General Pediatric Problems
Russ Horowitz
INTRODUCTION
Ultrasound is an extremely useful tool in the emergency evaluation and management of children. The preceding chapters in this book have addressed imaging principles, anatomy, and pathology for a general population. Although this content is largely useful for children as well, sometimes relatively minor alterations in technique, variations in anatomy, and different applications are important to note for children; we have highlighted these differences throughout the text. Some pediatric content differs enough that it merits more discussion. The next three chapters focus on content specific to pediatrics. Chapter 26 reviews basic principles of imaging in children, and content particularly relevant to children, including assessment of hydration, estimation of bladder volume, workup of limp in children (septic hip, transient synovitis), head injury, nonaccidental trauma, and bronchiolitis. Chapter 27 reviews abdominal applications for ultrasound in children, including appendicitis, pyloric stenosis, intussusception, and malrotation. Lastly, Chapter 28 devotes a separate section on ultrasound guidance for procedures commonly performed in a pediatric emergency department (ED).
There are a number of reasons why sonography is particularly attractive in children, most notably its absence of ionizing radiation. Children have increased sensitivity to the malignancy-related effects of ionizing radiation and long expected life spans, which allows more time for the appearance of the detrimental effects (1,2). Utilization of ultrasound reduces reliance on radiographs and computerized tomography (CT) scanning and their associated radiation risks. Children often are unable to remain perfectly still, are uncooperative, and are unable to suspend respiration. Ultrasound allows rapid bedside evaluation of pediatric patients. This reduces time in the stressful environment of the ED and permits radiographic evaluation without the need for sedation.
Children are uniquely suited for ultrasound imaging. Adipose tissue degrades sonographic images, and generally children have less subcutaneous and intra-abdominal body fat. In adults, one is often forced to choose between penetrance and resolution. However, with their relatively small size, excellent imaging can be accomplished in pediatric patients using higher frequency and high resolution transducers.
The use of point of care ultrasound in the evaluation of pediatric patients in the ED is a new and evolving practice. Assessment has been useful in identifying conditions, narrowing the differential diagnosis, and expediting care. This is true for both traditional applications as well as novel “pediatric” ones including appendicitis, intussusception, pyloric stenosis, fractures unique to children, hip effusions, and nonaccidental trauma.
Although there are some subtle details that improve image acquisition in pediatrics, the general techniques are very similar. Differences however lie in the approach to the pediatric patient, the diagnostic questions that are asked, and the significance of findings.
The dynamic nature of sonography permits positioning of children to maximize their comfort and reduce anxiety. A creative approach to imaging children will go a long way toward increasing cooperation. A brief introduction to the machine will reduce their anxiety. Take advantage of their inquisitive nature and allow them to handle the probe (aka “camera on a string”) to prove it is not a needle and does not hurt. Position the screen (aka “TV”) or additional monitor if available so it is visible to the child and parent.
The examination can be performed with the child in the calming arms of the parents, improving cooperation. The use of distraction techniques (videos and music) and Child Life Specialists is useful to alleviate stress. Although these techniques may increase the time on the front end, they can reduce the overall scanning time and increase child cooperation and both child and parent satisfaction. Gel heated in commercially available warmers reduces discomfort and provides a warm, calming experience.
In adults, one must sacrifice improved resolution for increased depth, but that may not be the case in young children. Even intra-abdominal organs may be well visualized with a high-frequency probe. Because of unique pediatric anatomy, probe location must be adjusted for image optimization. A large curvilinear probe may simply not fit in the subxyphoid space of a toddler, so probe placement or selection must be adjusted.
The very same sonographic diagnosis in adults and children may have dramatically different implications. For example, cholelithiasis is a common and not unexpected finding in adults with right upper quadrant pain. In the absence of cholecystitis, no extensive workup is necessary. However, in a child, even a small uncomplicated biliary stone is unusual and warrants an extensive search for underlying diseases. A small amount of free fluid in the pelvis of a 25-year-old woman is physiologic, but that same amount in a 6-month-old with vomiting is never normal and necessitates an investigation for nonaccidental trauma.
Even in circumstances where traditional studies must be done by the radiology department, bedside studies will assist with prioritization of patients and mobilization of resources. For example, intussusception diagnosed with point of care sonography would expedite the reduction enema or, if not available at one facility, will expedite transfer to a facility with appropriate resources.
HYDRATION STATUS
Introduction
Dehydration is a common complaint in pediatric patients in the ED. Degree of dehydration is determined by assessment of clinical features, including change from baseline weight, heart rate, capillary refill time, and mucous membrane appearance. These features have technical limitations and are affected by fever, ambient temperature, and underlying illness. Clinical assessment of dehydration using the constellation of signs and symptoms has low sensitivity and specificity (3,4). The decision to obtain vascular access for intravenous (IV) hydration should not be taken lightly given the sometimes-challenging process in young children secondary to limited cooperation and small vessels. Ultrasound provides a rapid, noninvasive, and objective tool to assess hydration status in children. In adults, collapsibility of the inferior vena cava (IVC) can be used to guide initial fluid resuscitation. In children, the IVC/Aorta ratio is a more reliable measure (See Chapter 6). In euvolemic children the IVC/aorta ratio is approximately 1.0; lower values are seen in clinically dehydrated children (5,6).
Editor’s note: Some authors alternatively report the Aorta/IVC ratio.
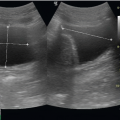
Image Acquisition
Place a mid-frequency curvilinear probe inferior to the xyphoid process in the transverse plane. Alternatively, a phased array or even high-frequency probe may be used to investigate the abdominal aorta and IVC. Transducer choice will be dictated by size and body habitus. Two anechoic circular structures will be visible anterior to the semicircular hyperechoic vertebral bodies. The circular structure on the patient’s right is the IVC, and the one on the left is the aorta. Color Doppler may be used for confirmation. Measure each in cross section. Use minimal pressure to avoid compressing the vessels.
Use of the Image in Clinical Decision Making
This bedside test may be used as an initial tool to assess need for IV hydration and response to oral rehydration therapy in children with concerns for dehydration (7). Physicians may choose to institute IV hydration in those with low IVC/aorta ratios and in those whose values do not approach 1.0 after oral rehydration.
BLADDER
Introduction
Urinalysis in young children is a common investigation and necessitates catheterization in neonates up to the age of toilet training. Unsuccessful catheterization occurs when insufficient urine is present in the bladder, requiring multiple attempts and repeated discomfort.
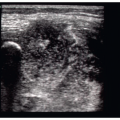
Image Acquisition
A mid-frequency transducer is the customary choice for bladder imaging. The probe is first placed in the transverse plane just superior to the pubic symphysis and angled caudally into the pelvis. The probe is then rotated 90 degrees clockwise to view the bladder in the long plane. Most ultrasound machines will calculate bladder volume when dimensions are measured in the three planes (See Abdominal Procedures, Chapter 13).
Use of the Image in Clinical Decision Making
Approximately one in four urethral catheterizations of young children is unsuccessful and does not provide sufficient urine volume for analysis (5). Repeat catheterizations subject the patient to additional trauma and increase parental angst. Bladder ultrasound eliminates the question of sufficient bladder volume. A transverse bladder dimension of >2 cm yields sufficient urine from a catheterized specimen. Ultrasound significantly improves the success
rate of urine catheterization and avoids multiple interventions (8, 9, 10). In addition, suprapubic catheterization success is also improved by bedside ultrasound (See Pediatric Procedures, Chapter 28) (11,12).
rate of urine catheterization and avoids multiple interventions (8, 9, 10). In addition, suprapubic catheterization success is also improved by bedside ultrasound (See Pediatric Procedures, Chapter 28) (11,12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree