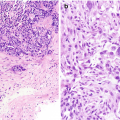
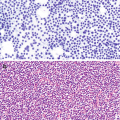
Sialosis . (a) Aspirate containing acini of serous salivary gland cells forming tight grapelike clusters of cells with granular cytoplasm and bland nuclei. The acini are oriented around ductal structures composed of flattened cells with high nuclear:cytoplasmic ratios. (b) In histologic sections, normal salivary gland parenchyma is predominantly made up of serous cells with basophilic coarse granules and mucinous cells with clear rarified cytoplasm in various proportions. A minor ductal element is seen with well-formed lumina
Non-neoplastic Conditions
Sialosis
General Characteristics
Diffuse non-neoplastic enlargement of the major salivary glands.
Usually bilateral; gives a “chipmunk” facial appearance
May occur in the settings of diabetes, alcoholism, or malnutrition.
Ultrasound (US)
On US, sialosis appears as a diffusely enlarged gland with a normal sonographic appearance of the parenchyma, without any focal lesion.
Computed Tomography (CT)
On CT, marked enlargement of both parotid glands may be seen with normal submandibular and sublingual glands. The attenuation coefficient of the parotid glands may be equivalent to that of fat (−55 Hounsfield units) and much lower than the normal range for parotid-gland parenchyma of −25 to 10 Hounsfield units, which is typically seen. Prominent septa of soft-tissue density may be seen within the gland parenchyma [5]. Alternatively, the size enlargement may be the only finding without change in the density of the tissue (Fig. 9.2).
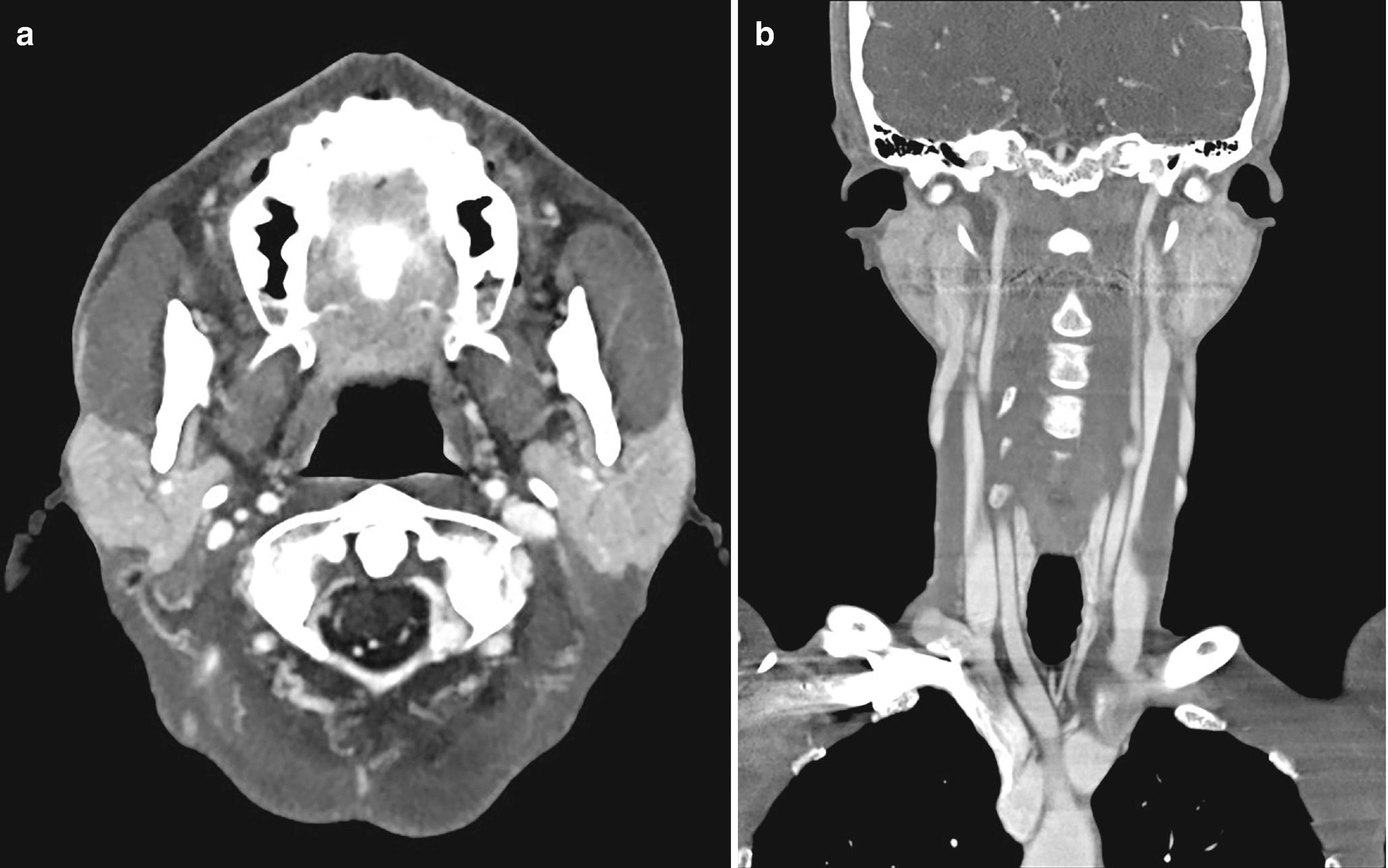
Sialosis . Contrast-enhanced axial (a) and coronal (b) CT demonstrates moderate enlargement of the parotid glands without focal lesions; this is most compatible with sialosis
Fine Needle Aspiration (FNA)
Aspirates from patients with sialosis contain lobules of unremarkable acinar cells, fat, and sheets of ductal cells [6]. The distinction between normal salivary gland tissue and sialosis is made on the basis of clinical findings as well as the fact that the lobules of acinar tissue are significantly larger than those seen in aspirates from normal salivary glands.
Core Biopsy
In core biopsies, sialosis resembles normal salivary gland tissue, but with larger lobules of acinar cells.
Sialolithiasis
General Characteristics
A calcified mass (sialolith) forms within the salivary gland ductal system.
It typically involves the submandibular gland but also may involve other major and minor salivary glands.
May result in secondary infection.
Ultrasound
Stones appear as strongly hyperechoic foci with distal acoustic shadowing. Small stones (<2 mm) may not shadow [7]. In cases of obstruction, the gland may appear enlarged with dilatation of the ducts proximal to the stone.
Computed Tomography
On CT, the stones appear intensely hyperdense (Fig. 9.3), both within the duct and within the gland. In cases of obstruction, the gland may appear enlarged, hyperdense, and associated with stranding and enhancement following contrast administration. In chronic cases, fatty atrophy will be evident, with the parenchyma reduced in volume and replaced by fat.
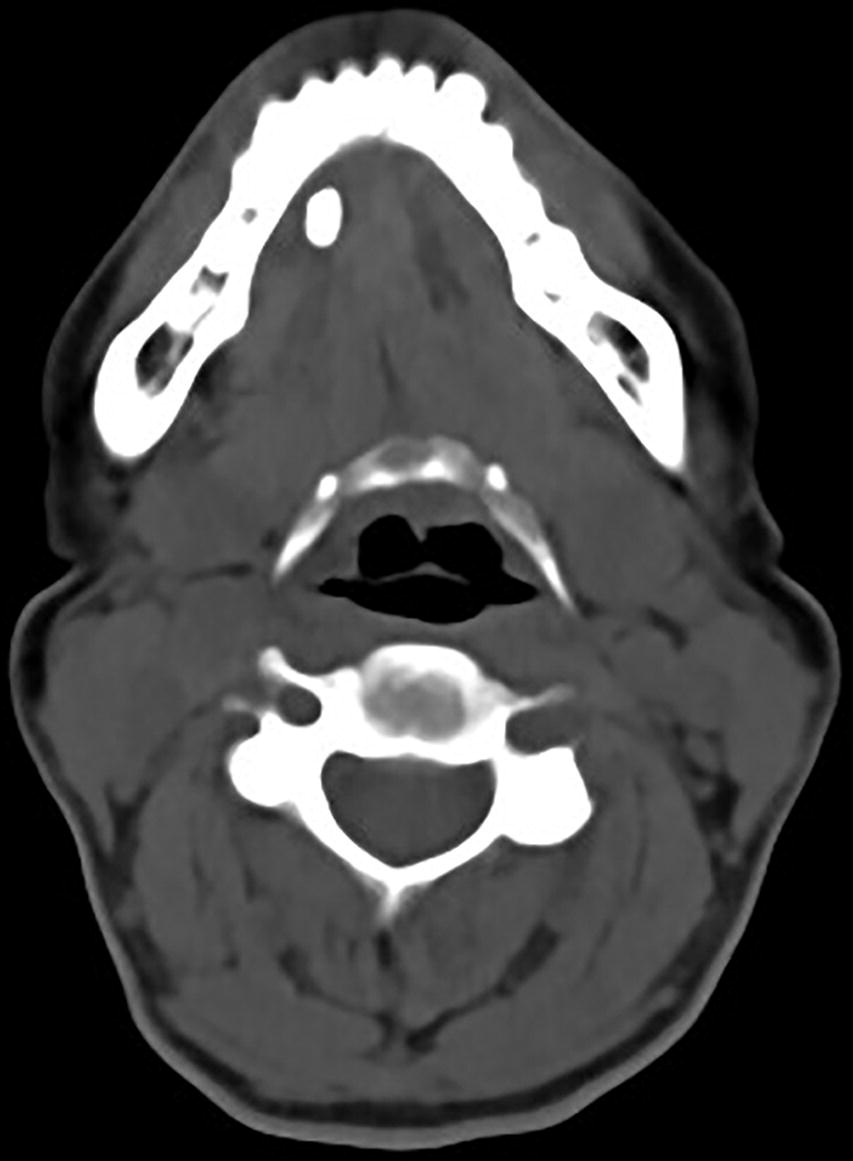
Sialolithiasis : non-contrast CT of the salivary glands demonstrates moderate sized hyperdense stones in the right submandibular gland duct
Magnetic Resonance Imaging
MRI is not only able to visualize larger stones but also in many instances is able to map the ductal anatomy and to assess the gland [8]. Stones appear as low-signal regions (on all sequences) outlined by high-signal saliva on T2-weighted images. In cases in which a small nonobstructive sialolith is present, the gland may appear entirely normal in appearance.
Fine Needle Aspiration
In aspirates, stone fragments may be seen in occasional cases [9]. Other findings are relatively nonspecific and include extravasated mucin, hyperplastic epithelial fragments with mucinous metaplasia, and acute and chronic inflammation.
Core Biopsy
Core biopsies in some cases may demonstrate ductal ectasia with chronic inflammation and stone fragments.
Sialadenitis
General Characteristics
Inflammation of the salivary gland.
May be acute or chronic and present with localized or systemic symptoms.
May be infectious or noninfectious (often autoimmune) in etiology.
Ultrasound
On US, the affected gland appears enlarged , hypoechoic, and hyperemic [10]. In chronic forms, the affected gland appears atrophic and diffusely hypoechoic with irregular margins. There may be evidence of sialectasis if there is recurrence.
Computed Tomogaphy
On CT, the salivary gland may be enlarged with abnormal attenuation, indistinct margins, and vivid contrast enhancement with associated adjacent fat stranding (Fig. 9.4) and/or thickening of the deep cervical fasciae that are typically unilateral [10]. Enlarged intra- or extraglandular lymph nodes may also be seen but are nonspecific.
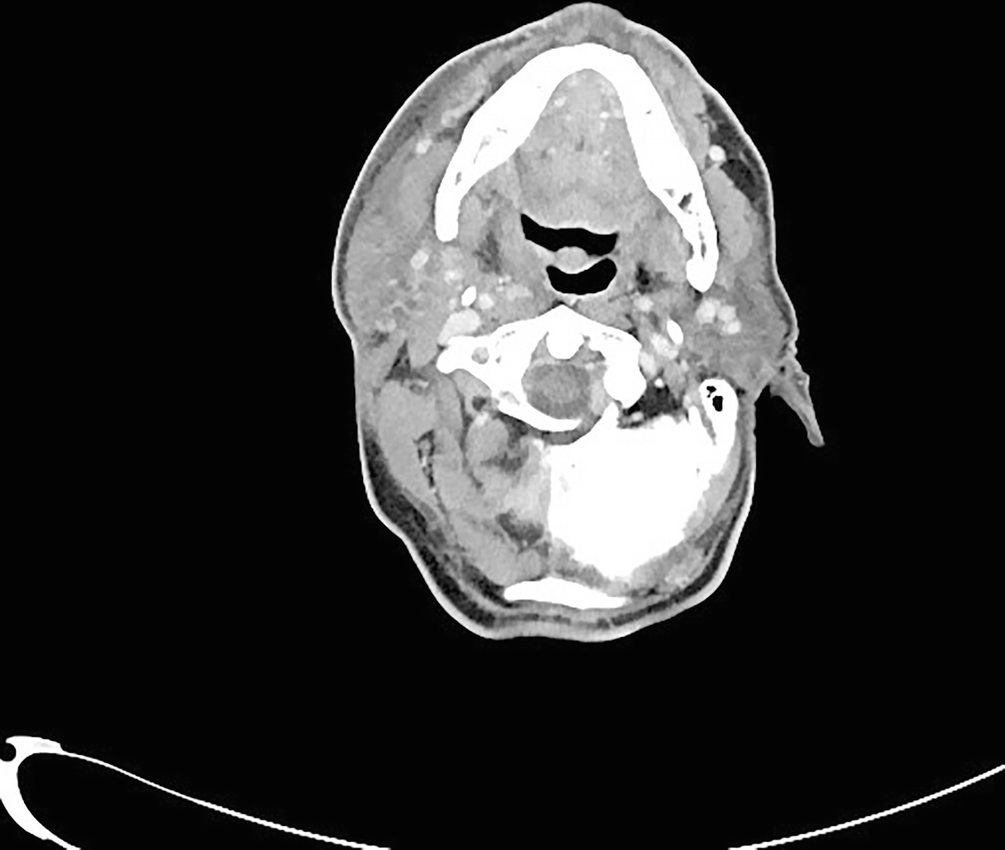
Sialadenitis : Axial contrast-enhanced CT of the salivary gland demonstrates extensive inflammation and fat stranding in the soft tissues surrounding the right parotid gland and overlying subcutaneous tissues. No definite sialolith is visualized along the course of the right Stensen duct
Magnetic Resonance Imaging
The involved gland is often enlarged. The affected gland can range from well-defined to poorly defined. Signal characteristics in the majority of cases tend to be heterogeneous [10]. The gland has a low T1 signal and a high signal on T2 sequences in acute forms. The T2 signal may be low in chronic forms secondary to fibrosis.
Fine Needle Aspiration
Aspirates from cases of chronic sialadenitis are typically hypocellular. Occasional fragments of ductal epithelium are seen with interspersed lymphoid tangles and irregular fragments of fibrotic stromal tissue (Fig. 9.5a, b) [11].
In cases of acute sialadenitis, the aspirate is dominated by sheets of neutrophils and degenerated metachromatic material.
Sialadenitis with crystalloid formation has a distinctive appearance, yielding cyst fluid with numerous, variably shaped amylase crystalloids in a background of histiocytes, inflammation, and reactive ductal cells.
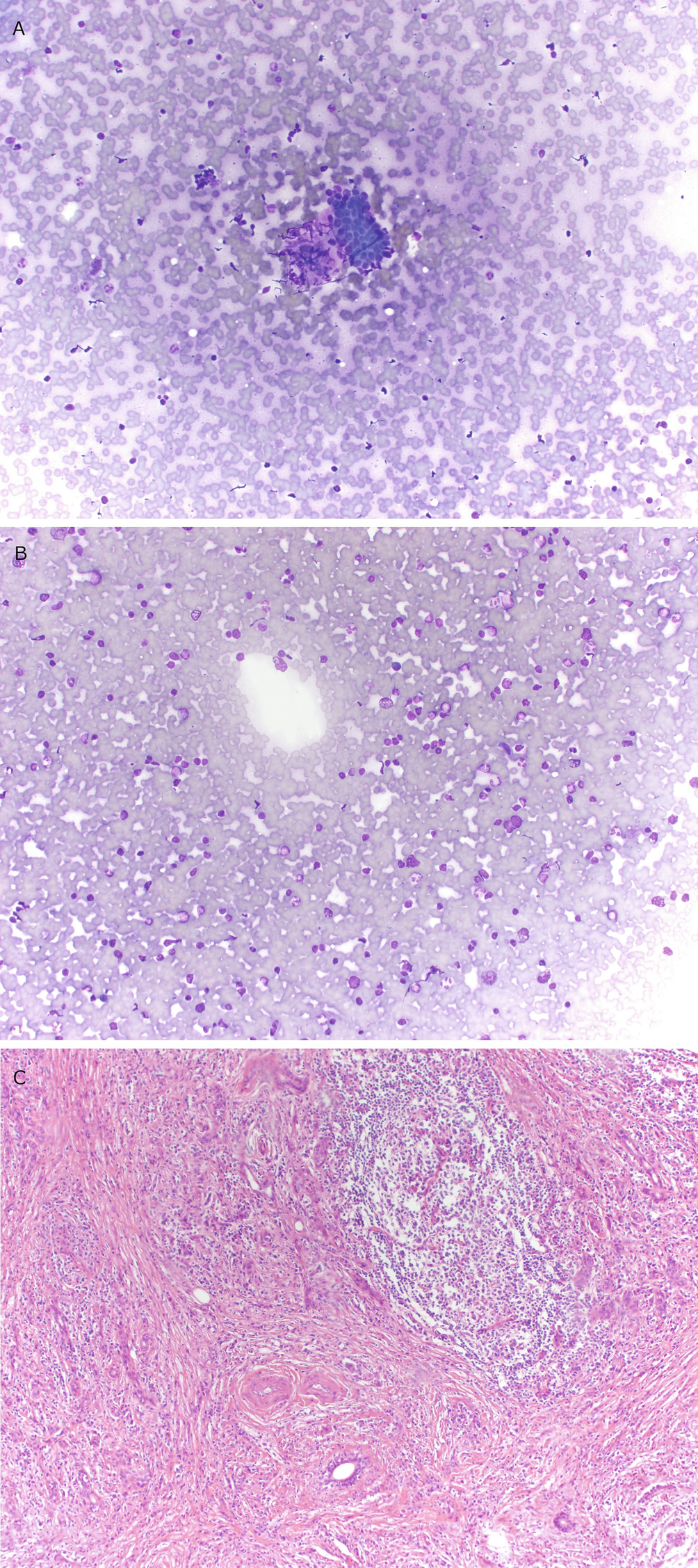
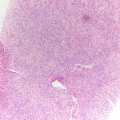
Chronic sialadenitis : (a) Hypocellular aspirate containing rare clusters of nondescript basaloid ductal epithelium with high nuclear:cytoplasmic ratios. (b) The background of the aspirate contains numerous chronic inflammatory cells. (c) In histologic sections, a dense lymphoid infiltrate with germinal center formation, fibrosis, and loss of the salivary gland acinar tissue and preservation of the ductal structures is seen
Core Biopsy
In cases of longstanding chronic sialadenitis, prominent fibrosis is seen, along with loss of the normal acinar tissue. Chronic inflammation with germinal center formation may be prominent (Fig. 9.5c).
In cases of acute sialadenitis, the normal salivary gland structures are obscured by a neutrophilic infiltrate.
Comment
Some cases of chronic sialadenitis are related to IgG4-mediated sclerosing disease. The findings of cellular fibrosis, a lymphoplasmacytic infiltrate, and obliterative phlebitis in a core biopsy or resected specimen may suggest this diagnosis [12]. Measurement of serum or tissue IgG4 levels may be of value in this context.
Sialocele
General Considerations
Accumulation of saliva within tissue that typically develops as a result of an injured salivary gland.
Often the result of trauma, either surgical or otherwise.
Ultrasound
On US, the salivary gland cyst may appear as hypoechoic to anechoic, depending on its contents.
Computed Tomography
On CT, sialocele will vary in its density, depending on its contents, but it would typically measure fluid attenuation (Fig. 9.6).
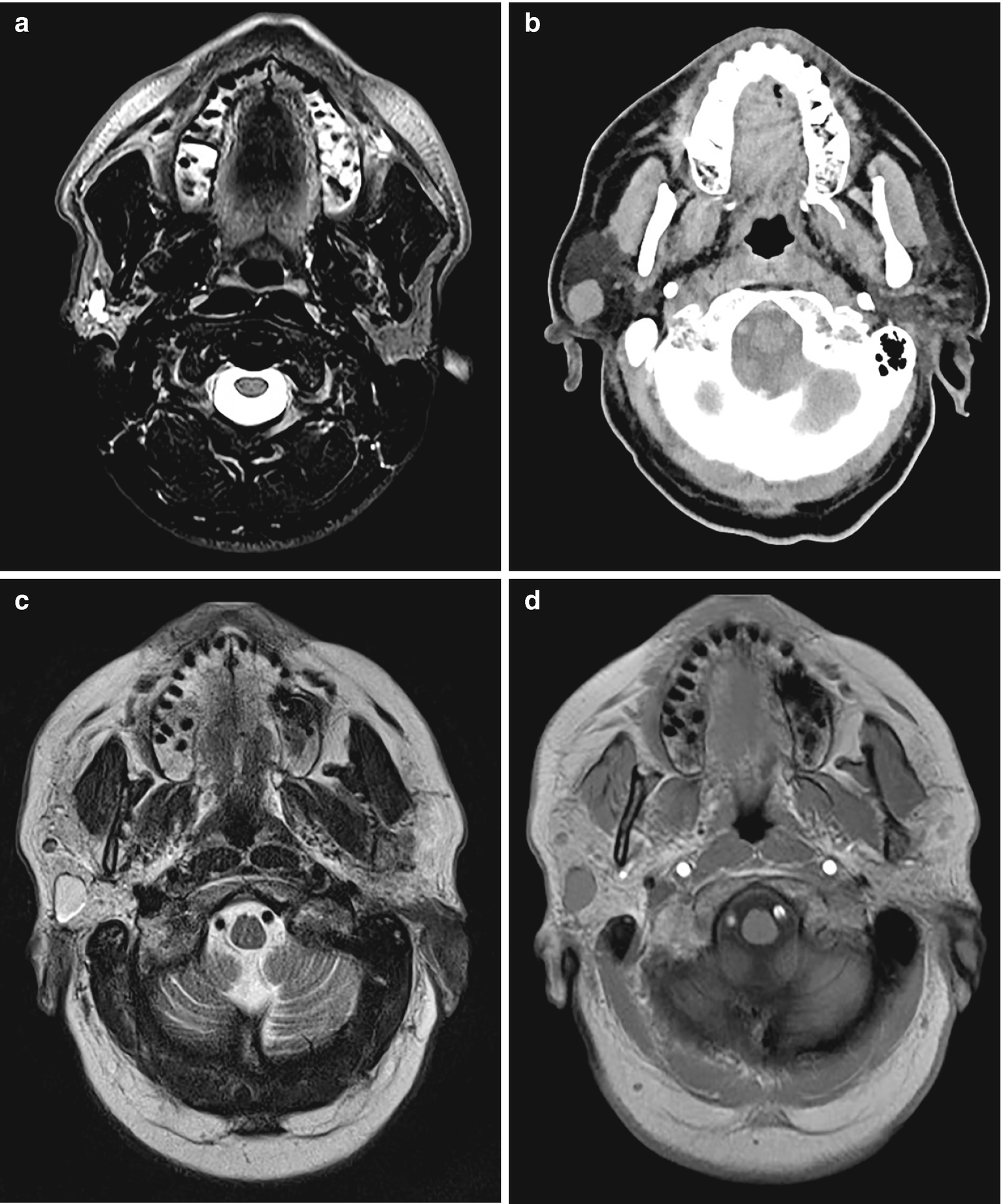
Sialocele : (a) Axial T2-weighted sequence demonstrates a small sialocele and mildly dilated intraparotid ducts. (b) Axial noncontrast CT demonstrates a round fluid-attenuation right parotid gland lesion consistent with a cyst. On MRI the lesion appears T2 hyperintense (c) and T1 hypointense (d)
Magnetic Resonance Imaging
T2-weighted sequence may show a sialocele to be T2 hyperintense. The cyst will be typically T1 hypointense and does not demonstrate enhancement.
Fine Needle Aspiration
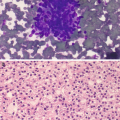
Aspirates are hypocellular and often contain mucin with occasional histiocytes (Fig. 9.7).
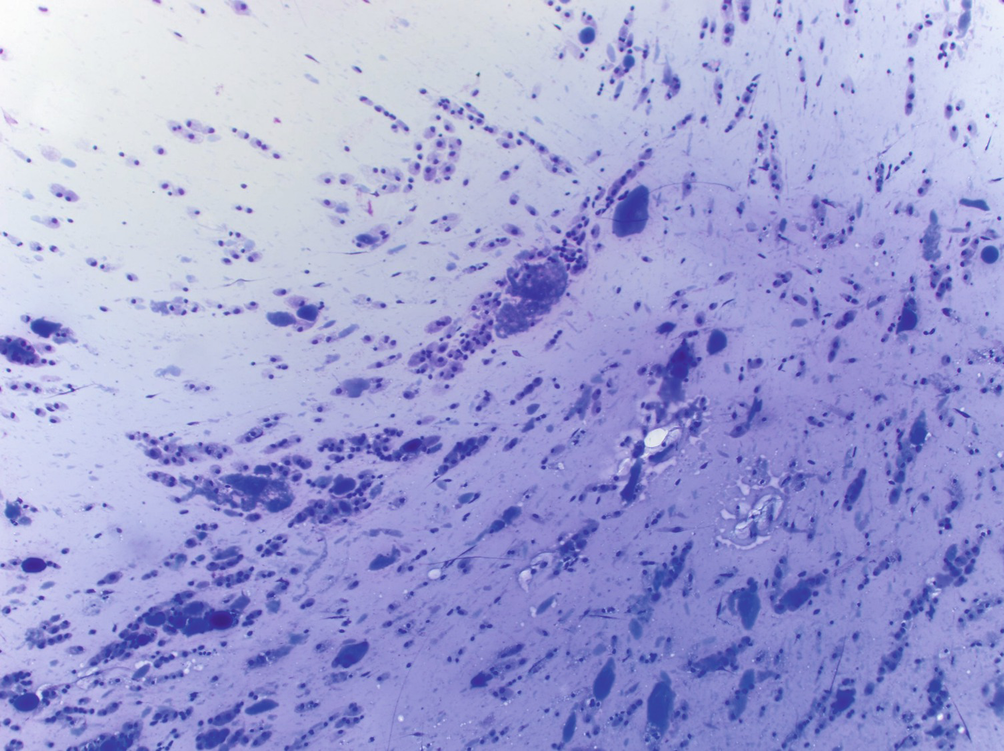
Sialocele : aspirates are hypocellular and contain abundant mucinous material. Scattered histiocytes are seen in the background
Comment
The main differential diagnostic consideration is low-grade mucoepidermoid carcinoma, which may also present as a predominantly cystic salivary gland mass. Any mucinous lesion with an epithelial component should prompt strong consideration of low-grade mucoepidermoid carcinoma. Even in cases in which only mucin is present in aspirate slides, a definitive diagnosis of sialocele should not be made.
Intraparotid Lymph Nodes
General Considerations
Lymph nodes are commonly present within the parotid gland and may be involved by reactive hyperplasia, lymphoma, or metastatic lesions.
A reactive intraparotid lymph node may present clinically as a parotid mass.
Submandibular lymph nodes may be mistaken for submandibular gland masses radiographically.
Ultrasound
The parotid gland is the only salivary gland to contain intraglandular lymph nodes. On US, they may appear as well-defined ovoid or round hypoechoic nodules with posterior sonographic enhancement and a central echogenic and central hilar vascularity on color Doppler imaging.
Computed Tomography
On CT, lymph nodes appear as intraparotid masses, slightly hyperdense to the parenchyma. A fatty hilum may be seen. Associated lymph node enlargement may be seen in the neck (Fig. 9.8).
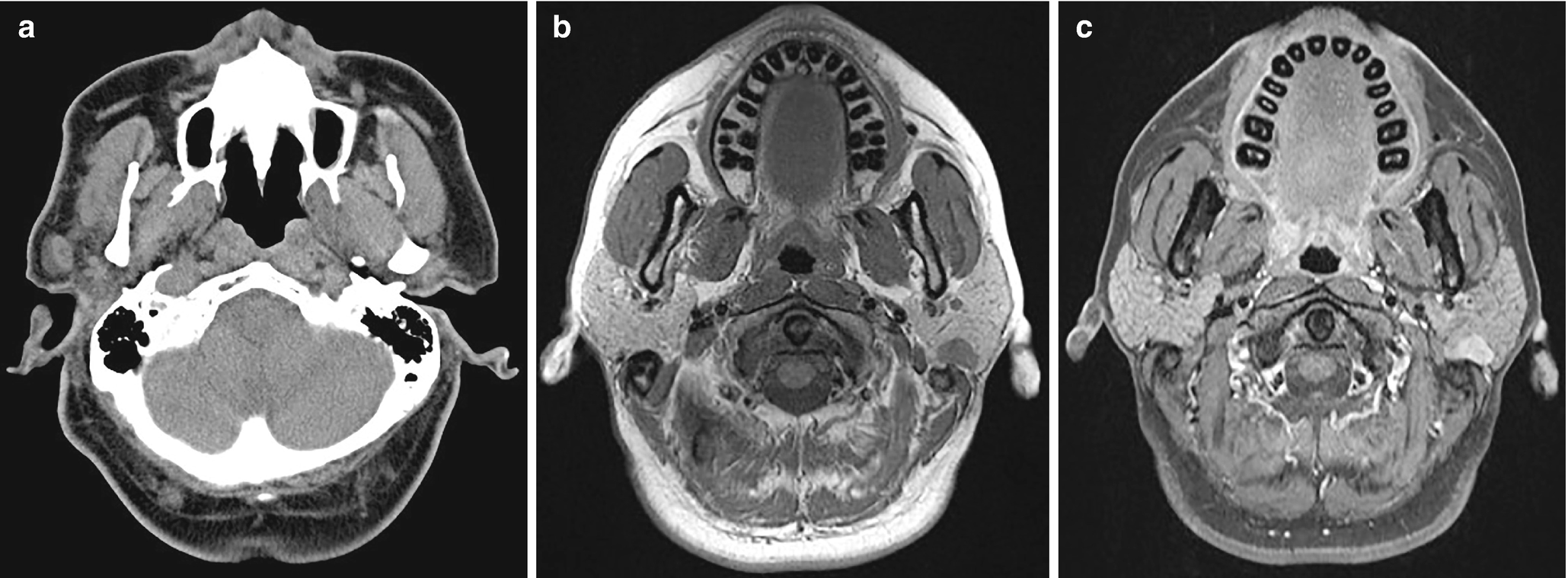
Intraparotid lymph node . (a) Axial CT demonstrates an oval right parotid gland lesion consistent with a lymph node. On MRI in another patient, a left parotid lymph node appears T1 hypointense (b) and enhances (c)
Magnetic Resonance Imaging
On MRI, lymph nodes are slightly T1 hypointense and enhance on the post-gadolinium images (Fig. 9.8).
Fine Needle Aspiration
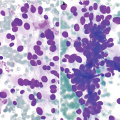
Aspirates from intraparotid lymph nodes demonstrate a polymorphous population of lymphoid cells, ranging from small lymphocytes to activated centroblasts and immunoblasts. Histiocytes, dendritic cells, and plasma cells may also be prominent (Fig. 9.9).
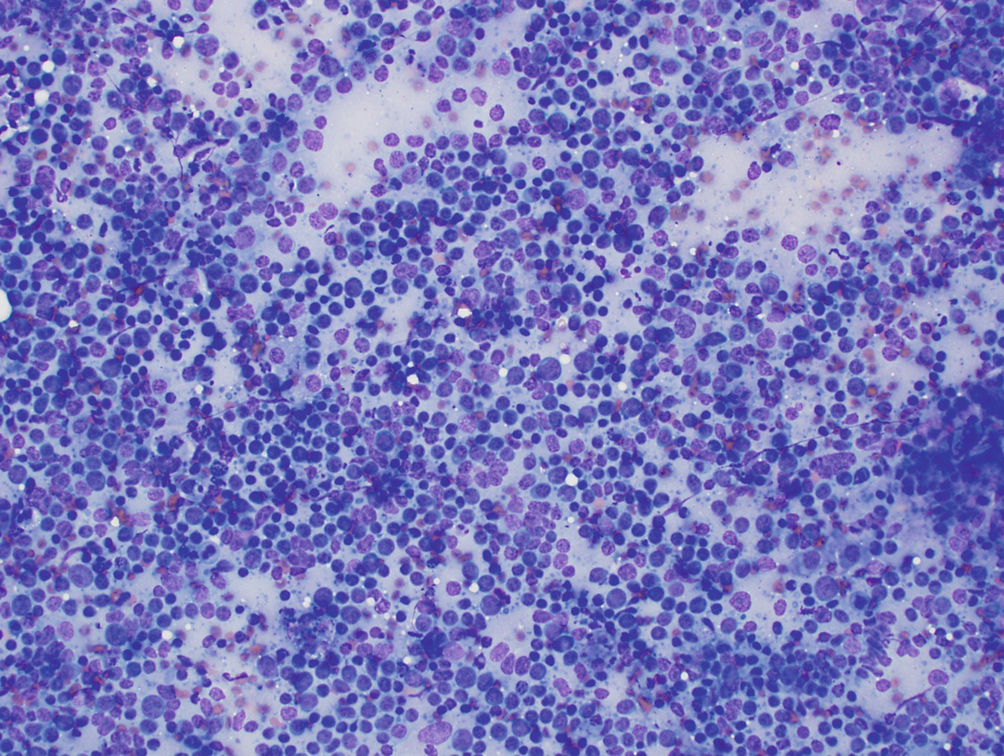
Reactive intraparotid lymph node . Aspirates are cellular and contain polymorphous round lymphoid cells with round nuclei of varying sizes. Numerous fragments of blue cytoplasm (lymphoglandular bodies) are seen in the background
Core Biopsy
Organized lymphoid tissue with germinal centers and histiocytic aggregates are typically seen in core biopsies of reactive lymph nodes.
Lymphoepithelial Lesions
General Considerations
Often slow growing and cystic with multilocular or unilocular growth.
May be associated with the human immunodeficiency virus (HIV) or autoimmune diseases.
Ultrasound
On US, there may be visualization of well-circumscribed cystic spaces; these may contain multiple small septations and commonly also small mural nodules.
Computed Tomography
The lesions may appear cystic with fluid attenuation (<20 Hounsfield units) or partly solid. These are typically multiple and bilateral (Fig. 9.10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree