• Left kidney usually lies—1–2 centimeters higher than the right. Extends from T12-L3 vertebrae usually.
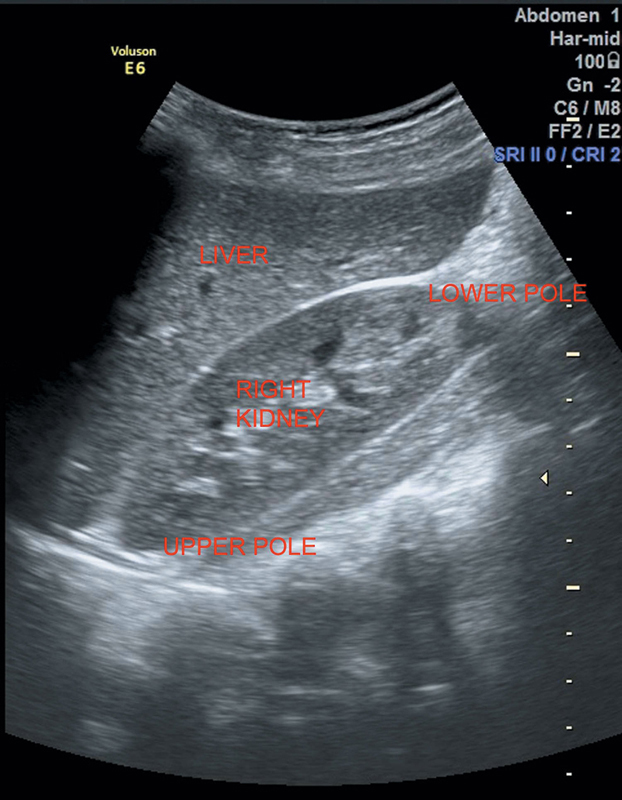
• Normal kidney measures approximately 9–13 centimeters in length and 4–6 centimeters in width. Size of both the kidneys should not differ by >2 centimeters (Figure 7.1).
• Renal parenchyma is composed of
Cortex: Usually less echogenic than the adjacent liver and spleen.
Medullary pyramids: More hypoechoic than cortex.
• Echogenic renal sinus containing urine collecting system, blood vessels, fat, and fibrous tissue seen in the center of kidney.
• The kidney has a thin, fibrous true capsule. Perirenal fat lies outside this capsule, encased anteriorly by the fascia of Gerota and posteriorly by the fascia of Zuckerandl.
Bilateral renal arteries arise from aorta at L1-2 vertebral body level.
Left renal vein is longer, passes between aorta and superior mesenteric artery (SMA) before entering into IVC.
Left gonadal vein drains into the left renal vein.
Right renal artery is longer, courses inferiorly, and passes posterior to IVC and right renal vein.
Figure 7.1 Depicting normal echotexture of right kidney in comparison to liver.
Left renal artery passes posterior to the left renal vein.
Four protective layers covering the kidney (inner to outer):
1. Fibrous capsule
2. Perirenal fat
3. Gerota’s fascia
4. Pararenal fat
30–34 centimeters long and 2–8 millimeters diameter. Nondilated ureter may not be visualized due to the overlying bowel gas. Normally, lie anterior to iliac vessels.
Trigone is an area demarcated by the ureteric and urethral orifices within the bladder. The wall thickness of bladder depends on the degree of bladder distension. Should be moderately filled for proper visualization. Normal bladder capacity is ~400–500 milliliters. Postvoid scan should be done to rule out any lower urinary tract pathology.
Hypertrophied column of Bertin: Normal variant representing the unresorbed polar parenchyma.
Sonographically, usually, seen at the junction of upper and middle thirds of the kidney.
Bordered by junctional parenchymal defect.
Indentation of renal sinus laterally.
Continuous with adjacent renal cortex.
It contains renal pyramids.
Generally <3 centimeters. May be misinterpreted for a small tumor. Presence of arcuate arteries by color Doppler (CD) differentiates it from a small tumor.
Renal hypoplasia: Kidney is small in size but otherwise normal.
Persistent fetal lobulation: Fetal kidney is normally lobulated. May persist as normal variant in adults.
Dromedary hump: Normal variant of contour of kidney due to splenic impression into superolateral border of the left kidney. It may simulate a renal mass but calyces and pyramids may extend into this pseudotumor.
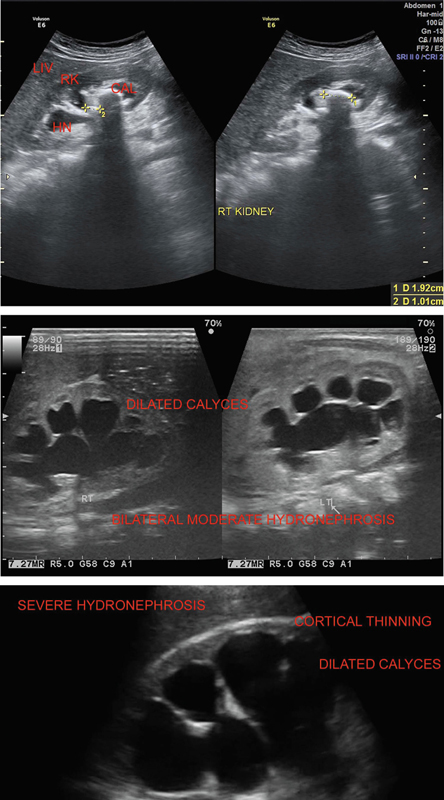
Dilated calyceal system and continuity of calyceal with renal pelvis differentiates it from cysts. Pelvi–calyceal system may dilate due to overhydration, overfilled urinary bladder (relieves after micturition), and pregnancy.
Grade1: Minimal splitting of pelvis—may be due to overfilled bladder.
Grade2: Mild—dilated pelvis and calyces.
Grade3: Moderate—both pelvis and calyceal system are dilated with mild parenchymal atrophy.
Grade4: Severe—markedly dilated pelvi–calyceal system with severe thinning of renal parenchyma (Figure 7.2).
Figure 7.2 Depicting varying grades of hydronephrosis as mild as moderate and severe.
Partial or complete duplication of the collecting system.
The lower pole collecting system inserts into the bladder at the normal site, but intramural portion may be shorter than usual leading to vesicoureteric reflux (VUR).
The upper pole ureter inserts ectopically inferomedial to the site of normal ureteral insertion. Its orifice may be stenosed and obstructed.
Patients with complicated renal duplications may present with urinary tract infections, failure to thrive, hematuria, and symptoms of bladder obstruction.
Females with urethral insertion of the upper pole ureter below the external urinary sphincter may present with chronic constant urinary incontinence or dribbling.
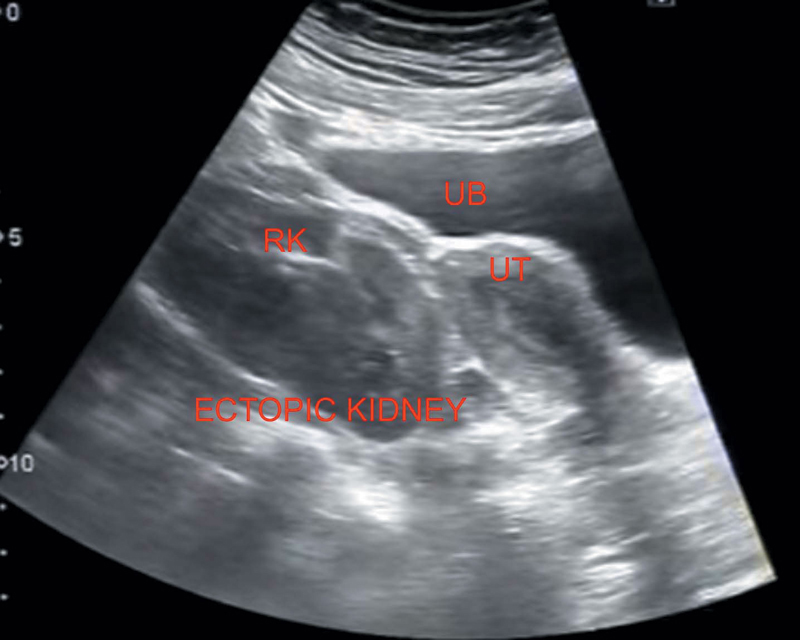
Failure of kidney to ascend during embryologic development results in pelvic kidney.
Kidneys are small sized with reduced functioning.
Ureters are short (Figure 7.3).
If the kidney ascends too high, it passes through Bochdalek’s foramen, results in thoracic kidney.
Figure 7.3 Showing ectopic right kidney in the pelvis.
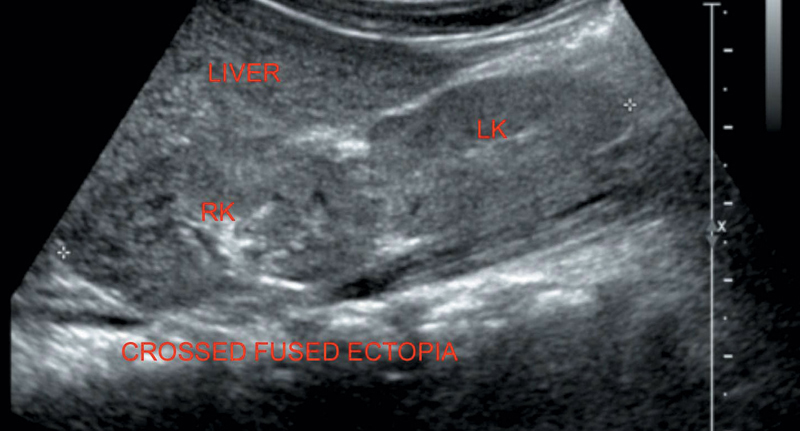
Figure 7.4 Illustrating normal right kidney cross fused with ectopic right kidney.
Both kidneys are found on the same side.
Ectopic kidney will be fused to the other kidney (Figure 7.4).
Ureteric-vesical junction (UVJ) is normally located.
Lies anterior to the abdominal great vessels.
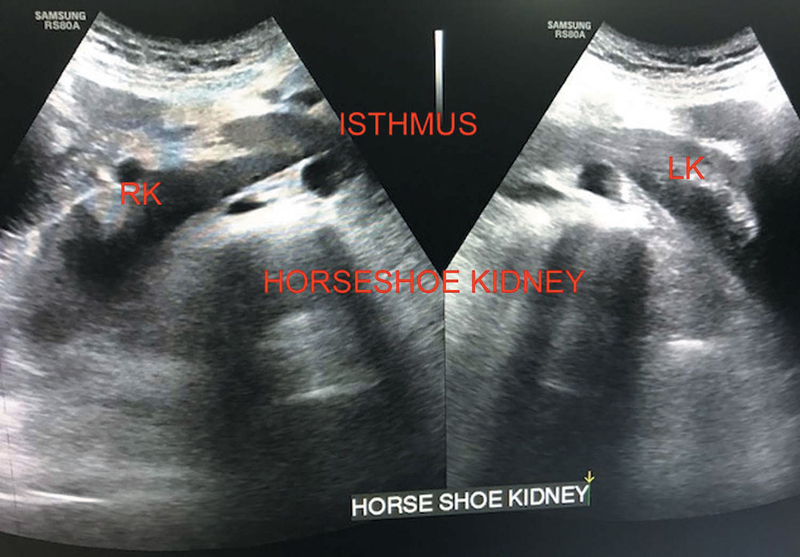
Fusion of lower poles with either functioning or fibrous isthmus.
Associated with pelvi-ureteric junction (PUJ) obstruction, VUR, and so on.
On sonography, kidneys are lower than normal with the poles projecting medially (Figure 7.5).
Hydronephrosis and calculi may be seen.
Figure 7.5 Illustrating horseshoe kidney.
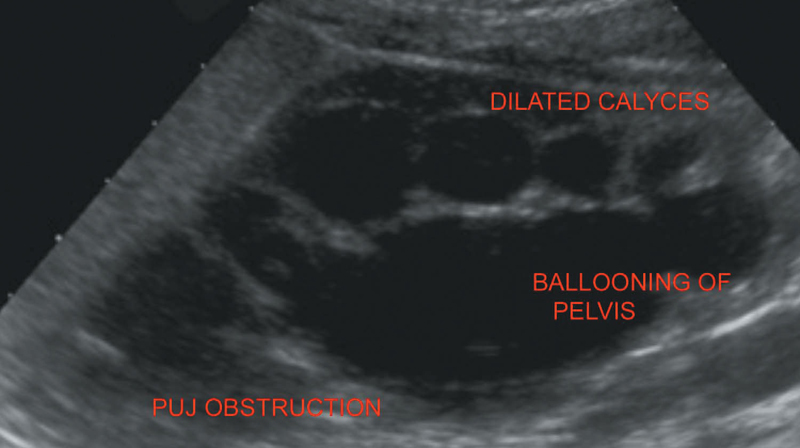
Figure 7.6 Illustrating PUJ obstruction.
PELVI-URETERIC JUNCTION OBSTRUCTION
M:F=2:1.
Left > Right.
On sonography, hydronephrosis up to the level of pelvi-ureteric junction.
Marked ballooning of the renal pelvis is present (Figure 7.6).
Usually kidneys appear normal. If abnormal, may show
• Altered echotexture
• Renal enlargement
• Loss of cortico-medullary differentiation
If focal, may appear as hypoechoic masses.
Untreated or inadequately treated APN may lead to parenchymal necrosis with abscess formation.
Diabetics, immunocompromised, and patients with chronic debilitating diseases are at an increased risk.
On USG, round, thick-walled hypoechoic complex masses with internal mobile debris.
Sometimes gas with dirty shadowing may also be seen.
D/D
• Hemorrhagic/infected cysts
• Parasitic cysts
• Multilocular cysts/cystic neoplasms
Small abscess: Treated conservatively.
Large abscess: Requires per cutaneous drainage/surgery.
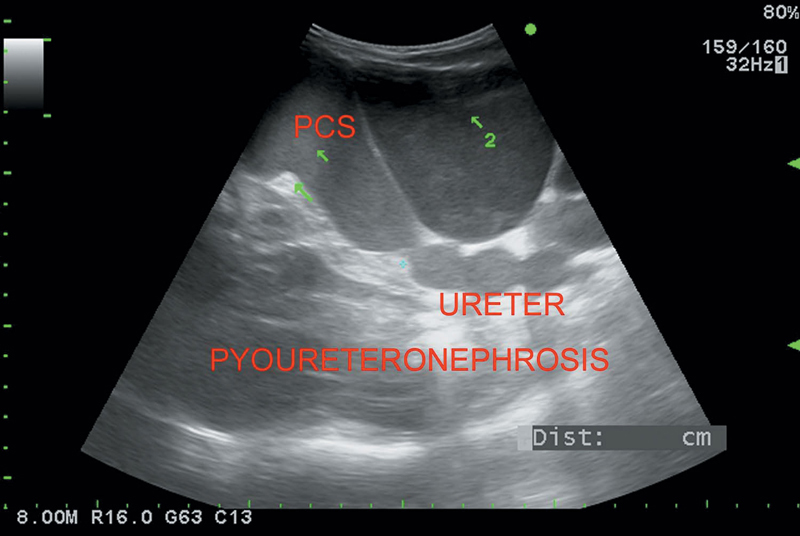
Purulent material in an obstructed collecting system
On sonography, hydronephrosis ± hydroureter
• Mobile debris (Figure 7.7)
• Gas with dirty shadowing may be seen
• Stones may be seen
Interstitial nephritis often associated with VUR.
On sonography
• Echogenic parenchyma with atrophy
• Dilated collecting system
Figure 7.7 Depicting dilatation of pelvicalyceal system and ureter with enlarged kidney and echogenic debris suggesting pyoureteronephrosis.
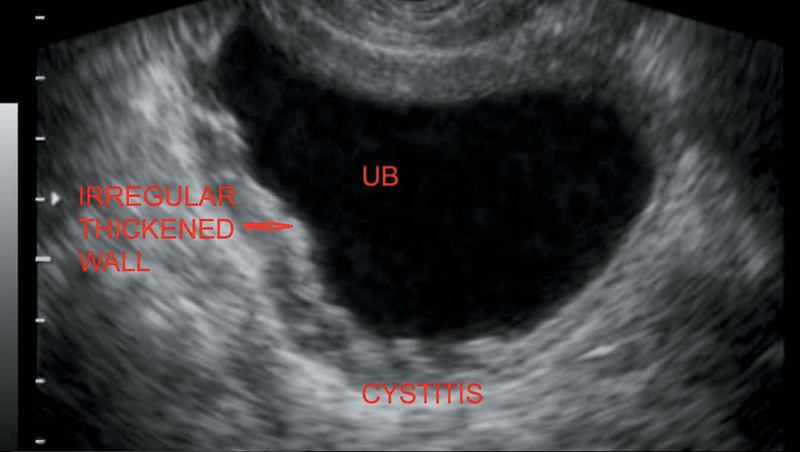
Figure 7.8 Depicting thickened and irregular bladder wall in a patient with cystitis.
Usually caused by E. coli.
Presents with bladder irritability and hematuria.
On sonography
• Diffuse irregular bladder wall thickening (Figure 7.8)
• Internal mobile echoes in the lumen may be seen
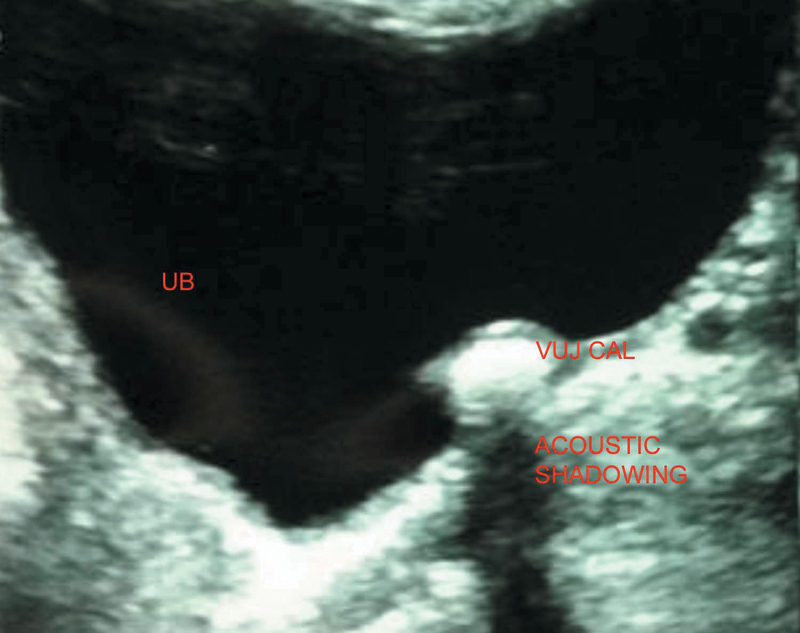
Most common type of stone is calcium oxalate (60%–80%).
Three areas of ureteric narrowing where the stone may lodge:
1. Just past the PUJ
2. Where the ureter crosses the iliac vessels
3. At the UVJ (most common site as ureter has its smallest diameter of 1–5 millimeters here)
On sonography → echogenic foci with distal acoustic shadowing seen and proximal hydroureteronephrosis. Sometimes hydronephrosis may not be present suggesting nonobstructing calculi. Twinkling artifacts may be seen on Doppler.
Staghorn calculus—coral calculus—take the shape of renal pelvis resembling horns of a stag. Occur due to recurrent infection; usually composed of struvite (Magnesium, Ammonium, Phosphate [MAP]).
Entities that mimic renal calculi
• Renal artery calcifications
• Intrarenal gas
• Calcified sloughed papilla
Figure 7.9 Showing a calculus at VUJ leading to upstream hydroureteronephrosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree