trypanosoma cruzi, which multiply in reticuloendothelial system (RES), muscle, and glia cells. When these cells rupture and organisms are destroyed, a neurotoxin is released that destroys ganglion cells in the myenteric plexus. Mortality, 5% (myocarditis, encephalitis).
Imaging Features
Esophagus
- •
Early findings: hypercontractility, distal muscular spasm; normal caliber
- •
Classic late findings (denervation): megaesophagus, aperistalsis, bird’s beak appearance at GEJ (achalasia lookalike)
- •
Esophageal complications:
Ulcers, hemorrhage
Perforation into mediastinum, abscess formation; carcinoma, 7%
- •
Colon
- •
Megacolon (anal sphincter neuropathy)
- •
Sigmoid volvulus, 10%
- •
Heart
- •
Cardiomyopathy (cardiomegaly)
- •
Clear lungs, no pericardial effusions
- •
Central nervous system (CNS)
- •
Encephalitis
- •
Benign Esophageal Neoplasm
- •
Leiomyoma (may calcify) 50%
- •
Fibrovascular polyp (may be large and mobile attached to upper esophagus and may contain fat on computed tomography [CT]), 25%
- •
Cysts, 10%
- •
Papilloma, 3%
- •
Fibroma, 3%
- •
Hemangioma, 2%
Malignant Esophageal Neoplasm
Types
- •
Squamous cell carcinoma (SCC; most common worldwide)
- •
Adenocarcinoma, usually in distal esophagus at GEJ (in the United States, the incidence is now higher than SCC)
- •
Lymphoma
- •
Leiomyosarcoma
- •
Metastasis
Associations
SCCs are associated with:
- •
Head and neck cancers
- •
Smoking
- •
Alcohol
- •
Achalasia
- •
Lye ingestion
- •
Adenocarcinoma is associated with:
- •
Barrett esophagus
- •
Gastroesophageal reflux disease (GERD)
- •
Obesity (probably because of the link with GERD)
- •
Imaging Features ( Fig. 3.14 )
Staging (CT)
- •
Invasion into mediastinum, aorta
- •
Local LN enlargement
- •
Metastases: liver, lung, lymphadenopathy, gastrohepatic ligament
- •
Staging (endoscopic US)
- •
Extension through wall
- •
LN metastases
- •
Spectrum of appearance
- •
Infiltrative, shelf-like margins
- •
Annular, constricting
- •
Polypoid
- •
Ulcerative
- •
Varicoid: does not change in configuration during fluoroscopy in contrast to esophageal varices
- •
Unusual bulky forms: carcinosarcoma, fibrovascular polyp, leiomyosarcoma, metastases
- •

Lymphoma
Because the esophagus and stomach do not normally have lymphocytes, primary lymphoma is rare unless present from inflammation. Secondary metastatic lymphoma is more common. Secondary esophageal lymphoma accounts for <2% of all gastrointestinal (GI) tract lymphomas (stomach > SB). Four radiographic presentations are infiltrative, ulcerating, polypoid, and endoexophytic.
Esophageal Foreign Body
Imaging Features
- •
Foreign body usually lodges in coronal orientation.
- •
It is important to exclude underlying Schatzki ring or esophageal carcinoma once the foreign body is removed.
Stomach
Types of Barium Studies
| Single Contrast | Double Contrast | |
|---|---|---|
| Contrast agent | Thin barium (40% w/w) | Thick barium (85% w/w) |
| Effervescent granules | ||
| Differences | Opaque distention Compression is necessary to allow penetration of beam | Translucent distention (“see-through”) Compression less important |
| Fluoroscopy emphasized | Filming emphasized | |
| Indication | Acute setting, uncooperative patient, obstruction | All elective barium studies |
Upper Gastrointestinal (UGI) Series
Patient Preparation
- •
Nothing by mouth for 8 hours before examination
- •
If a BE has been performed within the past 48 hours, give 4 tablespoons of Milk of Magnesia 12 hours before examination (cathartic).
Single-Contrast Technique ( Fig. 3.15 )
- 1.
Patient is in upright position and drinks thin barium. Spot GEJ.
- 2.
Prone position to observe esophageal motility. Spot GEJ, antrum, and bulb.
- 3.
Turn supine under fluoroscopic control.
- 4.
Turn left posterior oblique (LPO) for air contrast of antrum, bulb. Evaluate duodenum and proximal SB.
- 5.
Overhead radiographs: LPO, right anterior oblique (RAO) of stomach, PA of abdomen

Double-Contrast Technique
- 1.
Patient upright in slight LPO position. Administer effervescent granules with 20 mL of water. Start patient drinking thick barium (120 mL) and obtain air-contrast spot radiographs of esophagus.
- 2.
Table down with patient in prone position (compression view may be obtained here). Patient rolls to supine position through the left side. Check mucosal coating: if not adequate, turn patient to prone again and back to supine position, roll to keep left side dependent (so that emptying of barium into the duodenum is delayed).
- 3.
Obtain views of the stomach. This is generally the most important part of the study. The patient is turned to get air into different regions of the stomach.
- •
Patient supine (for body of stomach)
- •
Patient LPO (for antrum)
- •
Patient RPO (for Schatzki view for lesser curvature)
- •
Patient RAO (for fundus)
- •
- 4.
Views of bulb in contrast and gas relief. First leave the patient in RAO view and then turn to LPO view. Include some C-loop.
- 5.
Study of esophagus. Patient RAO drinking regular “thin” barium. Observe entire esophagus and evaluate motility. Take spot radiographs (routinely of distended GEJ).
- 6.
Overhead radiographs (optional):
- •
RAO, drinking esophagus
- •
AP of abdomen
- •
LPO and RAO stomach
- •
- 7.
Water-siphon test to exclude GE reflux, unless small-bowel follow-through (SBFT) is simultaneously scheduled then done at end after swallowing additional barium
Percutaneous Gastrostomy
Success rate 95%, minor complications 1%–2%, and major complications 2%–4%.
Indications
- •
Decompression in terminally ill patients with gastric outlet or small bowel obstruction (SBO): gastrostomy is sufficient.
- •
Feeding: gastrojejunostomy preferred
Technique
- 1.
Half cup of barium the night before to opacify colon. NG tube placement.
- 2.
Mark liver edge under US.
- 3.
Distend stomach by insufflating air through NG tube; mark entry high in midbody pointing toward pylorus, avoid marked colon and opacified bowel.
- 4.
Anesthetic through four 25-gauge needles 1–2 cm away from insertion point. Leave needles in.
- 5.
Gastropexy with T-tacks. Deploy them with 0.35-in ring wire under fluoroscopic guidance. Crimp T-tacks in place.
- 6.
Place needle with guidewire into stomach through central insertion point.
- 7.
Dilators 8, 10, 12, 14 Fr; place 15-Fr peel-away sheath.
- 8.
Place 14-Fr gastrostomy catheter (e.g., Cook). Gastric decompression can be achieved with smaller-bore catheters (>10 Fr). Secure catheter in place.
Contraindications
- •
Organs overlying stomach: liver, colon, ribs (high position of stomach)
- •
Massive ascites (perform therapeutic paracentesis before gastrostomy)
- •
Abnormal gastric wall (ulcer, tumor): hemorrhage is common.
- •
Elevated bleeding time
Normal Appearance
Anatomy ( Fig. 3.16 )
- •
Fundus
- •
Body
- •
Antrum
- •
Pylorus
- •
Curvatures: lesser, greater

Mucosal Relief
- •
Gastric rugae (prominent in body, proximal antrum): in double-contrast studies, rugae are more often effaced by gaseous distention.
- •
Area gastricae (normal gastric mucosal pattern) is most prominent in antrum and body; ectopic duodenal area gastricae is present in 20%.
Types of Gastric Lesions
There are three morphologic types of lesions:
- •
Ulcer: abnormal accumulation of contrast media
- •
Polypoid lesion (masses): filling defect
- •
Coexistent pattern: ulcerated mass
- •
The above lesions have different appearances depending on whether they are imaged with single- or double-contrast techniques, whether they exist on dependent or nondependent walls, and whether they are imaged in profile or en face.
Mucosal Versus Extramucosal Location of Mass ( Fig. 3.17 )
The location of a lesion can be evaluated by observing the angle the lesion forms with the wall:
Acute angle (looks like an a ): mucosal (polyp, cancer)
Obtuse angle (looks like an o ): extramucosal (intramural or extramural)
Preservation of mucosal pattern is also a hint to location of lesions:
- •
Disruption of normal pattern: mucosal
- •
Presence of normal pattern: intramural or extramural location
- •
Distinction of outline:
- •
Smooth, distinct: extramucosal
- •
Irregular, fuzzy: mucosal
- •

Peptic Ulcer Disease (PUD)
Cause
Helicobacter pylori (gram negative) plays a major role in the development of peptic ulcer.
- •
Not all individuals with H. pylori will develop ulcers. Prevalence of H. pylori: 10% of population <30 years, 60% of population >60 years.
- •
Prevalence of H. pylori in duodenal and gastric ulcers: 80%–90%; risk factor for adenocarcinoma and lymphoma
- •
Approach:
Precaution against infection should be taken by all GI personnel.
H. pylori serology may become useful for diagnosis of PUD.
PUD heals faster with antibiotics and antacids than with antacids alone.
- •
Incidence markedly decreased
- •
Detection
Detection rate of ulcers by double-contrast barium is 60%–80%.
Imaging Features ( Fig. 3.18 )
- •
Ulcer crater seen en face: distinct collection of barium that persists on different views; the collection is most often round but can be linear.
- •
Ulcer crater seen in profile: barium collection extends outside the projected margin of the gastric or duodenal wall.
- •
Double-contrast studies: the crater has a white center with surrounding black “collar.”
- •
Greater curvature ulcers are commonly because of malignancy or nonsteroidal antiinflammatory drug (NSAID) ingestion. (Aspirin-induced ulcers are also called sump ulcers because of their typical location on greater curvature.)
- •
Multiple ulcers are usually due to NSAID ingestion.
- •
Signs of benign and malignant ulcers
| Parameter | Benign Ulcer | Malignant Ulcer |
|---|---|---|
| Mucosal folds | Thin, regular, extend up to crater edge | Thick, irregular, do not extend through collar |
| Penetration | Margin of ulcer crater extends beyond projected luminal surface | Ulcers project within (projected) luminal surface; Carman (meniscus) sign a |
| Location | Centrally within mound of edema | Eccentrically in tumor mound |
| Collar | Hampton line: 1–2-mm lucent line around the ulcer b | Thick, nodular, irregular |
| Other | Normal peristalsis | Limited peristalsis |
| Incisura: invagination of opposite wall | Limited distensibility | |
| Gastrohepatic lymph nodes | Occasional | Common |
a Results from the fluoroscopically induced apposition of rolled halves of the tumor margin forming the periphery of the ulcerated carcinoma; meniscus refers to meniscoid shape of ulcer.
b This line is caused by thin mucosa overhanging the crater mouth seen in tangent; it is a reliable sign of a benign ulcer, but present in very few patients.

Gastritis (95% of All Ulcers)
Symptoms Mimic PUD
Causes
- •
NSAIDs
- •
H. pylori
- •
Alcohol
- •
Imaging Features
- •
Multiple tiny, aphthoid-like erosions throughout antrum, body
- •
Occurs on rugal folds
- •
Prominent area gastricae
Treatment
- •
Identify and treat causal agent
- •
H2 blockers
Malignant Ulcers (5% of All Ulcers)
- •
Carcinoma, 90%
- •
Lymphoma, 5%
- •
Rare malignancies (sarcoma, carcinoid, metastases)
Complications of Gastric Ulcer ( Fig. 3.19 )
- •
Obstruction
- •
Posterior penetration of ulcer into pancreas
- •
Perforation
- •
Bleeding: filling defect in the ulcer crater may represent blood clots.
- •
Gastroduodenal fistulas: double-channel pylorus

Pearls
- •
Categorize all gastric ulcers as definitely/probably benign or malignant.
- •
All patients, except for those with de novo definitely benign gastric ulcers, should proceed to endoscopy with biopsy.
- •
Benign ulcers decrease 50% in size within 3 weeks and show complete healing within 6 weeks with successful medical treatment.
- •
Benign ulcers may heal with local scarring.
- •
Ectopic pancreatic rest may contain a central umbilication that represents a rudimentary duct, not ulcer. Commonly located in antrum.
- •
Gastric diverticulum: commonly in posterior fundus; contains mucosal folds, neck, changes shape during fluoroscopy
Ménétrier Disease (Giant Hypertrophic Gastritis)
Large gastric rugal folds (hypertrophic gastritis) with protein-losing enteropathy. Clinical triad: achlorhydria, hypoproteinemia, edema. Typically occurs in middle-aged men. Complication: gastric carcinoma, 10%.
Imaging Features
- •
Giant gastric rugal folds, usually proximal half of stomach
- •
Hypersecretion: poor coating, dilution of barium
- •
Gastric wall thickening
- •
Small intestinal fold thickening because of hypoproteinemia
- •
Peptic ulcers are uncommon
Eosinophilic Gastroenteritis
Inflammatory disease of unknown cause characterized by focal or diffuse eosinophilic infiltration of the GI tract. An allergic or immunologic disorder is suspected because 50% of patients have another allergic disease (asthma, allergic rhinitis, hay fever). Only 300 cases have been reported to date. Treatment is with steroids.
Clinical Findings
- •
Abdominal pain, 90%
- •
Diarrhea, 40%
- •
Eosinophilia
Imaging Features
Stomach, 50%
- •
Tapered antral stenosis (common)
- •
Pyloric stenosis (common)
- •
Gastric fold thickening
- •
SB, 50%
- •
Fold thickening (common)
- •
Dilatation
- •
Luminal narrowing
- •
Gastroduodenal Crohn Disease
- •
Aphthous ulcers, usually in antrum and duodenum
- •
Stricture: Pseudo-Billroth I appearance on barium studies
- •
Fistulization
Zollinger-Ellison Syndrome
Syndrome caused by excessive gastrin production.
Clinical Findings
- •
Diarrhea
- •
Recurrent PUD
- •
Pain
Causes
Gastrinoma, 90%
- •
Islet cell tumor in pancreas or duodenal wall, 90%
- •
50% of tumors are malignant
- •
10% of tumors are associated with multiple endocrine neoplasia (MEN) type I
- •
Antral G-cell hyperplasia, 10%
Imaging Features
- •
Ulcers
Location: duodenal bulb > stomach > postbulbar duodenum
Multiple ulcers, 10%
- •
Thickened gastric and duodenal folds
- •
Increased gastric secretions
- •
Reflux esophagitis
Gastric Polyps
Gastric polyps are far less common than colonic polyps (2% of all patients with polyps).
- •
Hyperplastic polyps (80% of all gastric polyps; <1 cm, sessile; not premalignant)
Associated with chronic atrophic gastritis
Familial adenomatous polyposis (hyperplastic polyps in stomach, adenomatous polyps in colon)
Typically, similar size, multiple, and clustered in the fundus and body
Synchronous gastric carcinoma in 5%–25% of patients
- •
Adenomatous polyps; infrequent, malignant degeneration very rare
Solitary
Malignant transformation in 50%
Villous polyps (uncommon; cauliflower-like, sessile); strong malignant potential
Hamartomatous polyps rare; Peutz-Jeghers; Cronkhite-Canada syndrome, juvenile polyposis
Gastric Carcinoma
Fourth most common GI malignancy (colon > pancreas > liver/biliary > stomach)
Risk Factors
- •
Pernicious anemia
- •
Adenomatous polyps
- •
Chronic atrophic gastritis
- •
Billroth II > Billroth I
Location
- •
Fundus/cardia, 40%
- •
Antrum, 30%
- •
Body, 30%
Staging
- •
T1: Limited to mucosa, submucosa (5-year survival, 85%)
- •
T2: Muscle, serosa involved (5-year survival, 50%)
- •
T3: Penetration through serosa
- •
T4: Adjacent organs invaded
Imaging Features ( Fig. 3.20 )
Features of early gastric cancers:
- •
Polypoid lesions (type 1)
>0.5 cm (normal peristalsis does not pass through lesion)
Difficult to detect radiographically
- •
Superficial lesions (type 2)
2A: <0.5 cm
2B: most difficult to diagnose (mucosal irregularity only)
2C: 75% of all gastric carcinoma (folds tend to stop abruptly at lesion)
- •
Excavated lesion (type 3) = malignant ulcer

Features of advanced gastric cancer:
- •
Malignant ulcer: folds short of collar
- •
Ulcerated luminal mass
- •
Rigidity, diffuse narrowing: linitis plastica
- •
Thickened wall >1 cm by CT
- •
Lymphadenopathy
Gastrohepatic ligament
Gastrocolic ligament
Perigastric nodes
- •
Hepatic metastases
Gastric Lymphoma
Three percent of all gastric malignancies. Non-Hodgkin lymphoma (NHL) (common) > Hodgkin lymphoma (uncommon)
- •
Primary gastric lymphoma (arises from lymphatic tissue in lamina propria mucosae), 10%. Usually originates from mucosa associated lymphoid tissue (MALT lymphoma)
- •
Secondary (gastric involvement in generalized lymphoma), 90%
Risk Factors
- •
H. pylori infection
- •
Inflammatory bowel disease (IBD)
- •
Celiac disease
Imaging Features
- •
Diffuse infiltrating disease
- •
Normal gastric wall 2–5 mm (distended stomach) ≥6 mm is abnormal except at GEJ
- •
Thick folds
- •
Ulcerating mass
- •
More often than carcinoma, lymphomas spread across the pylorus into the duodenum.
- •
Hodgkin lymphoma of the stomach mimics scirrhous carcinoma (strong desmoplastic reaction).
- •
Gastrointestinal Stromal Tumor (GIST)
GIST is the most common mesenchymal neoplasm of the GI tract and is defined by its expression of KIT (CD117), a tyrosine kinase growth factor receptor. The expression of KIT is important, as it distinguishes GIST from other mesenchymal neoplasms such as leiomyomas, leiomyosarcomas, schwannomas, and neurofibromas. Pharmacologically targeting this receptor with a KIT tyrosine kinase inhibitor (STI-571, imatinib, Gleevec) has been shown to be of clinical use. In the stomach, small intestine, colon, and anorectum, GIST accounts for almost all mesenchymal tumors, because leiomyomas and leiomyosarcomas in these sites are very rare. GIST most frequently occurs in the stomach (70% of cases), followed by the small intestine (20%–30%), anorectum (7%), colon, and esophagus. Patients with neurofibromatosis type 1 (NF1) have an increased prevalence of GIST, often multiple small GISTs.
Imaging Features
- •
Exophytic masses of stomach or SB that may ulcerate; obstruction rare despite size
- •
Heterogeneous contrast enhancement
- •
Crescent-shaped necrosis (Torricelli-Bernoulli sign) in large GIST
- •
30% show aneurysmal dilation of enteric bowel.
- •
Liver is the most common site of metastases, followed by mesentery.
- •
Mesenteric metastases are smooth and multiple.
- •
Lymphadenopathy not common; if lymphadenopathy is present, consider alternate diagnosis of lymphoma.
- •
Good response to Gleevec (competitively binds to ATP binding site of tyrosine kinase, leading to cell death by apoptosis; areas of apoptosis appear as cystic spaces on CT or magnetic resonance imaging [MRI])
- •
positron emission tomography (PET) is a sensitive modality for follow-up of patients on therapy.
Metastases
Contiguous Spread
- •
From colon (gastrocolic, gastrosplenic ligament)
- •
From liver (gastrohepatic ligament)
- •
From pancreas: direct invasion
Hematogenous Spread to Stomach (Target Lesions)
- •
Melanoma (most common)
- •
Breast
- •
Lung
Imaging Features
- •
Diffuse uniform thickening, nondistensible, absent gastric folds, linitis plastica
- •
Multiple lesions with bull’s eye appearance: sharply demarcated with central ulcer (much bigger than aphthoid ulcer)
Carney Triad (Rare)
- •
Gastric leiomyosarcoma
- •
Functioning extraadrenal paraganglioma
- •
Pulmonary chondroma
Benign Tumors
Benign tumors are usually submucosal.
- •
Leiomyoma: most common benign tumor; may ulcerate, 10% malignant
- •
Lipoma, fibroma, schwannoma, hemangioma, lymphangioma
- •
Carcinoid (malignant transformation in 20%)
- •
Gastric Volvulus
Abnormal rotation of stomach. Two types ( Fig. 3.21 ):
Organoaxial
- •
Rotation around the long axis of stomach
- •
Stomach rotates 180 degrees so that greater curvature is cranially located; upside-down stomach
- •
Observed in adults with large hiatal hernia
- •
Complications rare
- •
Mesenteroaxial
- •
Stomach rotates around its short axis (perpendicular to long axis)
- •
Fundus is caudal to antrum
- •
More common when large portions of stomach are above diaphragm (traumatic diaphragmatic rupture in children)
- •
Obstruction, ischemia likely
- •

FIG. 3.21
Gastric Varices
Gastric varices represent dilated peripheral branches of short gastric and left gastric veins and appear as serpentine, nodular folds in body or fundus or as polypoid filling defects in the fundus.
Gastric varices are commonly associated with esophageal varices; the combination is often due to portal hypertension.
Gastric varices without esophageal varices are often caused by splenic vein obstruction and are most commonly secondary to pancreatitis or pancreatic carcinoma.
Benign Gastric Emphysema
Gas in wall of stomach is usually due to:
- •
Trauma from endoscopy, infection, ischemia, increased intraluminal pressure, vomiting, spontaneous or traumatic rupture of a pulmonary bulla into areolar tissue surrounding the esophagus
- •
No discernible underlying disease
- •
Duodenum and Small Bowel
Duodenum
Normal Appearance
The duodenum has four segments ( Fig. 3.22 ):
Segment I
- •
Begins at pylorus and extends to the superior duodenal flexure
- •
Contains the duodenal bulb
- •
Intraperitoneal position: freely mobile
- •
Segment II
- •
Begins at superior duodenal flexure and extends to inferior duodenal flexure
- •
Contains the major and minor papilla and the promontory
- •
Fixed retroperitoneal position
- •
Segment III
- •
Extends from inferior duodenal flexure transversely, crossing the midline
- •
Fixed retroperitoneal position
- •
Segment IV
- •
Extends superiorly to the ligament of Treitz
- •
Fixed retroperitoneal position
- •

FIG. 3.22
Mucosal Relief
- •
Folds in the duodenal bulb are longitudinally oriented.
- •
In the descending portion of the duodenum, Kerkring folds are transversely oriented.
- •
These folds are usually visible despite complete duodenal distention.
Papilla ( Fig. 3.23 )
Major papilla (Vater papilla): orifice for ducts
- •
Appears as round filling defect
- •
Located below the promontory
- •
8–10 mm in length
- •
Abnormal if >15 mm
- •
Minor papilla (accessory papilla, Santorini papilla)
- •
Located superiorly and ventral to major papilla
- •
Mean distance from major papilla 20 mm
- •
Not usually visualized
- •
Promontory:
- •
Shoulder-like luminal projection along medial aspect of the second portion of the duodenum
- •
Begins superior to major papilla
- •

Duodenal Ulcer ( Fig. 3.24 )
Duodenal ulcers are two to three times more common than gastric ulcers. All bulbar duodenal ulcers are considered benign. Postbulbar or multiple ulcers raise the suspicion for Zollinger-Ellison syndrome.
Bulbar, 95%
- •
Anterior wall: most common site, perforate
- •
Posterior wall: penetration into pancreas
- •
Postbulbar, 5%

Predisposing Factors
- •
Chronic obstructive pulmonary disease (COPD)
- •
Severe stress: injury, surgery, burn
- •
Steroids
Imaging Features
- •
Persistent round or elliptical collection; radiating folds, spasm
- •
Linear ulcers, 25%
- •
Kissing ulcers: 2 or more ulcers located opposite each other
- •
Giant ulcers
Crater is >2 cm.
Ulcer largely replaces the duodenal bulb.
A large ulcer crater may be mistaken for a deformed bulb but does not change shape during fluoroscopy.
- •
Duodenal ulcers often heal with a scar; this can lead to deformity and contraction of the duodenal bulb: cloverleaf deformity, or hourglass deformity.
- •
Postbulbar ulcers: any ulcer distal to the first portion of the duodenum should be considered to have underlying malignancy until proved otherwise (only 5% are benign ulcers, mostly secondary to Zollinger-Ellison syndrome).
Duodenal Trauma
Duodenal injuries are due either to penetrating (stab, gunshot) wounds or to blunt trauma (motor vehicle accident). Because the duodenum is immobile in retroperitoneum, most perforations occur there. Mortality of untreated duodenal rupture is 65%.
Location of Intestinal Trauma
- •
Duodenum/proximal jejunum, 95%
- •
Colon, 5%
Types of Injuries
- •
Perforation (requires surgery)
- •
Transection (requires surgery)
- •
Hematoma (nonsurgical treatment)
| Blunt Trauma (%) | Penetrating Trauma (%) | |
|---|---|---|
| Liver | 30 | 55 |
| Pancreas | 45 | 35 |
| Spleen | 25 | 2 |
| Colon | 15 | 10 |
| Small bowel | 10 | 25 |
| Kidney | 10 | 20 |
Imaging Features
Perforation:
- •
Extraluminal retroperitoneal gas
- •
Extravasation of oral contrast material
- •
Perforation or hematoma:
- •
Thickening of duodenal wall or high-density mass (clotted blood) can narrow the lumen
- •
Fluid in right anterior pararenal space or in the peritoneum
- •
Duodenal diverticula commonly project into head or uncinate process of pancreas and rarely present coming from lateral wall.
- •
Surgical Treatment
- •
Simple repair
- •
Pyloric exclusion for complex injuries
- •
Whipple procedure is rarely necessary.
- •
Surgical complications:
Intraabdominal abscess, 15%
Duodenal fistula, 4%
Duodenal dehiscence, 4%
Pancreatic fistula, 1%
Benign Tumors
More common than malignant duodenal tumors.
Types
- •
Lipoma, leiomyoma (most common)
- •
Villous adenoma (cauliflower-like), adenomatous polyp
- •
Lymphoid hyperplasia
- •
Heterotopic gastric mucosa: small angular filling defects in bulb, larger than nodules of lymphoid hyperplasia and smaller than Brunner gland hyperplasia
- •
Brunner gland hyperplasia
- •
Ectopic pancreas
Antral Mucosal Prolapse
Anatomic variant characterized by movement of gastric mucosa bulging into the base of the duodenal bulb. No pathophysiologic significance.
Imaging Features
- •
Lobulated stellate filling defect in the duodenal bulb
- •
Filling defect in contiguity with antral rugal folds
Malignant Tumors
Infrequent. The most common locations of malignant tumors are in the periampullary and infraampullary areas.
Types
- •
Adenocarcinoma (most common)
- •
Leiomyosarcoma
- •
Lymphoma
- •
Metastases
- •
Benign tumors with malignant potential: villous and adenomatous polyps, carcinoid
Upper Gastrointestinal (GI) Surgery
Complications of Surgery ( Fig. 3.25 )
Immediate complications:
- •
Anastomotic leak
- •
Abscess
- •
Gastric outlet obstruction (edema)
- •
Bile reflux gastritis
- •
Ileus
- •
Late complications:
- •
Bowel dysmotility: dumping, postvagotomy hypotonia
- •
Ulcer
- •
Bowel obstruction: outlet obstruction, adhesions, stricture
- •
Prolapse, intussusception
- •
Gastric carcinoma (in 5% of patients 15 years after surgery), Billroth II > Billroth I
- •
Metabolic effects: malabsorption
- •
Afferent loop syndrome
- •
Small pouch syndrome
- •
| Type | Anastomosis/Surgery | Common Indication |
|---|---|---|
| Antireflux | Fundoplication (Nissen, Toupet, Belsey Mark IV)
| Prevention of gastroesophageal reflux |
| Gastrectomy ( Fig. 3.26A ) | Gastroduodenostomy (Billroth I) | Gastroduodenal ulcer |
| Gastrojejunostomy (Billroth II) | Gastroduodenal ulcer | |
| Total gastrectomy | Gastric cancer | |
| Vagotomy ( Fig. 3.26B ) | Truncal vagotomy Selective vagotomy | |
| Parietal cell vagotomy | ||
| Drainage procedures | Facilitate gastric emptying after vagotomy | |
| Gastroenterostomy | ||
| Palliative curative | Pancreaticoduodenectomy (Whipple)
| Pancreatic cancer |



Bariatric Surgery
Numerous bariatric surgical procedures exist, the most common is now the sleeve gastrectomy. This procedure recently supplanted the Roux-en-Y gastric bypass as the most popular bariatric surgery. Roux-en-Y gastric bypass is still the preferred method to treat obesity in patients with diabetes.
Gastric Bypass ( Fig. 3.27 )
In gastric bypass surgery, a small gastric pouch (<30 mL) and a small gastrojejunostomy (<12 mm) are constructed (Roux-en-Y gastric bypass procedure). The remaining stomach is intact but functionally separate from food pathway. Currently, the Roux-en-Y gastric bypass combines restrictive and malabsorptive properties by creating a small gastric pouch and a Roux limb.

Complications
- •
Narrowing/stenosis
Immediate postsurgical narrowing is common and often subsides
Stenosis (lumen <6 mm) at >6 weeks after surgery is rare. Weight loss can be dramatic.
- •
Anastomotic leak
Incidence of leaks after Roux-en-Y bypass surgery is 1%–6%. More common after laparoscopic than open surgery.
The leak is commonly at the gastrojejunal anastomosis or at the enteroenteric anastomosis (both are life threatening).
Contrast material outside the confines of the gastric pouch and anastomosis indicates a leak. Although leaks from the enteroenteric anastomosis are rapidly clinically evident and severe, they are usually not diagnosed radiographically.
Immediate surgical exploration is needed.
- •
Fistula
During surgery, the gastric pouch and remnant are surgically separated. Oral contrast should not directly enter the gastric remnant. The presence of oral contrast in the remnant thus indicates a gastro-gastric fistula.
Contrast may be seen in excluded stomach on SBFT by retrograde filling through the duodenum.
- •
Internal hernia: The most common herniation is the transmesenteric (or transmesocolonic) type, which occurs through the defect in the transverse mesocolon. The herniated bowel is usually the Roux limb itself with a varying amount of additional SB loops.
CT findings:
Abnormal position of distended SB loops anterior to the pancreas and above the transverse colon; obstruction
Inferior displacement of the transverse colon
Crowding, engorgement, and deviation of mesenteric vessels
The transition point is proximal to the jejunojejunostomy.
- •
Hernias may also occur in the SB mesenteric defect at the jejunojejunostomy site and in the space posterior to the Roux limb (Peterson type).
- •
Weight gain
Degradation of pouch restriction: very rapid passage of contrast through a patulous anastomosis degrades the restrictive properties of the laparoscopic Roux-en-Y gastric bypass, resulting in weight gain.
Gastrogastric fistula: although uncommon, a fistulous tract arising from the pouch may opacify the excluded stomach and is thought to be a result of patient overeating.
Adjustable Gastric Banding
An adjustable band is laparoscopically placed around the proximal stomach, creating a small upper pouch 2 cm distal to the GEJ. The cuff is connected to a reservoir placed in the anterior rectus sheath or subcutaneous tissues. The reservoir allows adjustment of band diameter percutaneously. The angle of the cuff with the spinal column (Phi angle) should be 4–58 degrees on plain radiographs.
Complications
- •
Band placed too low in stomach
- •
Band not placed around stomach
- •
Band placed around esophagus, which is undesirable because sensation of satiety lacking and risk of perforation
- •
Slippage of the band with upward herniation of stomach (late complication).
Sleeve Gastrectomy
Left side (greater curvature and fundus) of stomach is surgically removed laparoscopically after staples are placed from the angle of His (angle formed as lateral border of esophagus meets the medial border of fundus) and the pylorus.
Jejunum and Ileum
Normal Appearance
The SB can be examined by conventional SBFT, enteroclysis, CT, CT enteroclysis (the former two procedures are most common), MR, or MR enteroclysis. The specific indications for enteroclysis are:
- •
Occult bleeding
- •
Recurrent obstructive symptoms
- •
Malabsorption
- •
To determine extent of Crohn disease
Normal Appearance of SB by SBFT
Luminal diameter
- •
>3 cm is abnormal
- •
Fold thickness
- •
Valvulae conniventes measure 1–2 mm; more prominent in jejunum than ileum
- •
>3 mm is abnormal
- •
Wall thickness
- •
Normal is 1–1.5 mm
- •
Secretions
- •
There should normally be no appreciable fluid in SB.
- •
Excess secretions cause dilution of barium column.
- •
Computed Tomography
- •
Normal wall thickness: 1–1.5 mm
- •
Incomplete distention or luminal fluid may mimic abnormally thick wall; look for antidependent luminal gas collections to better assess wall thickness.
Jejunal and Ileal Diverticuli
Jejunal and ileal outpouchings may predispose to bacterial overgrowth, vitamin B 12 deficiency, and megoblastic anemia.
Blind Loop Syndrome
Syndrome develops after bypassing SB by an enteroanastomosis with subsequent stagnation of bowel contents. Malabsorption in large diverticula may cause similar dynamics.
Malabsorption
Abnormal absorption of fat, water, protein, and carbohydrates from SB.
Imaging Features
- •
Dilatation of bowel loops
- •
Diluted barium (mixes with watery bowel content)
- •
Flocculated barium: barium aggregates into particles (mainly seen with older barium suspensions)
- •
Slow transit
- •
Segmentation of barium (lack of continuous column) rarely occurs with new agents
- •
Moulage pattern: featureless barium collection (rarely occurs with new agents)
- •
Hidebound pattern: valvulae thinner, closer together, wrinkled look
- •
Many of these features may no longer be seen with newer barium products.
Sprue
Three entities:
- •
Tropical sprue (unknown cause; responds to antibiotics)
- •
Nontropical (adults; intolerance to gluten in wheat and other grains; HLA-DR3, IgA, IgM antibodies)
- •
Celiac disease (children)
- •
Imaging Features
- •
Dilatation of SB is the most typical finding (caliber increases with severity of disease).
- •
Nodular changes in duodenum (bubbly duodenum)
- •
Reversal of jejunal and ileal fold patterns: “The jejunum looks like the ileum, the ileum looks like the jejunum, and the duodenum looks like hell.”
- •
Segmentation
- •
Hypersecretion and mucosal atrophy cause the moulage sign (rare).
- •
Transient intussusception pattern (coiled spring) is typical.
- •
Increased secretions: flocculation with older barium suspensions
- •
Increased incidence of malignancy, aggressive lymphoma, carcinoma
Associated Disorders
- •
Dermatitis herpetiformis
- •
Selective IgA deficiency
- •
Hyposplenism
- •
Adenopathy
- •
Cavitary mesenteric LN syndrome
Complications
- •
Ulcerative jejunoileitis: several segments of bowel wall thickening with irregularity and ulceration strictures may follow
- •
Enteropathy: associated T-cell lymphoma
- •
Increased incidence of cancers of esophagus, pharynx, duodenum, and rectum
- •
Sprue, SBO, scleroderma (SOS): dilated, prolonged motility, normal folds
| Disease | Primary Pattern | Comment |
|---|---|---|
| Scleroderma | AM + D, hidebound folds | Muscularis replaced by fibrosis |
| Whipple | DFTN, adenopathy may occur | Intestinal lipodystrophy |
| Amyloidosis | DFTN | Tiny nodule filling defects |
| Lymphangiectasia | DFTN, MA | Dilated lymphatics in wall |
| Ig deficiencies | DFTN | Nodular lymphoid hyperplasia |
| Mastocytosis | DFTN | Hepatomegaly, PUD, dense bones |
| Eosinophilic gastroenteritis | Very thick folds (polypoid) | Food allergy, 70% |
| Graft-versus-host disease | Effaced folds (ribbon like) | Bone marrow transplants |
| MAI infection | DFTN, MA, pseudo-Whipple | Immunocompromised host |
a See also Infectious Enteritis .
Mastocytosis
Systemic mast cell proliferation in reticuloendothelial system (RES) (SB, liver, spleen, LNs, bone marrow) and skin (95%) with histamine release.
Clinical Findings
- •
Diarrhea
- •
Steatorrhea
- •
Histamine effects (flushing, tachycardia, pruritus, PUD)
Imaging Features
SB
- •
Irregular fold thickening
- •
Diffuse small nodules
- •
Other
- •
Sclerotic bone lesions
- •
Hepatosplenomegaly
- •
Peptic ulcers (increased hydrochloric acid [HCl] secretion)
- •
Amyloidosis
Heterogeneous group of disorders characterized by abnormal extracellular deposition of insoluble fibrillar protein material. Diagnosis is established by biopsy of affected organs (birefringence, staining with Congo red). Clinical amyloidosis syndromes include:
Systemic amyloidosis
- •
Immunocyte dyscrasia (myeloma, monoclonal gammopathy)
- •
Chronic/active disease (see below)
- •
Hereditary syndromes
Neuropathic form
Nephropathic form
Cardiomyopathic form
- •
Chronic hemodialysis
- •
Senile form
- •
Localized amyloidosis
- •
Cerebral amyloid angiopathy (Alzheimer disease, senile dementia)
- •
Cutaneous form
- •
Ocular form
- •
Others
- •
Common chronic/active diseases that are associated with systemic amyloidosis (there are many less common causes):
Infections (recurrent and chronic)
- •
Tuberculosis
- •
Chronic osteomyelitis
- •
Decubitus ulcers
- •
Bronchiectasis
- •
Chronic pyelonephritis
- •
Chronic inflammatory disease
- •
Rheumatoid arthritis (5%–20% of cases)
- •
Ankylosing spondylitis
- •
Crohn disease
- •
Reiter syndrome
- •
Psoriasis
- •
Neoplasm
- •
Hodgkin disease (4% of cases)
- •
Renal cell carcinoma (RCC; 3% of cases)
- •
Imaging Features
Kidneys
- •
Nephrotic syndrome
- •
Renal insufficiency
- •
Renal tubular acidosis
- •
Renal vein thrombosis
- •
GI tract
- •
Diffuse thickening of SB folds
- •
Jejunization of ileum
- •
SB dilatation
- •
Multiple nodular filling defects, >2 mm
- •
Hepatosplenomegaly
- •
Macroglossia
- •
Colonic pseudodiverticulosis (may be unilateral and large)
- •
Heart
- •
Cardiomyopathy (restrictive)
- •
Rhythm abnormalities
- •
Nervous system
- •
Signs of dementia
- •
Carpal tunnel syndrome
- •
Peripheral neuropathy
- •
Intestinal Lymphangiectasia
Spectrum of lymphatic abnormality (dilated lymphatics in lamina propria of SB) that clinically results in protein-losing enteropathy.
Congenital (infantile) form presents with:
- •
Generalized lymphedema
- •
Chylous pleural effusions
- •
Diarrhea, steatorrhea
- •
Lymphocytopenia
- •
Acquired (adult) form as a result of:
- •
Obstruction of thoracic duct (radiation, tumors, retroperitoneal fibrosis)
- •
SB lymphoma
- •
Pancreatitis
- •
Imaging Features
- •
Diffuse nodular thickening of folds in jejunum and ileum caused by dilated lymphatics and hypoalbuminemic edema; mesenteric adenopathy on CT
- •
Dilution of contrast material as a result of hypersecretion
- •
Lymphographic studies
Hypoplastic lymphatics of lower extremity
Tortuous thoracic duct
Hypoplastic LNs
GI Lymphoma
Distinct subgroup of lymphoma that primarily arises in lymphoid tissue of the bowel rather than in LNs.
GI lymphoma in otherwise healthy patients:
- •
Gastric lymphoma arising from mucosa-associated lymphoid tissue (MALT)
- •
Usually low-grade malignancy
- •
Represent 20% of malignant SB tumors; usual age: 5th to 6th decade
- •
Imaging features
Mass, nodule, fold thickening (focal or diffuse) confined to GI tract in 50%
Adenopathy, 30%
Extraabdominal findings, 30%
- •
Large ulcerated mass presenting as endoenteric or exoenteric tumor (differential diagnosis [DDX]: GI stromal tumor, metastatic melanoma, jejunal diverticulitis with abscess, ectopic pancreas)
- •
Aneurysmal dilatation: localized dilated, thick-walled, noncontractile lumen because of mural tumor; Auerbach plexus neuropathy
- •
GI lymphoma in HIV-positive or immunosuppressed patients:
- •
Usually aggressive NHL with rapid spread, poor response to chemotherapy, short survival
- •
Widespread extraintestinal involvement, 80%
- •
Imaging features
- •
GI abnormalities: nodules, fold thickening, mass
Splenomegaly, 30%
Adenopathy, 30%
Ascites, 20%
Graft-Versus-Host (GVH) Reaction
Donor lymphocytes react against organs (GI tract, skin, liver) of the recipient after bone marrow transplant. Pathology: granular necrosis of crypt epithelium.
Imaging Features
- •
Classic finding: SB loops, which are too narrow, and featureless margins (ribbon bowel)
- •
Luminal narrowing is due to edema of the bowel wall.
- •
Flattening of mucosal folds (edema)
- •
Prolonged coating of barium for days
Scleroderma
Scleroderma or progressive systemic sclerosis (PSS) is a systemic disease that involves primarily skin, joints, and the GI tract (esophagus > SB > colon > stomach). Age: 30–50 years; female > male.
Imaging Features
SB
- •
Dilation of bowel loops with hypomotility is a key feature.
- •
Mucosal folds are tight and closer together (fibrosis): hidebound appearance.
- •
Pseudosacculations along antimesenteric border, may involve both small and large bowel
- •
Segmentation, fragmentation, hypersecretion are absent.
- •
Other
- •
Dilated dysmotile esophagus, esophagitis, incompetent LES, reflux, stricture
- •
Dilated duodenum and colon (pseudoobstruction)
- •
Pneumatosis cystoids coli (steroid therapy)
- •
Pulmonary interstitial fibrosis
- •
Acroosteolysis
- •
Soft tissue calcification
- •
Whipple Disease
Rare multisystem disease caused by Tropheryma whippelii . Structures primarily involved include SI joints, joint capsule, heart valves, CNS, and jejunum.
Clinical Findings
- •
Middle-aged men, United States, Northern Europe
- •
Diarrhea, steatorrhea
- •
Immune defects
Imaging Features
- •
1–2-mm diffuse micronodules in jejunum
- •
No dilatation or increased secretions
- •
Nodal masses in mesentery (echogenic by US); nodes have low CT density
- •
Sacroiliitis
Enteric Fistulas
Fistulas of SB with adjacent structures can be seen with Crohn disease, colorectal cancer, after surgery, and in diverticular disease.
Types
- •
Enteroenteric: SB → SB
- •
Enterocolonic: SB → colon
- •
Enterocutaneous: SB → skin
- •
Enterovesical: SB → bladder
- •
Enterovaginal: SB → vagina
Radiographic Workup
- •
Fistulogram (enterocutaneous fistula): injection of water-soluble contrast material through small catheter inserted into fistula
- •
UGI and SBFT
- •
Barium enema
Therapy
- •
Total parenteral nutrition to achieve “bowel rest”
- •
Postoperative fistulas usually heal spontaneously with conservative measures.
- •
Fistulas in active Crohn disease usually require excision of diseased bowel.
- •
Cyclosporine and other immunosuppressants have been used to heal fistulas in Crohn disease; more recently monoclonal antibody (infliximab) has been used.
Drug Chemotherapy-Induced Enteritis
- •
Chemotherapeutic agents can induce spontaneous GI edema, necrosis, and even perforation.
- •
Most common in long-term immunosuppressive treatment to prevent homograft rejection or in those receiving long-term chemotherapy for leukemia or lymphoma.
- •
CT findings can be seen in diseased or disease-free intestinal segments.
- •
Chemotherapy-induced enteropathy appears as nonspecific focal or diffuse bowel wall thickening with or without the target sign or as regional mesenteric vascular engorgement and haziness, more often in distal SB.
- •
Angiotensin-converting enzyme (ACE) inhibitors may cause angioedema resulting in reversible wall thickening.
Infectious Enteritis
Cryptosporidiosis
Cryptosporidium species are protozoa that frequently cause enteritis in AIDS patients but rarely in immunocompetent patients. Diagnosis is made by examination of stool or duodenal aspirate.
| Infection | Common Radiographic Patterns |
|---|---|
| Parasites | |
| Hookworms (Necator, Ancylostoma) | TFN |
| Tapeworms | FD |
| Ascaris | FD, intestinal obstruction |
| Infectious ( Fig. 3.28 ) | |
| Yersinia enterocolitica | TFN, ulcers, TI |
| TB | Stricture → obstruction, TI |
| Histoplasmosis | TFN |
| Salmonellosis | TFN, TI |
| Campylobacter | TFN, loss of haustration, TI |
| Common in AIDS | |
| Cytomegalovirus | TF in cecum, pancolitis |
| Tuberculosis | TF in cecum; adenopathy (low central attenuation), TI |
| MAI | TFN, adenopathy (homogeneous) |
| Cryptosporidiosis | TFN |
| Giardiasis | TFN, largely jejunal, jejunal spasm |

Imaging Features
- •
Thickened SB folds
- •
Dilatation of SB
Intestinal Helminths
| Organism (Treatment) | Route | Clinical Findings |
|---|---|---|
| Nematode (Mebendazole) | ||
| Ascaris lumbricoides a | Fecal-oral | Intestinal, biliary obstruction, PIE |
| Ancylostoma duodenale | Skin penetration | Iron-deficiency anemia, PIE |
| Necator americanus | Skin penetration | Iron-deficiency anemia, PIE |
| Strongyloides stercoralis | Skin penetration | Malabsorption, PIE |
| Nematode (Mebendazole) | ||
| Trichuris trichiura | Fecal-oral | Rectal prolapse |
| Enterobius vermicularis | Fecal-oral | |
| Cestode (Praziquantel) | ||
| Beef tapeworm ( Taenia saginata ) | Raw beef | |
| Pork tapeworm ( Taenia solium ) | Raw pork | Cysticercosis: CNS |
| Fish tapeworm | Raw fish | Vitamin B 12 deficiency |
| Dwarf tapeworm | Fecal-oral | Diarrhea |
| Trematode (Praziquantel) | ||
| Heterophyes heterophyes | Raw fish | Diarrhea |
| Metagonimus yokogawai | Raw fish | Diarrhea |
Ascariasis ( Fig. 3.29 )
Infection with Ascaris lumbricoides (roundworm, 15–35 cm long) is the most common parasitic infection worldwide.

Imaging Features
GI tract
- •
Jejunum > ileum, duodenum, stomach
- •
Worms visible on SBFT as longitudinal filling defects
- •
Enteric canal of worm is filled with barium
- •
Worms may cluster: “bolus of worm”
- •
Mechanical SBO
- •
Other complications: perforation, volvulus
- •
Biliary tract
- •
Intermittent biliary obstruction
- •
Granulomatous stricture of bile duct (rare)
- •
Oriental cholangiohepatitis
- •
Carcinoid Tumors
Carcinoid tumors arise from enterochromaffin cells.
Location:
GI tract, 85%
- •
Location: appendix, 50% > SB (33%), gastric, colon and rectum (2%); virtually never occur in esophagus
- •
90% of SB carcinoids arise in distal ileum
- •
30% of SB carcinoids are multiple; 40%–80% of GI tract carcinoids spread to mesentery
- •
Bronchial tree, 15%
- •
90% central, 10% peripheral
- •
Other rare locations
- •
Thyroid
- •
Teratomas (ovarian, testicular)
- •
Symptoms of GI carcinoids:
- •
Asymptomatic, 70%; obstruction, 20%; weight loss, 15%; palpable mass, 15%
- •
Carcinoid Syndrome
Ninety percent of patients with carcinoid syndrome have liver metastases. The tumor produces ACTH, histamine, bradykinin, kallikrein, serotonin (excreted as 5-HIAA in urine), causing:
- •
Recurrent diarrhea, 70%
- •
Right-sided endocardial fibroelastosis → tricuspid insufficiency, pulmonary valvular stenosis (left side of heart is spared because of metabolism by monoamine oxidase inhibitor [MAOI] in lung)
- •
Wheezing, bronchospasm, 15%
- •
Flushing of face and neck
Imaging Features
- •
Mass lesion in SB: filling defect
- •
Strong desmoplastic reaction causes angulation, kinking of bowel loops (tethered appearance), mesenteric venous congestion
- •
Mesenteric mass on CT with spokewheel pattern is virtually pathognomonic; the only other disease that causes this appearance is retractile mesenteritis (very rare).
- •
Stippled calcification in mesenteric mass
- •
Obstruction secondary to desmoplastic reaction
- •
Very vascular tumors (tumor blush at angiography, very hyperintense on T2-weighted [T2W] images)
- •
Liver metastases (arterial phase indicated)
Complications
- •
Ischemia with mesenteric venous compromise
- •
Hemorrhage
- •
Malignant degeneration: gastric and appendiceal tumors rarely metastasize; SB tumors metastasize commonly.
Radiation Enteritis
- •
Damage of SB mucosa and wall as a result of therapeutic radiation
- •
Highest to lowest tolerance: duodenum > jejunum, ileum > transverse colon, sigmoid colon > esophagus and rectum
- •
Tolerance dose (TD 5/5) is the total dose that produces radiation damage in 5% of patients within 5 years; TD 5/5 is 4500 cGy in SB and colon and 5000 cGy in rectum.
- •
Findings: mural thickening and luminal narrowing, usually in pelvic bowel loops, after treatment of gynecologic or urinary bladder cancers
- •
Long-term sequelae: narrowing or stenosis of affected segment; adhesions with angulation between adjacent loops; reduced or absent peristalsis
Ace-Inhibitor–Related Angioedema
- •
Acute onset or recurrent acute abdominal pain
- •
Segmental area of circumferential bowel wall thickening
- •
Decreased submucosal attenuation
- •
Mesenteric edema
- •
Ascites
- •
Engorgement of the vasa recta
Colon
General
Barium Enema
Patient Preparation
- •
Clear liquid diet day before examination
- •
Magnesium citrate, 300 mL, afternoon before examination
- •
50 mL castor oil evening before examination
- •
Cleansing enema morning of examination
Single-Contrast Technique
- 1.
Insert tube with patient in lateral position.
- 2.
Decide if need to inflate balloon for retention; if so, inflate under fluoroscopic control, being sure that balloon is in the rectum.
- 3.
Fluoroscopy as the barium goes in.
- 4.
Patient in supine position (as opposed to double-contrast study). Instill barium just beyond sigmoid colon. Take AP and two oblique spot radiographs of sigmoid.
- 5.
Try to follow head of column fluoroscopically.
- 6.
Take spot views of both splenic flexure and hepatic flexure.
- 7.
Spot cecum and terminal ileum. If a filling defect is encountered, palpate to see if it is sessile or floating.
- 8.
Obtain overhead views and postevacuation radiographs.
Double-Contrast Technique
- 1.
Patient is in lateral position. Insert tube.
- 2.
Patient supine: administer glucagon IV. Turn patient prone: this helps barium flow to the descending colon, decreases pooling in the rectum and sigmoid, and thereby is less uncomfortable. Instill barium beyond the splenic flexure. Stand patient up, bag to the floor, and let barium drain.
- 3.
Place patient in horizontal prone position. Start slow inflation with air and rotate patient toward you into a supine position. Take spot views of the sigmoid in different obliquities (take spots of any air-filled loop). When patient is supine, check to see if barium has already coated the ascending colon.
- 4.
Stand patient up to facilitate coating of ascending colon. Drain as much barium as possible through rectal tube. Insufflate more air.
- 5.
Spot views of splenic and hepatic flexure in upright position. Take spots in slightly different obliquities of both flexures.
- 6.
Patient prone; put table down. Take spot views of the cecum and sigmoid.
- 7.
Obtain overhead views:
AP, PA
Prone, cross-table lateral
Decubitus
Postevacuation radiographs
Contraindications to Barium Enema (BE)
- •
Suspected colonic perforation (use water-soluble iodinated contrast)
- •
Patients at risk for intraperitoneal leakage (use Gastrografin):
Severe colitis
Toxic megacolon (TMC)
Recent deep biopsy
- •
If colonoscopy needs to follow enema; use water-soluble iodinated contrast
- •
Severe recent disease: myocardial infarction, cerebrovascular accident (CVA)
Complications of Barium Enema
- •
Perforation (incidence 1 : 5000), typically caused by overinflation or traumatic insertion of balloon or fragile colonic walls
- •
Appearance of gas in portal venous system in patients with IBD (no significant ill effects)
- •
Allergy to latex tips
Glucagon
Glucagon is a 29–amino acid peptide produced in A cells of the pancreas.
Physiologically, the main stimulus for glucagon release is hunger (hypoglycemia).
Effects:
- •
Antagonist to insulin (increases blood glucose)
- •
Relaxation of smooth muscle cells
- •
Relaxation of gallbladder (GB) sphincter and sphincter of Oddi; increased bile flow
Glucagon is a useful adjunct (0.1–1 mg IV) to barium enema (BE) or whenever smooth muscle spasm is suspected of producing a “pseudostenotic lesion.” Thus it can be used in evaluation of the esophagus, stomach, duodenum, small intestine, common bile duct (CBD), and colon.
Contraindications include:
- •
Pheochromocytoma
- •
Insulinoma
- •
Glaucoma
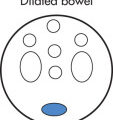
CT Colonography (CTC)
- •
Replacing DCBE for detecting and screening of colonic neoplasms.
- •
Helically acquired axial images of the gas-distended colon are obtained during breath holding in both prone and supine positions.
- •
Images are combined into a detailed model of the colon subsequently viewed using either 2D multiplanar reconstructions or primary 3D endoluminal display.
- •
Standard examination does not require IV contrast and uses extremely low dose x-ray technique, typically 20% radiation of standard diagnostic CT, and approximately 10% less than double-contrast barium enema.
- •
Detection of large polyps (>10 mm) is comparable with optical colonoscopy (OC); detection of polyps 6–9 mm approximately equal to OC; detection of polyps <6 mm, OC is superior.
- •
Studies using latest techniques (primary 3D visualization, fecal tagging) demonstrate sensitivity of 92% for polyps >10 mm; per patient specificity 96%
- •
Currently requires cathartic bowel preparation similar to that for fiberoptic colonoscopy
Magnetic Resonance Enterography (MRE)
- •
Performed to evaluate the small and large bowel in patients with IBD
- •
MRE has the advantage of depicting extraluminal abnormalities, the ability to distinguish active from fibrotic strictures, and better delineates fistulas. There is no ionizing radiation.
- •
Despite the advantages, there are some limitations, foremost is the relatively long acquisition times. It may be difficult to identify early mucosal lesions.
- •
Optimal amount of oral contrast for MRE is approximately 1300 mL
- •
Types of oral contrast for MRE:
- •
Positive: increased signal of bowel lumen on T1 and T2; solutions containing carbohydrate sugar alcohols (VoLumen) or gadolinium (Gd)-based agents
- •
Negative: decreased signal of bowel lumen on T1 and T2; iron oxide containing oral contrast (Gastromark)
- •
- •
Typical patient preparation for MRE
- •
Fasting for 6 hours before procedure
- •
- •
Sequences for MRE:
- •
Half-Fourier-acquired single-shot turbo spin echo (HASTE) or SSFSE; insensitive to motion. Provides high contrast between lumen and bowel wall
- •
High-resolution ultrafast balanced GRE (fast imaging employing steady-state acquisition [FIESTA], True FISP). Insensitive to motion and provides uniform luminal opacification. Ideal for detection, mesenteric findings in patients with Crohn disease
- •
T2W (fat saturated) or STIR. Ideal for detection of fistulas and for correlating inflammatory changes with Gd enhanced images.
- •
T1-weighted (T1W) 3D gradient echo sequence before and after gadolinium (Gd) administration. Primarily used to assess bowel wall enhancement, extraluminal findings
- •
- •
Fibrosis findings
- •
Low T2 signal in a thickened loop
- •
Delayed enhancement
- •
- •
Acute inflammation findings
- •
Wall thickening
- •
Early mucosal enhancement
- •
Engorgement of the vasa recta
- •
Diffusion restriction in the wall
- •
Polyps
A wide variety of colonic polyps exist. Nonneoplastic, hyperplastic polyps have been cited as the most frequent type for a long time.
| Single Polyp | Multiple Polyps | |
|---|---|---|
| Neoplastic | ||
| Epithelial | Tubular adenoma | Familial polyposis |
| Tubulovillous adenoma | Gardner syndrome | |
| Villous adenoma | ||
| Turcot syndrome | ||
| Nonepithelial | Carcinoid | |
| Leiomyoma | ||
| Lipoma | ||
| Fibroma | ||
| Nonneoplastic | ||
| Hamartomas | Hamartoma | Cronkhite–Canada syndrome |
| Juvenile polyposis Peutz-Jeghers syndrome | ||
| Inflammatory | Benign lymphoid polyp | Juvenile polyp, benign lymphoid polyp |
| Fibroid granulation polyp | Granulomatous colitis | |
| Unclassified | Hyperplastic polyp | Hyperplastic polyposis |
Adenomatous Polyps
Most common true colonic tumor (in up to 10% of the population by the seventh decade). Up to 50% of polyps are multiple.
Clinical Findings
- •
Asymptomatic
- •
Diarrhea
- •
Pain
- •
Hemorrhage
| Tubular | Tubulovillous | Villous | |
|---|---|---|---|
| Frequency | 64% | 27% | 9% |
| Malignancy potential | |||
| 0.5–0.9 cm | 0.3% | 1% | 2% |
| 1.0–1.9 cm | 4% | 7% | 6% |
| 2.0–2.9 cm | 7% | 11% | 17% |
Location ( Fig. 3.30 )
- •
Rectum and sigmoid, 60%
- •
Descending colon, 15%
- •
Transverse colon, 15%
- •
Ascending colon, 10%

Differentiation of Benign and Malignant Polyps
- •
Histologic differentiation of polyps is invariably difficult radiographically, so the majority of lesions require endoscopic sampling.
| Feature | Benign | Malignant |
|---|---|---|
| Size a | <1 cm | >2 cm |
| Stalk | Present (pedunculated, thin) | Absent (sessile) |
| Contour | Smooth | Irregular, lobulated |
| Number | Single | Multiple |
| Underlying colonic wall | Smooth | Indented, retracted |
a The larger the size of any polyp, the more likely it is malignant: <1 cm: 0.4%, 1–2 cm: 4%, >2 cm: >10%.
Advanced Adenoma ( Fig. 3.31 )
- •
Polyp ≥1 cm, high-grade dysplasia
- •
Of all polyps <1 cm, the likelihood that a lesion is an advanced adenoma is 3% (the majority are hyperplastic and the rest are benign adenomas).

Hyperplastic Polyps
Focal proliferation of normal mucosa, hence not an adenoma. Hyperplastic polyps have no malignant potential. Hyperplastic polyps are due to excessive cellular proliferation in Lieberkühn crypts. Seventy-five percent of polyps occur distal to the splenic flexure, mostly in the rectosigmoid area.
Imaging Features
- •
Stalked polyp
- •
Sessile but <5 mm
Postinflammatory Polyps (PIPs)
Postinflammatory polyposis (pseudopolyposis, filiform polyps) represents a benign condition, not associated with cancer. PIPs occur most commonly in Crohn disease and ulcerative colitis (UC) as a result of regeneration of nonulcerated tissue.
Imaging Features
- •
Filiform polyps: thin, short, branching structures
| Polyp | Pseudopolyp | |
|---|---|---|
| Size | Uniform in size | Uniform in size |
| Form | Round, stalked, sessile | Y-shaped, filiform, irregular |
| Margins | Well delineated | Fuzzy (inflammation) |
| Colonic haustra | Preserved | Distorted (inflammation) |
Polyposis Syndromes
| Type | Trait | Gastric | SB | Colon | Histology | GI Malignancy | Extraintestinal |
|---|---|---|---|---|---|---|---|
| Familial polyposis | AD | <5% | <5% | 100% | Adenoma | 100% | — |
| Gardner | AD | 5% | 5% | 100% | Adenoma | 100% | Osteoma, others a |
| Peutz-Jeghers | AD | 25% | 95% | 30% | Hamartoma | Rare | Perioral pigmentation |
| Juvenile polyposis | AD | — | — | 100% | Inflammatory | ? | — |
| Turcot | AR | — | — | 100% | Adenoma | 100% | Glioma |
| Cronkhite-Canada | NH | 100% | 50% | 100% | Inflammatory | None | Ectodermal changes |
| Cowden b | AD | — | — | — | Hamartoma | None | Oral papilloma c |
| Ruvalcaba-Myhre b | AD | Yes | Yes | Yes | Hamartoma | None | Macrocephaly, penile macules, mental retardation, SC lipomas |
a Soft tissue tumors, sarcomas, ampullary carcinoma, ovarian carcinoma.
Familial Polyposis
- •
Most common intestinal polyposis syndrome (incidence 1 : 8000)
- •
Screening of family members of familial polyposis patients should start at puberty: malignant degeneration by 40 years (treatment: prophylactic total proctocolectomy)
- •
Usually >100 polyps
- •
Polyps may be sessile or stalked.
- •
Familial adenomatous polyposis syndrome is a common umbrella name under which Gardner and familial polyposis syndromes are included.
Gardner Syndrome
- •
Polyposis: colon 100%, duodenum 90%, other bowel segments <10%
- •
Hamartomas of stomach
- •
Soft tissue tumors: inclusion cysts, desmoids (30%), fibrosis
- •
Osteoma in calvarium, mandible, sinuses
- •
Entrapment of cranial nerves
- •
Malignant transformation in 100% if untreated
- •
SB and pancreaticoduodenal malignancies
- •
Total colectomy recommended
Peutz-Jeghers Syndrome
- •
Second most common intestinal polyposis
- •
Autosomal dominant
- •
Hamartomas throughout GI tract except the esophagus
- •
Mucocutaneous pigmentations (buccal mucosa, palm, sole)
- •
Polyps have virtually no malignant potential.
- •
Slightly increased risk of stomach, duodenal, and ovarian cancer; benign neoplasm of testes, thyroid, and GU system
Juvenile Polyposis
- •
Usually large polyps in rectum
- •
Usually single; 80% are located in the rectosigmoid.
- •
Present in children with bleeding, prolapse, or obstruction
Cowden Disease
- •
Multiple hamartoma syndrome
- •
Mucocutaneous pigmentations (buccal mucosa, palm, sole)
- •
Most common in rectosigmoid with lesions also present in esophagus
- •
Mucocutaneous lesions → facial papules, oral mucosal papillomatosis, acral keratoses, sclerotic fibromas
- •
Thyroid gland abnormalities: goiter, adenomas
- •
Breast cancer (ductal), bilateral in 30%
- •
Uterine and cervical carcinomas
- •
Transitional cell carcinoma (TCC) of bladder and ureter
Turcot Syndrome
- •
Glioma polyposis syndrome
- •
Colonic adenomas with CNS gliomas and medulloblastomas
Colon Carcinoma
General
Third most common cancer in both men and women. Risk factor: being overweight or obese, being inactive, and diets high in red meat and/or low in fruits and vegetables. Synchronous lesions, 5%; metachronous lesions, 3%.
Modifiable Cancer Risk Factors
- •
Being overweight or obese
- •
Inactivity
- •
Diets high in red meat
- •
Diets low in fruits and vegetables
- •
Smoking
- •
Heavy alcohol use
Nonmodifiable Cancer Risk Factors
- •
Personal history of colorectal cancer or adenomatous polyps
- •
Personal history of chronic IBD
- •
Strong family history of colorectal cancer or polyps (cancer or polyps in a first-degree relative <60 years old or in two first-degree relatives of any age).
- •
Older age
- •
African American or Ashkenazi Jewish descent
Note: A first-degree relative is defined as a parent, sibling, or child.
Location
- •
Rectum, 35%
- •
Sigmoid, 25%
- •
Descending colon, 10%
- •
Ascending colon, 10%
- •
Transverse colon, 10%
- •
Cecum, 10%
Imaging Features ( Fig. 3.32 )
- •
Polypoid
- •
Ulcerative
- •
Annular constricting (apple core); <5 cm long
- •
Plaque-like (e.g., cloacogenic tumor at anorectal junction)
- •
Scirrhous carcinoma (rare): long (>5 cm) circumferential spread

Complications
- •
Obstruction
- •
Intussusception (in polypoid lesions), rare
- •
Local perforation (simulates diverticulitis)
- •
Local tumor recurrence
- •
Peritoneal spread
Staging ( Fig. 3.33 )
Dukes staging system
- •
Dukes A: Limited to bowel wall, 15%; 93% 5-year survival
- •
Dukes B: Extension into serosa or mesenteric fat, 35%; 77% 5-year survival
- •
Dukes C: LN metastases, 35%; 48% 5-year survival
- •
Dukes D: Distant metastases (15%): liver, hydronephrosis, peritoneal cavity, adrenal; 7% 5-year survival
- •

Tumor-Node-Metastases (TNM) Classification
Tx: No description of the tumor’s extent is possible.
Tis: The cancer is in the earliest stage. It has not grown beyond the mucosa (inner layer) of the colon or rectum. This stage is also known as carcinoma in situ or intramucosal carcinoma.
T1: Cancer has grown through the mucosa and extends into the submucosa.
T2: Cancer has grown through the submucosa, and extends into the muscularis propria.
T3: Cancer has grown completely through the muscularis propria into the subserosa but not to any neighboring organs or tissues.
T4: Cancer has spread completely through the wall of the colon or rectum into nearby tissues or organs.
Nx: No description of LN involvement is possible because of incomplete information.
N0: No LN involvement
N1: Cancer cells found in 1–3 nearby LNs.
N2: Cancer cells found in 4 or more nearby LNs.
Mx: No description of distant spread is possible because of incomplete information.
M0: No distant spread is seen.
M1: Distant spread is present.
Diagnostic Accuracy
Detection of LN metastases
- •
CT: 50%–70%
- •
MRI currently < CT
- •
Detection of liver metastases
- •
Contrast-enhanced CT: 60%–70%
- •
MRI: 70%–80%
- •
Rectal MRI
- •
Primarily used to stage and differentiate T2 from T3 disease since T3 disease requires neoadjuvant chemoradiation before surgery
- •
T2W is the most reliable sequence for local staging.
- •
Can have desmoplastic reaction with linear T2 hypointensity in T2 disease
- •
Need nodular extension of T2 intermediate tumor outside of the lamina propria to claim T3 diseaseNeed nodular extension of T2 intermediate tumor outside of the muscalaris propria to claim T3 disease
- •
Closely evaluate external iliac LNs as these denote M1 (distant metastatic disease) in rectal cancer.
Colitis
Causes
Idiopathic IBD
- •
UC
- •
Crohn disease
- •
Behçet disease
- •
Infectious colitis
Ischemic colitis
Iatrogenic
- •
Radiation
- •
Chemotherapy
- •
Imaging Features
The imaging features of bowel inflammation (any cause) depend mainly on the location of the process:
Mucosal inflammation
- •
Ulceration
Shallow: granularity of mucosa, aphthoid
Deeper: flask like collections of barium: collar button
- •
Edema
Displacement of barium: translucent halo around central ulcer
- •
Spasm
Localized persistent contraction
Narrowing of bowel lumen
- •
Submucosal inflammation
- •
Ulcers (deeper linear than in mucosal inflammation): cobblestone appearance
- •
Bowel wall thickening
CT: wall thickened (>3 mm with lumen distended)
Halo: fatty (chronic), gray (subacute or chronic), white (acute) with enhancement
- •
Subserosal mesenteric inflammation
- •
Stranding in surrounding fat
- •
Inflammatory mass
- •
Fistula
- •
Creeping fat: excessive fat deposited around serosal surface (Crohn disease)
- •
Crohn Disease (Regional Enteritis) ( Fig. 3.34 )
Recurrent inflammatory condition of bowel because of altered immunity to intestinal flora. Lesions may occur in the entire GI tract but are most common in:
- •
SB (especially terminal ileum), 80%
30% only SB involved
50% SB and colon involved
- •
Colon, 70%
25% of patients with colonic disease have pancolitis (entire colon affected)
- •
Duodenum, 20%
Pathologic development of lesions: initial event → hyperplasia of lymphoid tissue in submucosa → lymphedema → aphthoid ulcerations → deeper ulcers → fistulas, abscesses → strictures

Imaging Features ( Fig. 3.35 )
Types of lesions
- •
Thickening of folds (edema)
- •
Nodular pattern (submucosal edema and inflammation)
- •
String sign: tubular narrowing of intestinal lumen (edema, spasm, scarring depending on chronicity)
- •
Omega sign: asymmetric wall involvement results in contracture and C-shaped loop on SB series
- •
Ram horn sign: loss of antral fornices with progressive narrowing from antrum to pylorus
- •
Ulcerations:
Aphthoid ulcers are early lesions and correspond to mucosal erosions (pinpoint ulcer in edematous mound up to 3 mm in diameter and 2 mm in depth).
Ulcers are irregularly scattered throughout GI tract and are interspersed with normal mucosa.
Ulcerations grow and fuse with each other in linear fashion and, with intervening edematous mucosa, produce an ulceronodular pattern (“cobblestone” appearance).
- •
Filiform polyposis: thin, elongated, branching mucosal lesions; represents proliferative sequelae of mucosa adjacent to denuded surface
- •
Sinus tracts and fistulas originate in fissures or deep ulcers; characteristic of Crohn disease at advanced stages.
- •
Fatty thickening along mesenteric border (creeping fat) and paracolonic lymphadenopathy separate bowel loops.
- •
Fibrosis and scarring may result in:
Pseudodiverticula (fibrosis develops eccentrically)
Rigid, featureless bowel
Strictures and obstruction
Foreshortening of bowel
- •
Spatial arrangement of lesions
- •
Transitional zones are typical; they occur between involved bowel loops and normal bowel.
- •
Skip lesions are typical: discontinuous involvement of bowel
- •
Lesions appear preferentially at mesenteric side of intestine.
- •

Mural and Extramural Changes (CT Findings)
Primary intestinal findings
- •
Bowel wall thickening
Normally <3 mm if well distended
Mean diameter in Crohn disease: 10 mm
If >10 mm, include pseudomembranous, ischemic, or CMV colitis in DDX.
- •
Circumferential submucosal low attenuation surrounded by higher outer attenuation: halo sign
- •
Inner and outer layers surrounding low-attenuation middle layer: target sign; middle layer of fat density; chronic, middle layer of water density
- •
Peribowel inflammation (“dirty fat,” “ground glass”)
Mesentery
- •
Fat accumulates on serosal surfaces (“creeping fat”)
- •
Inflamed mesentery fat (stranding, “misty”)
- •
Adenopathy in SB mesentery common
- •
Comb sign: vasa recta stretched out along one wall of colon
- •
Extraintestinal findings
- •
Gallstones
- •
Osseous complications (may cause pain)
Spondylitis
Sacroiliitis
Steroid complications: osteomyelitis, osteoporosis, avascular necrosis
- •
Renal stones, 7%
- •
Complications ( Fig. 3.36 )
- •
Recurrence of disease after surgery (in contrast to UC, in which proctocolectomy is curative)
- •
Increased incidence of malignancies:
GI tract tumors
Lymphoma
- •
TMC
- •
Fistulas
- •
Abscess formation