Gynecologic Carcinoma
Takashi Nakano
Yoshiyuki Suzuki
Shingo Kato
Tatsuya Ohno
Thomas F. DeLaney
The combination of external beam radiotherapy and intracavitary brachytherapy is considered to be one of the standard treatment modalities for carcinoma of the uterine cervix. In early-stage disease, cervical cancer is highly curable by radiotherapy alone. However, the treatment results for locally advanced disease have been poor, with reported 5-year survival rates of 30% to 55% for stage IIIB, and 4% to 20% for stage IVA disease.1, 2, 3, 4, 5, 6 The major cause of death for patients with locally advanced cervical cancer is persistent or recurrent pelvic disease. Analyses of patterns of failure following radiotherapy in locally advanced disease report that 50% to 70% of the recurrences develop locoregionally and that locoregional recurrence rates increase with increasing tumor bulk.5,6
Clinical trials of combined chemotherapy and radiotherapy have been performed in an effort to improve the treatment outcomes for locally advanced cervical cancer. Several randomized phase III trials in the 1990s and a meta-analysis have demonstrated a survival advantage of approximately 10% for concurrent chemoradiotherapy when compared with radiotherapy alone.7, 8, 9 From the results of these studies, concurrent chemoradiotherapy has become the standard treatment for locally advanced cervical cancer.10 Nevertheless, the rates of locoregional control and overall survival for patients with stage III or IVA disease have remained unfavorable when compared with those for patients with stage IB to IIB disease.7,8
ADVANTAGES OF PARTICLE BEAM THERAPY
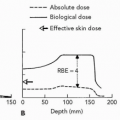
Charged particle radiation therapy has physical dose advantages over photons. This can be advantageous for management of the primary cervical tumor when a good brachytherapy implant cannot be achieved as well as for treatment of metastatic disease to the pelvic and paraaortic lymph nodes. This superior dose distribution may allow an improvement in local control while minimizing normal tissue damage. The radiobiologic similarity of protons to photons does allow physicians to draw upon a rich clinical experience with photons in treatment of cancer of the cervix in terms of dose and integration with chemotherapy. High-linear energy transfer (LET) charged particle therapy, however, may have additional advantages in terms of radiobiologic effects as well as dose distribution, and might offer a therapeutic gain over low-LET radiotherapy for some advanced cancers. The various biologic advantages of high-LET radiation including neutrons and heavy charged particles, can be summarized as a decreased oxygen enhancement ratio, a diminished capacity for sublethal and potentially lethal damage repair, and diminished cell cycle-dependent radiosensitivity.11,12 These biological properties may be advantageous in the treatment of hypoxic tumors or tumor types that are not well controlled with low-LET photons.13, 14, 15
NEUTRON THERAPY FOR CANCER OF THE UTERINE CERVIX
Radiation Therapy Oncology Group Study
A Radiation Therapy Oncology Group (RTOG) phase III study of neutron therapy for stage IIB to IVA cervical cancer was undertaken in the United States between 1976 and 1984.15 One hundred and fifty-six patients with locally advanced cervical cancer were entered into this study with the participation of five institutions. Patients were randomly assigned to receive photons with 50 Gy in 25 fractions over 5 weeks plus an intracavitary or external-beam boost versus mixed-beam radiotherapy with two fractions of neutrons a week, 3 fractions of photons a week to a total RBE-adjusted dose of 50 Gy (RBE) over 5 weeks plus an intracavitary
or external mixed-beam boost. Only patients with International Federation of Gynecology and Obstetrics (FIGO) stage IIB, III, or IVA squamous cell carcinoma with negative para-aortic nodes on lymphangiogram were eligible. One hundred and forty-six patients were analyzed, including 80 treated with mixed-beam radiotherapy and 66 with photons. Tumor clearance was 52% and 72% for mixed beam and photons, respectively (p <0.03). Local control rates at 2 years were 45% for mixed beam and 52% for photons. Severe complications in the mixed-beam and photon patients occurred in 19% and 11%, respectively (p <0.13). The inferior outcome with neutron therapy was attributed to the poor neutron dose distribution related to the use of horizontal neutron beams of varying energy and penetration.
or external mixed-beam boost. Only patients with International Federation of Gynecology and Obstetrics (FIGO) stage IIB, III, or IVA squamous cell carcinoma with negative para-aortic nodes on lymphangiogram were eligible. One hundred and forty-six patients were analyzed, including 80 treated with mixed-beam radiotherapy and 66 with photons. Tumor clearance was 52% and 72% for mixed beam and photons, respectively (p <0.03). Local control rates at 2 years were 45% for mixed beam and 52% for photons. Severe complications in the mixed-beam and photon patients occurred in 19% and 11%, respectively (p <0.13). The inferior outcome with neutron therapy was attributed to the poor neutron dose distribution related to the use of horizontal neutron beams of varying energy and penetration.
Calfornium-252 Neutron Brachytherapy for Cervical Cancer
Maruyama conducted clinical trials evaluating the neutron-emitting radioactive isotope, californium-252 (252Cf), for the treatment of cervical cancer beginning in 1976.13,14 The first protocol employed 50 to 55 Gy of whole pelvis photon irradiation followed by one to two 252Cf insertions using a single tandem placed in the uterocervicovaginal region. A biologically equivalent dose to point A by 252Cf of 10 to 15 Gy (RBE) was used; the relative biological effectiveness (RBE) for neutrons in this study was set at 6. A total of 218 patients were treated in the initial study period from 1976 until 1983. These studies included stage III and IV advanced cervical cancer patients. The 2- and 5-year survival rates of patients treated with neutron therapy were 53% and 36%, which were not significantly different from those obtained with photon brachytherapy (2-year survival, 61%; 5-year survival, 34%). Complications of neutron therapy were minimal and included proctitis (19%) and vaginal stenosis (9%).13 However, Maruyama reported superior 5-year survival rates for neutron brachytherapy compared to conventional photon therapy in stage III patients14 and noted that application of neutrons early in the treatment course resulted in superior local control when compared to later neutron treatment.13 The proposed reason for this improved outcome was the biologic advantage of high LET and concentrated dose distribution by the use of brachytherapy. In contrast, stage IV disease did not appear be well suited for this approach because of the high incidence of distant metastases and difficulty covering the entire extent of pelvic tumor by an adequate implant dose with the 252Cf insertion.
The Phase I&II Study of Neutron Therapy for the Uterine Cervix at the National Institute of Radiological Sciences
A semirandomized trial of fast neutron therapy for locally advanced or radioresistant malignant tumors was undertaken in November 1975 at the National Institute of Radiological Sciences (NIRS).16 To evaluate the effectiveness of mixed fast neutron-photon fractionated irradiation on squamous cell carcinoma of the uterine cervix, 98 patients with stage IIIB disease were enrolled in the study. The whole pelvis was irradiated with 50 to 55 Gy of conventional megavoltage x-rays in the photon arm and with 50 to 55 Gy (RBE) with mixed beams of neutrons and photons in the neutron arm. Subsequently, all patients in both arms then received intracavitary irradiation with a remote after-loading system delivering 11 to 13 Gy to point A. The local control rate after neutron-mixed beam therapy was 73%, which was not significantly superior to the 66% rate seen with photon irradiation. The 5-year survival rate of 49% for patients treated with neutron therapy was the same as those with photon therapy. The absence of significant benefit was attributed to an inferior dose distribution of the neutron beams compared to that of photons, resulting in no additional therapeutic benefit.
PROTON BEAM IRRADIATION FOR CANCER OF THE CERVIX
Treatment Planning Studies
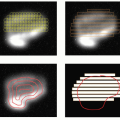
Slater et al. performed comparative treatment planning studies comparing photon and proton irradiation for management of carcinoma of the cervix.17 Several scenarios were evaluated. In the first scenario, patients were to be treated with 50 Gy of external beam pelvic irradiation, intracavitary brachytherapy, and an external beam parametrial boost. The comparative dose distributions showed the proton beam avoiding more of the bladder, small bowel, and rectum than the photon boost while still covering the lateral parametria. In the second scenario, patients who were not candidates for intracavitary therapy because of tumor bulk or poor geometry were treated with external beam only. In this second scenario, dose to the tumor could be increased within normal tissue tolerance to 80 to 90 Gy (RBE) with protons, whereas dose with three-dimensional (3-D) conformal photons was limited to approximately 70 Gy.
Similar findings were reported by Smit who performed treatment planning studies comparing intracavitary brachytherapy combined with either 3-D photons or protons.18 The protons were delivered through a split posterior and two lateral fields. His study suggested that the volume of normal tissue irradiated to significant dose could be reduced by up to 60% with protons compared to photons, allowing tumor doses of up to 20% higher. Assuming a gamma factor of 2,19 this would translate into a 40% improvement in local control using protons compared to 3-D photons.
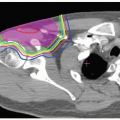
Levin studied the potential for gain in the use of a proton beam boost to the para-aortic lymph nodes in the management of carcinoma of the cervix.20 Delivery of two-dimensional (2-D) or 3-D conformal photon doses >50 Gy to the para-aortic lymph nodes has been associated with an unacceptable risk of small bowel morbidity.21,22
Levin found that the use of protons would allow safe dose escalation to the para-aortic lymph nodes to 70 Gy (RBE) with acceptable doses to bowel and other sensitive structures. He estimated that this increase in dose might improve disease-free survival by 11% in stage II and as much as 21% in stage III disease.
Levin found that the use of protons would allow safe dose escalation to the para-aortic lymph nodes to 70 Gy (RBE) with acceptable doses to bowel and other sensitive structures. He estimated that this increase in dose might improve disease-free survival by 11% in stage II and as much as 21% in stage III disease.
Clinical Results
The Tsukuba group reported on the results of combined photon-proton irradiation of 19 patients with uterine cervical carcinoma.23 Patients were treated with external irradiation only. They treated 19 patients, 8 of whom had stage IIB disease and 11 of whom had stage IIIB disease. Whole pelvis irradiation was initially given through parallel opposing 10-MV photons to a dose of 50.4 Gy in 28 fractions. After 0 to 45 Gy (median 25 Gy), the central target volume as determined by computed tomography (CT) scan was blocked and this volume was irradiated with proton beams through anterior and lateral portals. Proton doses of 46 to 63 Gy (mean 58.0 Gy) at 2.6 to 3.8 Gy (mean 3.3 Gy) were delivered because of the limited availability of beam time and the preference of the attending physicians. The total dose to the primary tumor from the combination of photons and protons ranged from 79 to 92 Gy (mean 85.0 Gy). Proton doses quoted were physical Gy without any RBE correction. Local failures occurred in two patients (10.5%) who had stage IIIB tumors, but no local failures occurred in the patients with stage IIB disease. The actuarial survival rates at 3 years were 87.5% for stage IIB and 75.8% for stage IIIB patients. Two patients developed major radiation related proctitis, but neither required surgical intervention and eventually became symptom-free with conservative measures. Radiation cystitis was described as minimal to moderate.
Kagei et al.24 recently updated the Tsukuba series and included an additional six patients. These 25 patients were treated between 1983 and 1991 using the techniques described in the preceding text. There were 9 stage IIB patients, 15 stage IIIB patients, and one stage IVA patient. In this updated group, a median physical proton tumor dose of 61 Gy (range 37 to 101 Gy) was delivered in three to four fractions weekly, with doses per fraction varying from 2.5 to 4 Gy. The median combined total photon/proton tumor dose was 86 Gy (range 71 to 101 Gy). When the authors converted these doses to conventionally fractionated radiation given at 2 Gy q.d. using the linear quadratic formula with an α/β = 10 for acute effects and α/β = 3 for late effects, the equivalent total doses in conventional fractionation were 92 Gy (range 74 to 118 Gy) and 99 Gy (range 78 to 114 Gy), respectively. For the proton component, the median equivalent doses were 68 Gy (range 41 to 118 Gy) and 78 Gy (range 46 to 142 Gy), respectively.
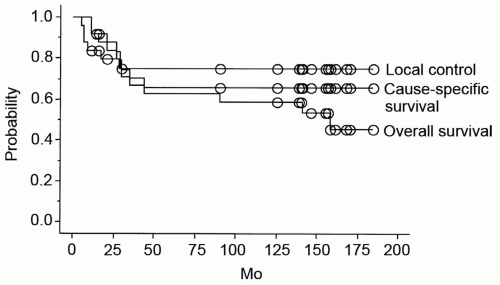
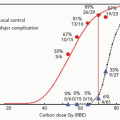
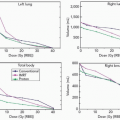
With a median duration of follow-up after the start of radiotherapy of 90 months (range 11 to 161 months), the overall and cause-specific survival were 59% and 65%, respectively (see Fig. 20.1). Overall survival rates for stages IIB and IIIB/IVA patients at 10 years were 89% and 40%, respectively. Six patients developed local recurrences that occurred within 28 months of irradiation. No patient with stage IIB disease suffered a local recurrence. Five-year local control rates for all (Fig. 20.1), stage IIB, and stage IIIB/IVA patients were 75%, 100%, and 61% respectively. Five patients, none with stage IIB, developed distant metastases. Rates of freedom from distant metastases at 5 years for all, stage IIB, and stage IIIB to IVA patients were 79%, 100%, and 66% respectively. A combined equivalent dose (2 Gy, α/β = 10) of >92 Gy was associated with a trend toward a higher rate of local control at 5 years (85% vs. 59%, p = 0.08) and improved survival (84% vs. 42%, p = 0.013).
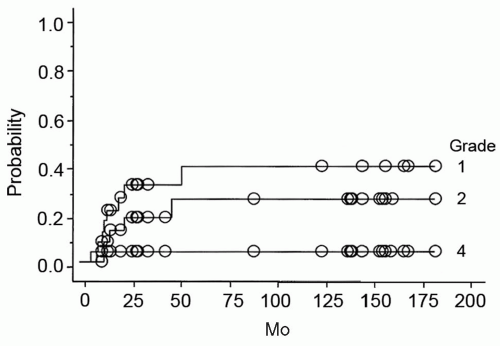
Acute reactions were not significant; one patient developed diarrhea requiring a 3-day treatment break but no other patients required a treatment interruption. Treatment complications are shown in Table 20.1. Approximately half of the patients developed late complications in the small or large bowel, predominantly rectal bleeding and 20% of the patients sustained late urinary bladder complications. Most complications were grade 1 to 2 but one patient developed grade 4 intestinal and bladder complications after receiving an equivalent dose based on an α/β = 10 and α/β = 3 of 93 and 102 Gy respectively. The patient developed severe hemorrhagic cystitis requiring transurethral hemostatic intervention and arterial embolization followed later by intestinal obstruction managed by small bowel resection 86 months after irradiation. No grade 5 complications were seen. The late complications appeared 6 to 53 months after irradiation. The actuarial rates of grade 1, 2, and 4 complications at 5 years were 43%, 26%, and 4% respectively (see Fig. 20.2). Combined equivalent doses (2Gy, α/β = 3) of >102 Gy were associated with more late bowel or bladder complications (49% at 5 years) when compared
to those receiving lower doses (11%), p = 0.06. A similar trend was seen for proton equivalent doses (2 Gy, α/β = 3) >78 Gy with complications at 5 years of 51% compared to 10% for lower doses, p = 0.04.
to those receiving lower doses (11%), p = 0.06. A similar trend was seen for proton equivalent doses (2 Gy, α/β = 3) >78 Gy with complications at 5 years of 51% compared to 10% for lower doses, p = 0.04.
TABLE 20.1 CRUDE INCIDENCE OF LATE COMPLICATIONS IN THE SMALL/LARGE BOWEL OR THE URINARY BLADDER IN PATIENTS TREATED WITH COMBINED PHOTON/PROTON RADIOTHERAPY AT TSUKUBA UNIVERSITY IN JAPAN | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
These results are comparable to those achieved with external beam photon irradiation and intracavitary insertion and suggest the proton irradiation would be an appropriate alternative for patients who are not candidates for intracavitary treatment. Because of the relatively small numbers of patients treated, optimal doses and schedules have not yet been defined but there is a suggestion of a dose window where local control can be improved with higher dose within a tolerable risk of normal tissue complications. These results were achieved with irradiation alone without chemotherapy. Proton treatments in the future are likely to be combined with chemotherapy; substituting protons for photons in combined chemoradiation approaches that might reduce both the acute and late morbidity of chemoradiation.
CARBON ION IRRADIATION FOR CANCER OF THE CERVIX
Conventional intracavitary brachytherapy using tandem and ovoid cannot deliver an adequate dose for patients with bulky tumors and/or extensive parametrial involvement, resulting in an unfavorable treatment outcome for these patients. Hence, combined intracavitary and interstitial brachytherapy has been used to improve the dose distribution for patients with locally advanced bulky cervical cancer,25 but this treatment is technically challenging. The potential biologic advantages of higher LET particles were not realized with external beam neutrons because of the poor physical dose distribution. If high-LET biology could be combined with a superior physical dose distribution, an improvement in local control in patients with locally advanced cervical cancer might be realized. Therefore, patients with stage III bulky and stage IVA cervical cancers were considered to be appropriate for inclusion in phase I and II clinical studies of heavy charged particle radiation. These patients had not been included in the studies of high-LET charged particle therapy using neons, which were performed at the Lawrence Berkley Laboratory.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree