Presentation and Presenting Images
( ▶ Fig. 8.1, ▶ Fig. 8.2, ▶ Fig. 8.3, ▶ Fig. 8.4)
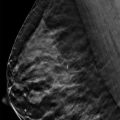
A 55-year-old female presents for screening mammography.
8.2 Key Images
( ▶ Fig. 8.5, ▶ Fig. 8.6, ▶ Fig. 8.7)
8.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
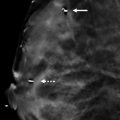
8.2.2 Imaging Findings
In the upper outer quadrant of the left breast at the 1 o’clock location in the posterior depth, there are grouped amorphous and round calcifications ( ▶ Fig. 8.5 and ▶ Fig. 8.6). The close-up of the calcifications on the mediolateral (MLO) view demonstrates their amorphous and loosely grouped appearance ( ▶ Fig. 8.7). They are difficult to localize to one digital breast tomosynthesis (DBT) slice in either imaging plane as they are loosely grouped. Comparison to earlier mammograms shows that these calcifications have been stable more than 5 years. The exam from 5 years ago was an analog mammogram and so not as easily reproduced. Therefore, the comparatives from 3 years ago are presented here as representative of the earlier mammograms showing the calcifications.
8.3 BI-RADS Classification and Action
Category 2: Benign
8.4 Differential Diagnosis
Benign calcifications: The punctate and amorphous calcifications are very loosely grouped and have been stable for more than 5 years. There are several areas of calcifications in the same breast that appear similarly.
Calcifications needing further evaluation: The stability of the calcifications suggest that they are benign and require no further evaluation.
Suspicious calcifications: Amorphous calcifications are part of the suspicious BI-RADS lexicon; however, some amorphous calcifications can be due to benign pathology. The stability of these calcifications suggests a benign etiology.
8.5 Essential Facts
DBT is not as good for identifying calcifications as it is for identifying masses and architectural distortion.
Only a few calcifications of a group of small and dispersed calcifications may show on a single reconstructed DBT slice.
Large calcifications can cause significant artifacts with repeating ghostlike objects bordered by dark shadows in the direction of the X-ray tube motion.
Spangler and colleagues (2011) noted that full-field digital mammography (FFDM) was significantly better for calcification detection than DBT (84% vs. 75%). In addition, FFDM had a higher specificity for calcifications over BDT (71% vs. 64%).
Kopans and colleagues (2011) noted that calcifications can be seen equally well if not with superior clarity on DBT compared to conventional mammography (this study used both analog and digital mammograms for comparisons).
Further research is needed to evaluate calcification detection on DBT.
8.6 Management and Digital Breast Tomosynthesis Principles
DBT slices are generally reconstructed as 1-mm slices; however, increasing the slice thickness may help the three-dimensional perception of calcifications. The trade-off is that the spatial resolution of the individual calcifications is decreased with the increased slice reconstruction thickness.
DBT slices are generally reconstructed as 1-mm slices. The thinness of the slices can cause calcifications in a group or a linear distribution to appear over several slices, thus not allowing the distribution of the individual calcifications to be observed in a single slice. The corresponding two-dimensional, conventional or synthetic mammogram may better provide this overview of calcifications. A synthesized view is a single two-dimensional (2D) image of the breast that is formed from either the projection images or the reconstructed slices. The synthesized view may serve as a surrogate for a conventional 2D mammogram.
8.7 Further Reading
[1] Conant EF. Clinical implementation of digital breast tomosynthesis. Radiol Clin North Am. 2014; 52(3): 499‐518 PubMed
[2] Kopans D, Gavenonis S, Halpern E, Moore R. Calcifications in the breast and digital breast tomosynthesis. Breast J. 2011; 17(6): 638‐644 PubMed
[3] Spangler ML, Zuley ML, Sumkin JH, et al. Detection and classification of calcifications on digital breast tomosynthesis and 2D digital mammography: a comparison. AJR Am J Roentgenol. 2011; 196(2): 320‐324 PubMed

Fig. 8.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree