FIGURE 1.1
FINDINGS Posteroanterior (PA) radiographs of both hands. On the left side, sausage-digit soft tissue swelling involves the entire index finger. The other fingers are normal. There is a single erosion at the metacarpophalangeal (MCP) joint of the index finger at the radial aspect of the proximal phalanx, and fluffy periostitis is present adjacent to the proximal interpha-langeal (PIP) and distal interphalangeal (DIP) joints. Overall bone mineralization is preserved, and there is no abnormality of alignment or narrowing of the cartilage spaces. On the right side, the ring finger shows sausage-digit soft tissue swelling. There are erosions at the PIP and DIP joints and periostitis.
DIFFERENTIAL DIAGNOSIS Psoriatic arthritis, erosive osteoarthritis, rheumatoid arthritis, gout.
DIAGNOSIS Psoriatic arthritis.
DISCUSSION Sausage-digit soft tissue swelling is characteristic of diffuse inflammation, raising the possibility of cellulitis and underlying osteomyelitis as well as one of the seronegative spondyloarthropathies such as psoriatic arthritis. This pattern of swelling, reflecting involvement of the tendons and ligaments as well as the joint capsules, is different from the fusiform soft tissue swelling that is characteristic of effusion or synovial joint inflammation. The presence of erosions, as well as the fluffy periostitis, is pathognomonic for an inflammatory process. In this case, the periostitis is more evident when the cortex and shapes of the abnormal bones are compared with that of their normal neighbors. The distribution of involvement—a single, entire digit, with normal adjacent digits—is characteristic of psoriatic arthritis. Early changes of psoriatic arthritis may precede or follow dermatologic manifestations of psoriasis, sometimes by many years. Although many patients have relatively indolent arthritic changes, some patients may have a very aggressive, deforming, and disabling arthritis for which early, aggressive treatment is indicated [1].
CASE 1.2 CLINICAL HISTORY
A 55-year-old man with rash.
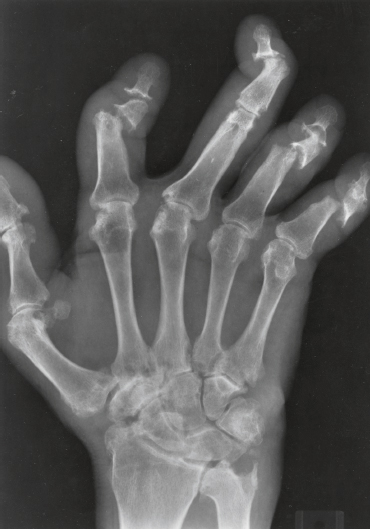
FIGURE 1.2
FINDINGS PA radiograph of the right hand. Polyarticular arthritis is distributed through the entire hand and wrist. The DIP and PIP joints of all the fingers are severely involved, with erosions of the articular ends of the bones resulting in complete loss of cartilage and subarticular bone. Several joints have pencil-in-cup deformities. There is pancompartmental involvement of the wrist, with erosions and mature periosteal new bone. The periosteal bone is best seen at the ulnar styloid processes. The contralateral hand has a similar appearance.
DIFFERENTIAL DIAGNOSIS Psoriatic arthritis, erosive osteoarthritis, rheumatoid arthritis, gout.
DIAGNOSIS Psoriatic arthritis, arthritis mutilans appearance.
DISCUSSION Psoriasis is a common, genetically predisposed skin disease characterized by dry, pink, scaly, nonpruritic lesions. Psoriatic arthritis is an inflammatory arthropathy associated with psoriasis and characterized by the absence of rheumatoid factor [2]. As many as 5% of patients with psoriasis have an associated arthritis. Psoriatic arthritis has five patterns of clinical presentation: (1) asymmetric oligoarthritis, seen in more than 50% of cases; (2) polyarthritis with predominantly DIP involvement, of which the classic presentation is seen in 5% to 19% of cases; (3) symmetric seronegative polyarthritis simulating rheumatoid arthritis, seen in up to 25% of cases; (4) sacroiliitis and spondylitis resembling ankylosing spondylitis, seen in 20% to 40% of cases; and (5) arthritis mutilans with resorption of phalanges, seen in 5% of cases. Individual patients may progress from one clinical pattern to another. The dominant radiologic features in this case—erosions and periostitis—are those of inflammatory arthritis [3]. The features of degenerative joint disease—osteophytes, subchondral sclerosis, and asymmetric joint space loss—are conspicuously absent. The preservation of normal bone mineralization mitigates against rheumatoid arthritis, in which profound osteoporosis is an invariable feature in chronic, severe disease. The greater severity of interphalangeal (IP) joint involvement, compared with carpal and MCP joint involvement, favors psoriatic arthritis over rheumatoid arthritis. The complete erosions of the articular ends of the phalanges and the involvement of the DIP joints are characteristic of the arthritis mutilans pattern of peripheral psoriatic arthritis.
CASE 1.3 CLINICAL HISTORY
A 55-year-old woman with stiff hands.

FIGURE 1.3A

FIGURE 1.3B
FINDINGS PA (A) and lateral (B) radiographs of the left hand. Arthritic changes involve the PIP and DIP joints of the fingers and the IP, MCP, and basal joints of the thumb. These changes are characterized by bony hypertrophy, with large osteophytes and subchondral sclerosis. The cartilage spaces are narrowed asymmetrically. Mineralization of the hand is normal. Soft tissue swelling is not prominent, and there are no erosions.
DIFFERENTIAL DIAGNOSIS Osteoarthritis, pyrophosphate arthropathy.
DIAGNOSIS Primary osteoarthritis.
DISCUSSION The presence of hypertrophic degenerative changes at the basal joint of the thumb (first carpometa-carpal joint and scaphoid-trapezium-trapezoid joints) is generally seen only in primary osteoarthritis. Involvement of the PIP and DIP joints is also characteristic. Soft tissue swelling, juxta-articular osteoporosis, erosions, and ankylosis should be absent, unless inflammatory changes are also present. Osteoarthritis is the most common form of poly articular arthritis. Its prevalence increases with age, so that it is nearly ubiquitous in patients older than 65. In addition to the hand, other common sites of osteoarthritis include the hip, the knee, the first metatarsopha-langeal joint, and the synovial joints of the cervical and lumbar spine. The early morphologic abnormality in osteoarthritis is fibrillation of the surface of the articular cartilage, reflecting disruption of the molecular structure of the cartilage. Progressive mechanical erosion of the cartilage, thinning of the cartilage, and formation of fissures will eventually expose the subchondral bone. An adaptive response of osteophyte formation and subchondral sclerosis, combined with asymmetric cartilage space narrowing, results in the characteristic radiographic appearance [4]. In pyrophosphate arthropathy, involvement of the MCP and radial-carpal joints is more typical.
CASE 1.4 CLINICAL HISTORY
A 58-year-old woman with arthritis.

FIGURE 1.4A

FIGURE 1.4B
FINDINGS (A, B) PA radiographs of both hands. There is poly articular disease with asymmetric joint space narrowing, osteophytes, and subchondral sclerosis. The predominant sites of involvement are the IP joints and the basal joints of the thumb, with sparing of the MCP and radiocarpal joints. A seagull appearance is present at the PIP joints of the middle, ring, and little fingers. Bone mineralization is normal.
DIFFERENTIAL DIAGNOSIS Osteoarthritis, erosive osteoarthritis, psoriatic arthritis, pyrophosphate arthropathy.
DIAGNOSIS Erosive osteoarthritis.
DISCUSSION The presence of osteophytes and subchondral sclerosis indicates a degenerative form of arthritis. The particular distribution of involvement is characteristic of osteoarthritis (IP joints, basal joint of the thumb). Although joint degeneration always has some component of synovial inflammation because of the presence of joint debris and cartilage breakdown products, when the inflammation has erosive changes that dominate the clinical presentation, the condition may be called erosive osteoarthritis [5]. Radiographs show the degenerative features and distribution of primary osteoarthritis, but the acute synovitis causes inflammatory erosions, uniform joint space narrowing, and sometimes ankylosis. A characteristic “gull-wing” appearance may be seen on PA radiographs at the IP joints of the fingers, corresponding to central erosions and bony hypertrophy [6]. The typical patient is a postmenopausal woman (female-to-male ratio of about 12:1). The inflammation usually subsides within a few months to a couple of years, leaving the residual degenerative changes. Although psoriatic arthritis may have a similar distribution, the presence of subchondral sclerosis and osteophytes eliminates psoriatic arthritis as a diagnostic consideration.
CASE 1.5 CLINICAL HISTORY
A 33-year-old woman with continued pain, redness, and swelling, Radiographs at presentation, after 2 months, and after 9 months.
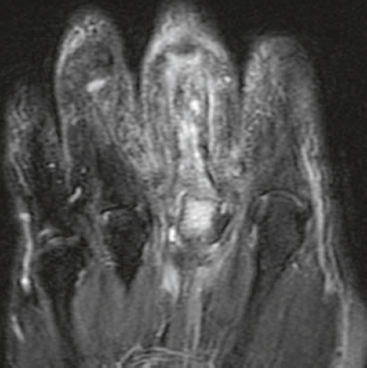
FIGURE 1.5A
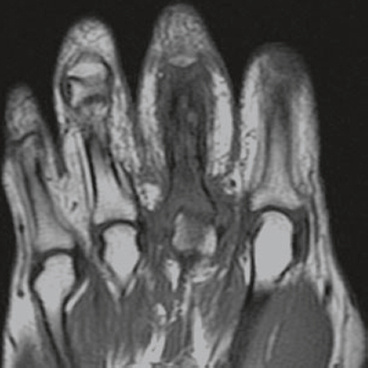
FIGURE 1.5B
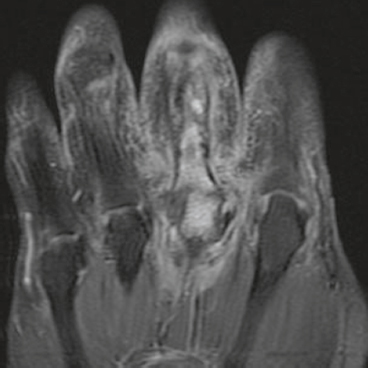
FIGURE 1.5C
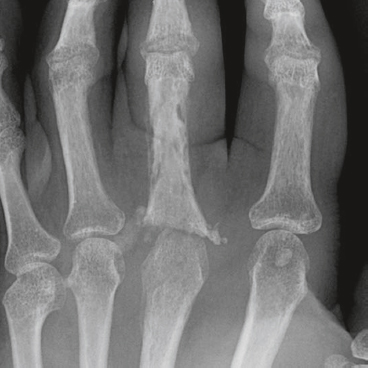
FIGURE 1.5D
FINDINGS
- Coronal T2-weighted fat-suppressed MRI shows fluid signal within the proximal phalanx of the middle finger and head of the third metacarpal and surrounding soft tissue edema.
- Coronal T1-weighted MRI shows low marrow signal corresponding to the fluid signal demonstrated on the T2-weighted images, with irregularity of the bony contours of the proximal phalanx of the middle finger.
- Coronal T1-weighted fat-suppressed MRI following intravenous gadolinium injection shows enhancement of the involved bones and surrounding soft tissues.
- AP radiograph shows destructive and reactive changes in the proximal phalanx of the middle finger and third metacarpal head. A thin layer of periosteal bone surrounding the proximal phalanx represents involucrum; the relatively dense bone within represents sequestrum. The adjacent bones show acute osteoporosis.
DIFFERENTIAL DIAGNOSIS Osteomyelitis, fracture healing.
DIAGNOSIS Osteomyelitis.
DISCUSSION Infection following open fractures is a known and feared complication. The likelihood of infection depends primarily on the degree of tissue damage sustained during the trauma, the size of the open wound, the severity of contamination, and the effectiveness of treatment [7]. On MRI, one generally expects to see low signal within the affected marrow on T1-weighted images, bright signal on T2-weighted or STIR images [8], and enhancement following gadolinium [9]. Features such as involucrum, sequestrum, abscess, and draining sinus may be present. Diagnostic accuracy is greatly improved in the proper clinical setting and decreased in the presence of confounding conditions such as fracture healing [10]. In this case, the clinical setting suggests infection, and the radiographs are confirmatory.
CASE 1.6 CLINICAL HISTORY
A 50-year-old immunocompromised man with deformed, tender, swollen thumb. Radiographs at presentation, after 2 months, and after 9 months.

FIGURE 1.6A
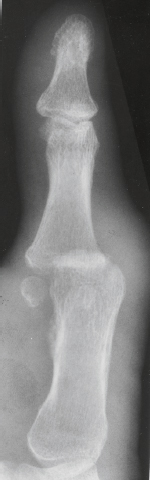
FIGURE 1.6B

FIGURE 1.6C
FINDINGS
- Lateral radiograph demonstrates soft tissue swelling and erosion of the articular surfaces of the first MCP joint. The surfaces of the erosions have indistinct margins. Volar subluxation is present.
- Oblique radiograph taken 2 months after presentation demonstrates increased reactive bone at the articular erosions and metadiaphyseal periostitis.
- Lateral radiograph taken 9 months after initial presentation, following treatment, demonstrates smooth, amputated, well-corticated margins with resolved periostitis.
DIFFERENTIAL DIAGNOSIS Osteomyelitis, septic arthritis, tuberculous arthritis, psoriatic arthritis.
DIAGNOSIS Tuberculous arthritis.
DISCUSSION The images in this case document a slowly destructive arthritis of a single joint that healed without ankylosis. Tuberculous arthritis may be caused by direct extension from tuberculous osteomyelitis of initial seeding of the synovium, generally from a preexisting focus of infection of the lung. The overgrowth of granulation tissue from the synovium extends into the joint, destroying both the articular cartilage and the subchondral bone. There is virtually no reactive bone formation. Although fibrous ankylosis may result, bony ankylosis ordinarily does not. The process may be protracted and evolve with only mild symptoms occurring over a period of months. Tuberculous arthritis is an unusual form of extrapulmonary tuberculosis, appearing in no more than 1% of patients with tuberculosis. Both Mycobacterium tuberculosis as well as atypical mycobacteria may be the infective agents. Often seen in association with human immunodeficiency virus (HIV) infection, patients with tuberculous arthritis who are not infected with HTV are usually adults between 30 and 60 years of age. Predisposing factors for joint involvement include joint trauma, systemic disease such as diabetes melhtus, intravenous drug abuse, intra-articular corticosteroid injection, and HIV infection. HIV specifically eliminates the tissue macrophages and CD4 lymphocytes that provide immunity against tuberculosis; therefore, it is not surprising that tuberculosis, one of the more virulent of opportunistic infections, appears fairly early in HIV disease and is becoming much more common [11]. A large proportion of patients who are infected with tuberculosis will also be seropositive for HIV, and patients with tuberculosis are more likely to have extrapulmonary involvement if they are seropositive for HIV [12].
CASE 1.7 CLINICAL HISTORY
A 63-year-old woman with chronic cough.

FIGURE 1.7
FINDINGS Detail of thumb reveals mixed lytic and permeative destruction of the distal phalanx with associated soft tissue swelling. The joint space is preserved.
DIFFERENTIAL DIAGNOSIS Infection, trauma, squamous cell carcinoma, metastases, melanoma.
DIAGNOSIS Lytic metastasis (lung carcinoma).
DISCUSSION The radiographic appearance is that of an aggressive bone-destroying lesion. Differential diagnostic considerations might include infection, but one might expect an infection to spread into the joint space and involve the adjacent bone. Metastases to the hands and feet, particularly the digits, are uncommon. Location in the distal phalanx of a digit, or in a subungual location, is rare [13] and is associated with a poor prognosis. Phalangeal metastases commonly display inflammatory symptoms that may mimic an acute infection [14]. They may also present as onycholysis (detachment of a nail plate from its distal and lateral attachments) [15]. The most common responsible primary sites are lung, kidney, and breast, and in 44% of patients with subungual metastases, this was the presenting symptom [16]. The most common primary malignant lesions of the distal phalanges are epidermoid carcinoma and malignant melanoma. External cortical erosions radiographically characterize primary nail bed lesions, whereas metastatic lesions tend to show extensive permeated destruction [17].
CASE 1.8 CLINICAL HISTORY
A 28-year-old woman with slowly enlarging mass at the tip of her index finger; it is painful when she bumps it.
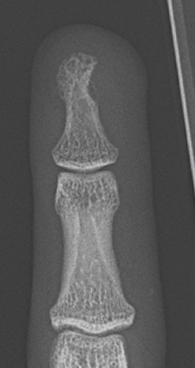
FIGURE 1.8A
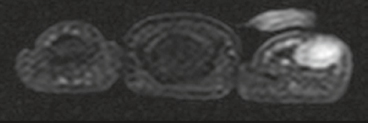
FIGURE 1.8B
FIGURE 1.8C
FIGURE 1.8D
FINDINGS
- PA radiograph of the index finger demonstrates soft tissue fullness corresponding to the mass, with smooth erosion of the underlying phalangeal tuft.
- Axial STIR MRI shows a soft tissue lesion abutting and eroding the distal phalanx. The lesion has high signal.
- Axial Tl-weighted MRI shows intermediate signal within the lesion.
- Axial Tl-weighted fat-suppressed MRI following intravenous gadolinium shows intense enhancement throughout the lesion.
DIFFERENTIAL DIAGNOSIS Glomus tumor, epidermoid inclusion cyst, foreign body granuloma, periosteal chondroma, sarcoma.
DIAGNOSIS Glomus tumor.
DISCUSSION Locating the lesion in the subungual soft tissues rather than within the bone is key to approaching the diagnosis. Although the differential diagnosis would include foreign body granuloma, epidermoid inclusion cyst, enchondroma, and sarcoidosis, the clinical presentation suggests the correct diagnosis. Glomus tumors are hamartomas that arise from the neuromyoarterial glomus, a normal, specialized vascular anastomotic complex surrounded by nerve elements [18]. Located in diverse internal organs and in the dermis and superficial subcutaneous tissues in the extremities, particularly around the fingertips, the neuromyoarterial glomus functions in the regulation of body temperature. Glomus tumors are typically small, soft tissue lesions that are highly vascular. In the fingers, most are located in the sub-ungual region, with the remaining located in the pulp [19]. Radiographically, they produce shallow erosions in adjacent bone. Direct demonstration by magnetic resonance imaging (MRI) has been described, and multiple lesions may occur [20]. Intraosseous glomus tumors are rare. Complete surgical excision is curative.
CASE 1.9 CLINICAL HISTORY
A 43-year-old construction worker with chronically swollen finger.

FIGURE 1.9A

FIGURE 1.9B
FINDINGS
- PA radiograph of the finger shows a round lucent lesion in the distal phalanx with a well-defined sclerotic margin. The lesion is slightly eccentric in location.
- Lateral radiograph shows a subungual soft tissue mass raising the nail bed and eroding the dorsal surface of the cortex of the distal phalanx.
DIFFERENTIAL DIAGNOSIS Glomus tumor, epidermoid inclusion cyst, foreign body granuloma, enchondroma, sarcoidosis.
DIAGNOSIS Epidermoid inclusion cyst.
DISCUSSION Bone cysts lined with epidermis are uncommon and are found only in the skull and the distal phalanges. Epidermoid inclusion cysts are posttraumatic lesions that result from penetrating trauma in which dermoid elements are implanted into the bone [21,22]. Growth of these elements results in a slowly enlarging cyst filled with desquamated keratin flakes, sebaceous material, and foreign-body reactive tissue and debris. Nearly all lesions involving the phalanges are reported to be in the hand. In the majority of cases, a definite history of trauma to the affected finger exists. The typical injury is a fairly severe crushing wound to the fingertip. Men are affected more frequently than women by a 2:1 ratio. The episode of trauma may have occurred decades before presentation, often when the patient was a child or young adult. Epidermoid inclusion cysts present clinically with swelling, often with associated redness and tenderness. They may occasionally be asymptomatic. The classic radiologic appearance is a clear-cut, lucent, rounded lesion with a sclerotic rim, causing destruction and expansion of the phalanx. Sometimes a retained foreign body, implanted at the time of trauma, will be visible [23]. Treatment is surgical excision or curettage; amputation is generally not required.
CASE 1.10 CLINICAL HISTORY
A 50-year-old woman with bilateral hand deformities.

FIGURE 1.10
FINDINGS PA radiograph of both hands shows destructive changes involving the phalanges of all the fingers, with a lace-like appearance. The bone has remodeled, and the less involved regions (metacarpals, carpals, and distal forearm) are osteopenic. The soft tissues are not swollen.
DIFFERENTIAL DIAGNOSIS Sarcoidosis, hemangiomatosis, enchondromatosis, tophaceous gout.
DIAGNOSIS Sarcoidosis.
DISCUSSION Sarcoidosis may involve the joints in about 10% of cases, but sarcoidosis most often causes transient migratory polyarticular arthralgias without radiographic findings. A chronic granulomatous arthritis develops in only a few patients, leading to chronic noncaseating granulomatous inflammation of the synovium. Granulomas within or adjacent to the bone may result in punched-out cortical erosions or central lytic lesions with nonaggressive features within the medullary cavity. The process appears not to provoke reactive bone, and the remaining portions of cortex and trabeculae become reinforced and thickened. The middle and distal phalanges of the fingers are the typical sites of involvement. The characteristic appearance caused by the presence of multiple granulomatous lesions has been described as lace-like, latticework, or honeycomb. The most common radiographic appearance in bone is lace-like or honeycomb involvement of the hands or feet. Cyst-like lesions in bone are, in fact, bone that has been replaced by solid sarcoid granulomas, and are not actually cysts. Soft tissue involvement by sarcoid may occur in one-third of patients. The hand, bone, muscle, tendon, cutaneous or subcutaneous tissue, or synovium may be involved [24,25]. The natural history of sarcoid bone lesions is variable, ranging from rare cases of recovery to gradual progression and eventual autoamputation. Treatment with systemic corticosteroids may result in improvement or stabilization of bone lesions, but bone usually does not return to normal.
Radiologic appearances consist of cyst-like lesions, a lace-like pattern, or extensive bone destruction. Asymmetric soft tissue swelling may be present. Enlargement of the fingertips may result in an appearance on physical examination described as “pseudoclubbing” and reflects phalangeal involvement [26].
CASE 1.11 CLINICAL HISTORY
A 29-year-old woman who was in an accident 2 years ago.

FIGURE 1.11
FINDINGS PA radiograph of the hand shows loss of the distal portions of the fingers. The margins of the bone loss are corticated and well healed, with some dystrophic calcification at the tips of the index, middle, and ring fingers. The thumb is spared. There is no osteoporosis and there are no joint changes.
DIFFERENTIAL DIAGNOSIS Thermal injury (burns, frostbite), diabetic neuroarthropathy, leprosy, scleroderma, Lesch-Nyhan disease.
DIAGNOSIS Burns.
DISCUSSION Loss of the distal portions of multiple contiguous fingers, including distal phalanges and DIP joints, is usually from a trauma. Sparing of the thumb and normal morphology of the more proximal portions of the hand and wrist makes a systemic or vascular disease unlikely. The presence of dense bone distally would not be expected after traumatic mechanical amputation but is common following severe burns. Burns cause coagulative tissue necrosis. The depth of the injury is related to the severity and duration of the applied heat. Initially, one can see soft tissue loss and soft tissue edema. Osteoporosis and periostitis may occur in the weeks that follow. Periarticular osseous excrescences are common after extensive burns and may be seen 2 to 3 months after injury. The exact pathogenesis of these ossifications is unknown and seems not to correlate with the severity of the burn.
CASE 1.12 CLINICAL HISTORY
A 45-year-old woman with progressive gastrointestinal symptoms.

FIGURE 1.12A

FIGURE 1.12B
FINDINGS PA (A) and lateral (B) radiographs of the right hand show dense, amorphous calcium hydroxyapatite deposits in the distal portions of several digits.
DIFFERENTIAL DIAGNOSIS Scleroderma, mixed connective tissue disorder.
DIAGNOSIS Scleroderma.
DISCUSSION Scleroderma (progressive systemic sclerosis) is a multisystem fibrosing, autoimmune, connective tissue disease of variable clinical course. Characteristically, the skin becomes fibrotic, thickened, and taut. Gastrointestinal and renal involvement is prominent, but radiologic manifestations in the musculoskeletal system are present in most patients. These abnormalities are usually seen in the hands and consist of soft tissue atrophy, soft tissue calcification, resorption of the phalangeal tufts, and DIP joint erosions. Osseous destruction and bony erosions are common in the phalangeal tufts. The soft tissue atrophy results in cone-shaped fingertips. Subcutaneous calcifications are typically present in multiple digits and elsewhere in the extremities. The calcium deposits are dystrophic, and consist of calcium hydroxyapatite deposits at sites of local tissue damage. Calcification may also occur in tendons and tendon sheaths, in joint capsules, and even within the joint cavity. Synovial fibrosis without inflammation may cause flexion contractures.
CASE 1.13 CLINICAL HISTORY
A 42-year-old woman with bilateral hand pain.

FIGURE 1.13A

FIGURE 1.13B
FINDINGS (A, B) PA radiographs of both hands show that some of the metacarpals and phalanges are mildly expanded, with thin, osteopenic cortex and no clearly defined trabecular bone pattern within. The involved metacarpals are under-tubulated, resulting in a cylindrical shape. A ground-glass radiolucency can be appreciated. The distribution of abnormalities is bilateral and polyostotic, but not symmetric. Some of the bones appear normal.
DIFFERENTIAL DIAGNOSIS Fibrous dysplasia, sickle cell disease, enchondromatosis, Gaucher disease.
DIAGNOSIS Polyostotic fibrous dysplasia.
DISCUSSION The mild expansion of the long bones and thinning of the cortices suggests a space-occupying process in the marrow, but the asymmetric distribution of involvement indicates that it is a localized rather than systemic process. Fibrous dysplasia is a nonhereditary condition in which osteoblasts fail to undergo normal morphologic differentiation and maturation, resulting in lesions containing fibro-osseous tissue rather than bone. Lesions may be solitary or multiple, and one or more bones may be involved. Approximately 70% to 80% of cases are monostotic, 20% to 30% are polyostotic, and 2% to 3% are associated with endocrine dysfunction. The typical endocrine abnormality is precocious female sexual development and cutaneous pigmentation (McCune-Albright syndrome). Fibrous dysplasia weakens the structural integrity of the involved bone, predisposing it to fracture or progressive deformity. Such orthopedic complications represent the major morbidity of fibrous dysplasia. Malignant degeneration in fibrous dysplasia is extremely rare, but has been reported in the literature [27].
CASE 1.14 CLINICAL HISTORY
A 37-year-old woman who jammed her little finger.

FIGURE 1.14A

FIGURE 1.14B

FIGURE 1.14C
FINDINGS (A-C) PA, oblique, and lateral radiographs of the little finger show a mildly expansile lucent lesion occupying the proximal half of the distal phalanx but not extending to the articular surface. The expanded portion of the cortex is thinned but intact. No definite internal mineralization is seen. There is a transverse fracture through the lesion. The joint is not involved.
DIFFERENTIAL DIAGNOSIS None.
DIAGNOSIS Enchondroma, with fracture.
DISCUSSION The lesion has benign characteristics, with a well-defined sclerotic endosteal margin and an intact, although thinned and mildly expanded, cortex. The lack of cartilaginous matrix mineralization does not exclude an enchondroma.
Solitary enchondromas are benign neoplasms, located within the medullary cavity, that are composed of mature hyaline cartilage. They probably arise from cartilaginous rests displaced from the growth plate. The incidence in males and females is equal, and most patients are between 10 and 50 years of age. Typically, the lesions are asymptomatic and discovered incidentally, but many patients present with pathologic fractures. The most common locations for solitary enchondromas are the hands (about 50% of cases), the proximal and distal femur, and the proximal humerus. In the hands, the middle and distal portions of the metacarpals and the proximal portions of the phalanges are typically involved. Radiographically, these lesions are lucent from replacement of bone by nonmineralized cartilage, but the typical mineralization patterns of cartilaginous matrix may be present: dense punctate or flocculent calcifications, or ring-shaped or arc-shaped densities from enchondral ossification of lobular cartilage. Slow endosteal enlargement causes an expanded, thinned cortex, but cortical penetration is absent. Healing of pathologic fractures tends to be slow, because the thinned cortex overlying an enchondroma will not have a normal endosteal blood supply. The risk of developing chondrosarcoma in a solitary enchondroma of the hand is exceedingly low [28].
CASE 1.15 CLINICAL HISTORY
A 55-year-old man with recurrent episodes of hand pain.

FIGURE 1.15
FINDINGS PA radiograph of the left hand demonstrates multiple punched-out erosions in the carpus and index MCP region. The erosions have sclerotic margins, and an overhanging edge may be seen at the scaphoid. Bone mineralization is normal, and there are no alignment deformities. Asymmetric joint space narrowing is seen at several IP joints, at the second MCP joint, and in the carpal and radiocarpal joints.
DIFFERENTIAL DIAGNOSIS Gout, xanthomatosis, psoriasis, multicentric reticulohistiocytosis, pyrophosphate arthropathy.
DIAGNOSIS Tophaceous gout.
DISCUSSION Gout is defined by the presence of hyperuricemia (serum uric acid concentration greater than 7 mg/dL). Hyperuricemia may be idiopathic or secondary to known conditions, including excess ingestion (in protein), intrinsic overproduction, or reduced renal secretion. There is a familial incidence, but it appears to be controlled by multiple genes. Specific mutations with biochemical defects in purine metabolism leading to hyperuricemia have been found in a few cases. Gout is associated with obesity, diabetes, hyperlip-idemia, hypertension, atherosclerosis, alcohol consumption, acute illness, and pregnancy. There is a negative association with rheumatoid arthritis. The prevalence of the symptomatic forms of gout, gouty arthritis, and tophaceous gout has declined dramatically with the increased use of drugs that control hyperuricemia. Gouty arthritis is similar to other crystal-related joint diseases, whereas tophaceous gout has the radiologic appearance of a metabolic deposition disease. Tophaceous gout is the most common metabolic deposition disease. Deposits of monosodium urate crystals are called tophi, and they are generally found in the periarticular soft tissues. The development of tophi requires decades of sustained hyperuricemia and is related to the degree and duration of hyperuricemia. Control of hyperuricemia by drugs has reduced the incidence of tophi in people with gout from over 50% in the 1950s to about 3% today. Deposits near the joints and tendons cause a lumpy-bumpy appearance. These localized areas of swelling may cause the slow development of pressure erosions on adjacent bone. Such erosions will have well-defined sclerotic margins. A shell of new bone may attempt to encompass the deposit, leaving an overhanging edge. The articular spaces may be preserved until late in the disease. Tophaceous gout may occur in combination with episodes of gouty arthritis.
CASE 1.16 CLINICAL HISTORY
A 21-year-old man with hand pain after a snowboarding accident, persisting for a year.

FIGURE 1.16
FINDINGS PA radiograph of the hand shows an expansile lesion involving the distal third of the index metacarpal, extending into the epiphysis. The lesion is symmetrically expansile but appears contained by a thin expanded shell of bone. The periosteal bone at the interface between the lesion and the normal cortex has not matured, suggesting an actively enlarging process. No appreciable matrix mineralization is present.
DIFFERENTIAL DIAGNOSIS Giant cell tumor, giant cell reparative granuloma, aneurysmal bone cyst, enchondroma.
DIAGNOSIS Giant cell reparative granuloma.
DISCUSSION Giant cell reparative granuloma is a nonneo-plastic lesion of bone that is said to be a reactive process (to an unknown stimulus). It is found most commonly in the jaws and in the hands and feet; giant cell tumor of bone is distinctly unusual in these sites (fewer than 1% of the Mayo Clinic series of 671 giant cell tumors [29]). Except for location, giant cell reparative granuloma is virtually indistinguishable from giant cell tumor of bone on imaging [30], However, giant cell tumor and giant cell reparative granuloma may be distinguished from each other on histologic examination. Giant cell tumors may have a locally aggressive clinical course, whereas giant cell reparative granulomas do not.
CASE 1.17 CLINICAL HISTORY
A 70-year-old woman with rapidly progressive pain, swelling and “red bumps” in the skin of both hands.

FIGURE 1.17A
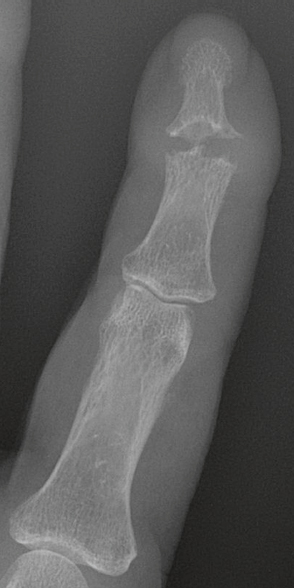
FIGURE 1.17B
FINDINGS
- PA radiograph of the hand. The soft tissues are diffusely thickened. There are erosions with overhanging edges at multiple joints, seen best at the DIP joints.
- Detail view of the index finger.
DIFFERENTIAL DIAGNOSIS Multicentric reticulohistiocytosis, erosive osteoarthritis, gout, psoriasis.
DIAGNOSIS Multicentric reticulohistiocytosis.
DISCUSSION Metabolic deposition diseases involving the joints, in which the body accumulates a substance it cannot excrete or metabolize, are relatively uncommon. If focal, mass-like deposits are located in the musculoskeletal system, the result is a clinically indolent disease with randomly distributed, slowly enlarging, space-occupying deposits. Chronic erosions with overhanging edges are a classic feature of metabolic deposition disease. In this case, the diffuse soft tissue thickening and the absence of a lumpy-bumpy morphology mitigate against tophaceous gout, the only common form of metabolic deposition disease involving the bones and joints. In the rare condition of multicentric reticulohistiocytosis, lipid-containing macrophages are deposited randomly in the soft tissues around joints and tendons. Skin nodules are common. As with gout and other metabolic deposition diseases, normal bone density and normal joint spaces are associated with intraosseous and juxta-articular accumulations. Bone erosions with sclerotic margins and overhanging edges are typical, but sometimes a destructive, erosive arthritis ensues [31]. The origin of the abnormal lipid is unknown. Multicentric reticulohistiocytosis may be associated with the development of malignancies and has been described as a paraneoplastic syndrome [32].
CASE 1.18 CLINICAL HISTORY
A 43-year-old woman with difficulty using her hands.

FIGURE 1.18
FINDINGS PA radiograph of the left hand shows severe subluxations at the MCP joints, with marked ulnar deviation of the fingers. The carpometacarpal joint of the thumb is dislocated, with proximal retraction of the first metacarpal. The entire carpus is translocated toward the ulna. Boutonniere deformities involve the index and middle fingers, and flexion deformities involve the little finger. Erosions of bone are absent, and there are no hypertrophic changes of bone. Bone density is nearly normal, although perhaps slightly osteopenic.
DIFFERENTIAL DIAGNOSIS Systemic lupus erythematosus (SLE), scleroderma, spondyloarthropathy, rheumatoid arthritis.
DIAGNOSIS Systemic lupus erythematosus.
DISCUSSION SLE is a chronic systemic disease whose pathogenesis is related to immune complex deposition. It is more common in women by an 8:1 ratio, and there is a component of genetic susceptibility. The fluorescent antinuclear antibody test is virtually always positive at the onset of clinical disease. Manifestations in the musculoskeletal system are common, and may antedate other systemic manifestations by months or years. Nonerosive symmetric polyarthritis with a distribution similar to that of rheumatoid arthritis is present in 75% to 90% of patients with SLE. The early findings on radiographs are fusiform soft tissue swelling and juxta-articular osteoporosis, but there should be no joint space narrowing or erosions. A deforming nonerosive arthropathy is also common in patients with SLE. The hands are typically involved at the MCP and IP joints. Thumb, wrist, and foot involvement is more common than shoulder and knee involvement. Ten percent of patients may develop atlantoaxial subluxation. These deformities are initially reducible, and radiographs may appear normal. Fixed deformities and secondary degenerative changes may develop with time. Osteonecrosis may involve the femoral head, femoral condyle, humeral head, and other sites, and it commonly has a symmetric distribution. Myositis, tendon weakening and spontaneous rupture, and soft tissue calcification are other musculoskeletal manifestations.
CASE 1.19 CLINICAL HISTORY
A 45-year-old woman with pain and stiffness in both hands.

FIGURE 1.19
FINDINGS PA radiographs of both hands show mild ulnar subluxation of the second and third MCP joints on the right, and the second MCP joint on the left. Marginal erosions involving the metacarpal heads are present at these sites. Secondary degenerative changes are present at the left second MCP joint. The other joints appear relatively spared. Bone mineralization appears normal.
DIFFERENTIAL DIAGNOSIS Rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, osteoarthritis.
DIAGNOSIS Rheumatoid arthritis.
DISCUSSION The distribution of disease is that of rheumatoid arthritis in the MCP joints. The marginal erosions are characteristic, and the alignment deformities are suggestive. Although the radiographic manifestations of rheumatoid arthritis are often bilateral and symmetric, bilateral and asymmetric findings may be present early in the course, and progression may be modified by treatment.
Secondary degenerative changes, such as subchondral sclerosis, may occur if the inflammatory process remits for several years. Both rheumatoid arthritis and primary osteoarthritis are common conditions; patients with both diseases may have confusing radiographic findings. In this case, the distribution of disease is not that of osteoarthritis. The common late radiologic findings of rheumatoid arthritis include chronic generalized osteoporosis, progression of marginal erosions to severe erosions involving subchondral bone, synovial cyst formation, subluxations and abnormalities of alignment, and secondary osteoarthritis. Compressive erosions and remodeling of bone may result from the collapse of osteoporotic bone by muscle tension; this is particularly common at the MCP joints. Malalignment in advanced disease results from the loss of balanced muscular tension and ligamentous involvement by the inflammatory process.
CASE 1.20 CLINICAL HISTORY
A 35-year-old woman with morning stiffness of her hands.

FIGURE 1.20
FINDINGS PA radiographs of both hands show juxta-articular osteopenia. The cartilage spaces of the carpal, MCP, and PIP joints are diffusely narrowed, and erosions are present, particularly at the MCP joints. There are no hypertrophic bony changes such as osteophytes or subchondral sclerosis.
DIFFERENTIAL DIAGNOSIS Rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, osteoarthritis.
DIAGNOSIS Rheumatoid arthritis.
DISCUSSION The underlying pathologic change in rheumatoid arthritis is chronic synovial inflammation with hyperemia, edema, and effusion. Although symmetric clinical involvement is the rule, the clinical involvement may not correlate with the sites of radiologic involvement. The earliest radiographic changes are demonstrated in this case. The earliest sites of erosions are typically at the MCP joints and are seen best on the supinated oblique “ball catcher’s” views. As the condition progresses, the radiographic features tend to become much more pronounced and differentiated from other forms of polyarticular arthritis. Rheumatoid arthritis has a prevalence of 1% in the general population; women are affected more than men by a 3:1 ratio. The clinical course is progressive in 70% of cases, with rapid or slow clinical deterioration. In 20% of cases, the disease is intermittent, with remissions and exacerbations. In 10% of cases, the remissions may last for several years.
CASE 1.21 CLINICAL HISTORY
A 63-year-old woman with polyarthritis.
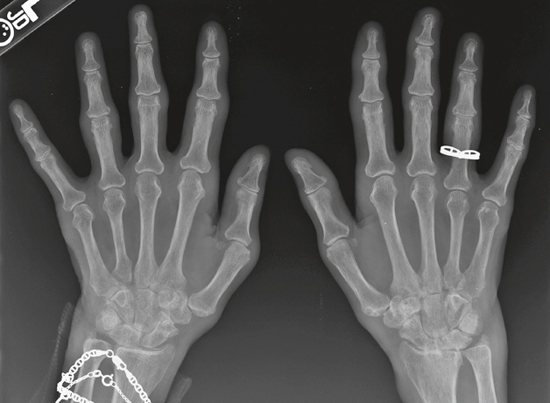
FIGURE 1.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree