Globe
Aqueous humor is secreted by the epithelium of the ciliary body, and is present in both the smaller anterior chamber and the larger posterior (vitreous) chamber of the globe. The globe is comprised of three concentric layers: the sclera, uvea, and retina. The sclera is the outermost layer and is composed of collagen-elastic tissue. The uvea is the middle layer, is vascular in nature (providing the vascular supply to the eye), and contains the iris, ciliary body, and choroid. The retina is the innermost layer, separated from the vitreous by the hyaloid membrane. The retina has two layers, the inner being the complex sensory layer and the outer being the retinal pigment epithelium.
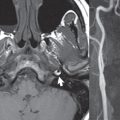
There are three potential spaces and, thus, three types of retinal detachment: that between hyaloid and sensory retina (the posterior hyaloid space), that between the sensory retina and retinal pigment epithelium (the sub-retinal space), and that between the choroid and the sclera (the suprachoroidal space). Posterior hyaloid detachment is seen in adults > 50 years of age, with macular degeneration. Separation of the sensory retina from retinal pigment epithelium produces the classic V-shape imaging appearance (of a retinal detachment), with convergence at the optic disc ( Fig. 2.44 ). Etiologies include masses (e.g., malignant melanoma), diabetes, inflammatory disease, trauma, and senile macular degeneration. Choroidal detachment can be due to surgery, trauma, or inflammatory disease, with the fluid either serous or hemorrhagic in nature. Retinal detachments are well-visualized on MR. Because of the high incidence of retinal detachments in older adults, a scleral buckle (placed to repair a retinal detachment) ( Fig. 2.45 ) is a common finding on screening CT (or MR) performed for other reasons.


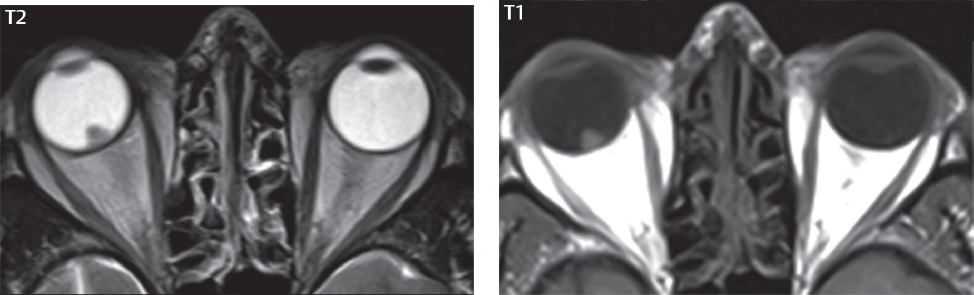
Retinoblastoma is the most common childhood intraocular tumor (98% of cases present before 6 months of age), often presenting with leukocoria. It is bilateral in 25 to 30%. Histologically these are primitive neuroectodermal tumors. The entity trilateral/quadrilateral retinoblastoma refers to a patient with bilateral retinoblastomas and an additional tumor in either the suprasellar and/or pineal region ( Fig. 2.46 ). Imaging is performed to look for retrobulbar spread, optic nerve invasion, and intracranial metastases. Both on ophthalmologic exam and imaging, a variety of benign mass lesions can mimic retinoblastoma. CT shows calcification (punctate or speckled) in more than 90% of retinoblastomas, in marked distinction to other intraocular lesions. On MR, retinoblastoma is visualized as a mass with short T1 and T2 (mildly hyperintense on T1 and hypointense on T2). Enhancement is typically moderate to marked ( Fig. 2.47 ). There are many uncommon, benign diseases that occur in the globe, some of which can mimic retinoblastoma, which are beyond the scope of this textbook. These include persistent hyperplastic primary vitreous, Norrie disease, Warburg syndrome, retinopathy of prematurity, Coats disease, and ocular toxocariasis.


Ocular choroidal melanoma and choroidal metastases ( Fig. 2.48 ) are usually diagnosed by ophthalmoscopy, which is true of all ocular tumors. Ocular melanoma is the most common primary intraocular neoplasm in adults, typically unilateral, with retinal detachment frequent. MR plays a limited role for characterization and definition of extent. Lesions that present for MR are usually small and mound-shaped with a broad choroidal base ( Fig. 2.49 ). Although choroidal melanomas are described as having a classic MR appearance, due to melanin, with marked hyperintensity on T1 and hypointensity on T2, this is observed in just slightly more than half of these tumors. Thus, differentiation on MR between choroidal metastases and melanomas is limited.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree