Chapter Outline
Temporal Bone, 457
General, 457
Trauma, 460
Inflammation, 460
Tumors, 463
Otodystrophies and Dysplasias, 463
Congenital Anomalies, 464
Skull Base, Foramina, and Cranial Nerves, 465
General, 465
Anterior Skull Base Lesions, 467
Central Skull Base Lesions, 467
Perineural Tumor Spread, 468
Orbit, 469
General, 469
Globe, 469
Optic Nerve, 472
Extraocular Tumors and Vascular Lesions, 472
Infectious, Inflammatory, and Infiltrative Lesions, 473
Trauma, 474
Other, 475
Lymph Nodes, 475
Oral Cavity, Suprahyoid and Infrahyoid Neck, and Larynx, 476
Sinuses, Nasal Cavity, 489
Glands and Periglandular Region, 496
Mandible and Maxilla, 503
Differential Diagnosis, 506
Temporal Bone
General
The temporal bone is divided into five portions:
- •
Mastoid (posterolateral part that includes the mastoid process: attachment for sternocleidomastoid and other muscles)
- •
Petrous portion (pyramidal-shaped medial part; inner ear structures, internal auditory canal [IAC], petrous apex)
- •
Squamous portion (anterolateral part; forms lateral wall of middle cranial fossa)
- •
Tympanic portion (forms bulk of external auditory canal [EAC] and middle ear space)
- •
Styloid portion
- •
External Auditory Canal (EAC)
- •
Cartilaginous portion
- •
Bony portion
- •
Middle Ear ( Figs. 7.1 – 7.2 )
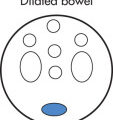
Composed of air-filled spaces that contain the ossicles and are divided into:
- •
Epitympanum (attic; above imaginary line between scutum tip and tympanic facial nerve)
- •
Mesotympanum (middle ear proper between epitympanum and hypotympanum)
- •
Hypotympanum (shallow space below imaginary line between tympanic annulus and cochlear promontory)
- •


Boundaries of the middle ear are tympanic membrane (TM) laterally, the tegmen superiorly, and the inner ear medially. Posteriorly, there are three important structures (facial nerve recess, pyramidal eminence, and sinus tympani). The eustachian tube (pressure equalization) connects the middle ear with the nasopharynx. The lateral epitympanic recess (Prussak space) is a common location for retraction pockets and cholesteatoma. Three ossicles transmit sound waves from the TM to the oval window in the vestibule:
- •
Malleus
- •
Incus
- •
Stapes (two crura, one footplate)
- •
Inner Ear ( Fig. 7.3 )
The inner ear (labyrinth) consists of:
- •
Three semicircular canals, which connect to vestibule
- •
Vestibule (utricle and saccule) between semicircular canals and cochlea
- •
Cochlea (sensorineural hearing), which connects to:
Stapes → oval window
Round window (allows for counterpulsation of fluid)
- •

Internal Auditory Canal (IAC) ( Fig. 7.4 )
Left and right IAC should not differ >2 mm in diameter. Contents of IAC are divided by the falciform crest and Bill bar:
- •
Facial nerve (anterior superior): cranial nerve (CN) VII (“7 up”)
- •
Cochlear part (anterior inferior): CN VIII (“Coke down”)
- •
Superior vestibular nerve (posterior): CN VIII
- •
Inferior vestibular nerve (posterior): CN VIII
- •

Facial Nerve ( Figs. 7.5 – 7.6 )
Four main parts of the facial nerve:
- •
Intraaxial segment
- •
Cisternal segment
- •
Intratemporal segment:
Meatal (IAC) segment
Labyrinthine segment
Tympanic (horizontal) segment
Mastoid (vertical) segment
- •
Extracranial segment:
Exits the skull through the stylomastoid foramen
Immediately gives off the posterior auricular branch/nerve
- •


Main trunk courses through the parotid gland and gives rise to five terminal branches. The intratemporal segment of the facial nerve gives rise to three branches (see Fig. 7.6 ):
- •
Greater superficial petrosal nerve
- •
Stapedius nerve
- •
Chorda tympani nerve
- •
Hearing Loss
Types
Conductive
- •
Disruption of sound conduction that may be secondary to abnormalities in the EAC, TM, ossicles, or oval window
- •
Common underlying causes: otitis, cholesteatoma, otosclerosis, trauma
- •
Sensorineural
- •
Evaluate inner ear, IAC
- •
Common underlying causes: idiopathic, hereditary, vestibular Schwannoma, enlargement of vestibular aqueduct, labyrinthitis ossificans, otosclerosis (cochlear otosclerosis), trauma
- •
Pulsatile Tinnitus
Causes
Normal vascular variants
- •
Aberrant ICA
- •
Jugular bulb anomalies (high or dehiscent jugular bulb, diverticulum)
- •
Persistent stapedial artery
- •
Vascular tumors
- •
Glomus jugulare paraganglioma
- •
Glomus tympanicum
- •
Vascular abnormalities
- •
Skull base dural arteriovenous fistula/arteriovenous malformation (AVM)
- •
Atherosclerotic carotid artery stenosis
- •
Carotid-cavernous fistula (CCF)
- •
ICA dissection or aneurysm at the petrous apex
- •
Fibromuscular dysplasia
- •
Dural sinus stenosis
- •
Transverse-sigmoid sinus diverticulum
- •
Other causes of tinnitus
- •
Idiopathic intracranial hypertension
- •
Paget disease
- •
Otosclerosis
- •
Ménière disease
- •
Trauma
Temporal Bone Fractures
Clinical Findings
- •
Periauricular swelling and ecchymosis (Battle sign)
- •
Bleeding into EAC or hemotympanum
- •
Hearing loss
- •
Tinnitus
- •
Vertigo
- •
Cerebrospinal fluid (CSF) leak
- •
Facial paresis
- •
Radiographic Features
| Parameter | Longitudinal Fractures | Transverse Fractures |
|---|---|---|
| Frequency | 80% | 20% |
| Fracture line | Parallel to long axis | Perpendicular to long axis |
| Typically involves | Middle ear | Inner ear |
| Labyrinth | Typically spared | Commonly involved |
| Ossicles | Involved: conductive hearing loss | Commonly spared |
| Tympanic membrane | Involved | Frequently spared |
| Facial paralysis | Approx. 20% | Approx. 50% |
a Fractures may also be characterized as oblique: mixed features of longitudinal and transverse fractures, cross the petrotympanic fissure.

Fracture Complications
- •
Ossicular fractures or dislocations
- •
TM perforation
- •
Hemotympanum
- •
CN VII paralysis
- •
CSF otorrhea
- •
Meningitis, abscess
- •
Sinus thrombosis, rare
- •
Labyrinthitis ossificans (late)
- •
Also assess for associated cervical spine fracture or fracture extension to carotid canal.
- •
Indications for Surgery in Temporal Bone Fractures
- •
Ossicular fracture or dislocation: varied, conservative or surgery
- •
Facial nerve injury: frequently conservative, but occasionally requires surgical decompression
- •
Labyrinthine fistulae: surgery if persistent
- •
CSF leaks: surgery if persistent
- •
Inflammation
Acute Inflammation
- •
Otitis media (fluid in the middle ear cavity): acute, subacute, chronic forms
- •
Children: common
- •
Adults: less common; exclude nasopharyngeal carcinoma (NPC), which can cause eustachian tube obstruction and serous otitis media.
- •
Mastoiditis: fluid-filled mastoid cells are also often present but not specific for infection.
- •
Coalescent mastoiditis: occurs if medical treatment of acute otomastoiditis fails. Enzymatic resorption of mastoid septa and development of an intramastoid empyema seen as erosive changes on computed tomography (CT); comparison with the opposite side can be helpful in subtle cases.
- •
Labyrinthitis
- •
Potential Complications
- •
Meningitis
- •
Subdural empyema or epidural abscess
- •
Dural venous sinus thrombosis
- •
Petrositis (infection of petrous air cells)
- •
Gradenigo syndrome (rare complication of petrositis: triad of otomastoiditis, sixth nerve palsy, and pain in the distribution of the fifth nerve)
- •
Subperiosteal or Bezold (via defect at the mastoid tip) abscess
- •
Focal encephalitis, brain abscess, otitic hydrocephalus
- •
Bell Palsy
Acute onset peripheral facial nerve palsy secondary to herpes simplex virus (HSV) that the majority of time resolves within 2 to 3 months. Imaging typically performed for atypical or persistent palsy. By magnetic resonance imaging (MRI), there is enhancement along the facial nerve involving intracanalicular (“fundal tuft”) and labyrinthine segments that normally do not enhance. Note that mild enhancement of the tympanic and mastoid segments of the facial nerve can be seen as a normal finding due to vascular supply. Facial nerve enhancement is nonspecific and can occur in other inflammatory and neoplastic conditions (especially if the nerve is enlarged, consider secondary to perineural spread of a tumor).
Acquired Cholesteatoma ( Fig. 7.8 )
Mass of stratified squamous epithelium and keratin debris. Cause: epithelial cells accumulate in the middle ear via a perforation of the TM. The most accepted theory is that they arise from TM retraction pockets resulting from decreased intratympanic pressure. Types:
- •
Acquired (98%): chronic middle ear infection (common). Arise in attic (Prussak space; pars flaccida cholesteatoma), or from pars tensa (sinus tympani).
- •
Congenital (epidermoid; 2%): cholesteatoma arises from epithelial nests in middle ear, mastoid, or petrous bone, including the labyrinth (uncommon).
- •

Radiographic Features
- •
High resolution temporal bone CT first line, excellent for detailed bone evaluation; MRI can be helpful for complex cases and cholesteatoma distinction.
- •
Soft tissue mass in middle ear
- •
Borders may be well- or ill-defined.
- •
Erosion of incus and otic spur (scutum) common
- •
Bone resorption (collagenase) is typical and occurs most commonly in:
Ossicles
Lateral semicircular canal (fistula)
Tegmen tympani
Facial canal
- •
Mastoid air cells may be underpneumatized and sclerotic secondary to chronic infection.
- •
Labyrinthine fistula formation in lateral semicircular canal is less common.
- •
It is often impossible to distinguish chronic middle ear infection from cholesteatoma in cases with little bone destruction on CT. However, MRI can be useful for distinction of cholesteatoma (restricted diffusion, no enhancement) from inflammatory changes or granulation tissue (enhances).
- •
| Parameter | Attic Cholesteatoma | Sinus Cholesteatoma |
|---|---|---|
| TM perforation | Pars flaccida | Pars tensa |
| Location | Prussak’s space | Sinus tympani |
| Ossicles displaced | Medially | Laterally |
| Bone erosion | Lateral tympanic wall (erosion of scutum is an early finding) | Initially subtle |
| Ossicle erosion | Head of malleus and long process of incus | Short process of incus and stapes |
Complications of Acquired Cholesteatoma
- •
Labyrinthine fistula (dehiscence of semicircular canals—most frequently lateral canal)
- •
Facial nerve paralysis (involvement of facial nerve canal)
- •
Invasion of tegmen tympani, petrous apex, or sigmoid plate
- •
Automastoidectomy
- •
Congenital Cholesteatoma (Epidermoid)
Constitute approximately 2% of temporal bone cholesteatomas and may affect middle ear, EAC, mastoid, or petrous bone, including the labyrinth (uncommon). The most common location is the anterosuperior portion of the middle ear near the eustachian tube or stapes. The typical presentation is in a young patient with otherwise normal mastoid pneumatization and without history of chronic ear infections. Histologically, the cholesteatoma is made up of squamous cell lining, keratin debris, and cholesterol.
Cholesterol Granuloma (Cholesterol Cysts)
Mix of hemorrhage, cholesterol crystals, and granulation tissue that may be present in temporal bone, including the petrous apex or rarely the middle ear. Depending on the location of the expansile erosive lesion and involvement of critical structures, they can be associated with hearing loss, tinnitus, and CN palsies.
Radiographic Features
- •
Expansile erosive osseous lesion of the petrous apex
- •
Smooth margins
- •
CT: isodense relative to brain, no enhancement, no calcification
- •
MRI: hyperintense relative to brain on T1-weighted (T1W) images because of methemoglobin and cholesterol crystals
- •
Cholesterol granulomas retain their high signal on fat suppressed T1W images, distinguishing them from fatty lesions.
- •
| Epidermoid (Congenital Cholesteatoma) | Cholesterol Granuloma (Cholesterol Cyst) | Mucocele a | |
|---|---|---|---|
| CT | ≤ | Isodense, no calcium, no enhancement | < or occasionally > |
| T1W | ≤ (lamination) | > (cholesterol) | ≤ or occasionally > |
| T2W | > | > (with peripheral low signal hemosiderin ring) | > or occasionally < |
a Density and MRI signal characteristics of mucoceles can vary depending on protein content.
Malignant or Necrotizing External Otitis
Severe, life-threatening Pseudomonas aeruginosa infection in older adults with diabetes. Aggressive infection of EAC, adjacent soft tissues, and skull base that spreads via cartilaginous fissures of Santorini and can extend into:
- •
Middle ear and mastoid air cells
- •
Variable involvement of skull base, including osteomyelitis
- •
Phlegmon and abscesses may spread in any direction:
Parapharyngeal, parotid, or masticator space
Intracranially
Anteriorly to temporomandibular joint (TMJ)
- •
Radiographic Features
- •
Early findings may manifest as thickened mucosa of EAC and soft tissue swelling; more advanced disease can have bone erosion associated with the opacification.
- •
Mastoiditis
- •
Skull base osteomyelitis
- •
Sinus phlebitis and thrombosis
- •
Phlegmon or abscess in nearby soft tissues and spaces
- •
Labyrinthitis Ossificans
Ossification of the membranous labyrinth as a sequela of previous infectious, inflammatory, traumatic, or surgical injury to the inner ear. Seen as ossification within the membranous labyrinth on high resolution computed tomography (HRCT) and foci of low signal on T2-weighted (T2W) MRI within the otherwise high signal fluid of the membranous labyrinth.
Tumors
Glomus Tumors
Glomus tumors (chemodectomas) arise from chemoreceptor cells in multiple sites in the head and neck. The majority are benign and approximately 10% are multiple; thus it is important to check other common locations in the head and neck during imaging (glomus jugulare, vagale, and carotid body tumor). Glomus tympanicum represents the most common middle ear tumor.
Types
- •
Glomus jugulare: origin at jugular bulb; more common
- •
Glomus tympanicum: arises from paraganglia along inferior tympanic nerve (Jacobson nerve), frequently on the cochlear promontory
- •
Glomus vagale
- •
Carotid body tumor
- •
Clinical Findings
- •
Pulsatile tinnitus (most common)
- •
Conductive hearing loss
- •
Rarely, facial nerve paralysis
- •
Other focal neurologic symptoms depending on location as well as systemic symptoms such as sudden blood pressure (BP) fluctuations if the tumor secretes catecholamines
- •
Radiographic Features
- •
Glomus tympanicum typically presents as a small enhancing soft tissue mass centered over the cochlear promontory. Enhancement distinguishes tumors from obstructive secretions.
- •
Glomus jugulare (glomus jugulotympanicum) is centered in the region of the jugular foramen. Most common path of spread is to the middle ear. It is accompanied by permeative bone changes in the jugular foramen. Characteristic findings by MRI are multiple low signal intensity areas that represent flow voids in the tumor. This has a salt-and-pepper appearance.
- •
Glomus vagale paraganglioma: arises from paraganglia in the nodose ganglion of the vagus nerve in the nasopharyngeal carotid (or poststyloid parapharyngeal) space; displaces carotid anteromedially, jugular vein posterolaterally, and does not splay the carotid bifurcation.
- •
Carotid body paraganglioma: arises from carotid glomus bodies (paraganglia); splays the external carotid artery (ECA) and internal carotid artery (ICA).
- •
Intense contrast enhancement by CT, MRI, angiography
- •
Large tumors erode bone.
- •
Other Benign Temporal Bone Tumors
- •
Meningioma
- •
Facial schwannoma may arise anywhere along the course of CN VII. In the IAC, the tumor may be indistinguishable from a vestibular schwannoma unless it can be seen to arise from the facial nerve.
- •
Osteoma
- •
Adenoma (ceruminoma), benign but locally aggressive, rare
- •
Endolymphatic sac tumor, benign but locally aggressive; permeative destructive lesion with spiculated calcified tumor matrix
- •
Epidermoid (primary cholesteatoma): not a true neoplasm
- •
Malignant Temporal Bone Tumors
- •
Carcinoma (CA) (most common malignant tumors)
Squamous cell carcinoma (SCC) arising from the EAC
Adenocarcinoma
- •
Lymphoma
- •
Metastases: breast, lung, renal, prostate; neuroblastoma and leukemia in children
- •
Chondrosarcoma, other primary bone tumors
- •
Rhabdomyosarcoma in children and late teens
- •
Otodystrophies and Dysplasias
Otosclerosis (Otospongiosis)
The osseous labyrinth (otic capsule) is the normal dense bone of the inner ear surrounding the cochlea, vestibule, and semicircular canals. In otosclerosis, the capsule is replaced by vascular, irregular bony trabeculae (lucent on CT) and later by new bone within the lucent areas in the late, chronic healing phase. Unknown cause, sporadic or autosomal dominant (AD) gene transmission, frequently bilateral. Patients (female > male) present with progressive conductive or mixed hearing loss.
Types
- •
Fenestral: sclerosis or spongiosis around oval window, including fixation of stapes. Diagnosis is usually made from clinical and audiometric findings (conductive hearing loss). Begins as radiolucent focus at the anterior margin of the oval window. Early disease may not be seen on imaging or may be very subtle.
- •
Cochlear (retrofenestral) otosclerosis: involves pericochlear bony labyrinth. CT findings:
Deossification around cochlea (lucent halo)
Sclerosis occurs later in disease (mixed lucencies and densities)
- •
Disease begins at fissula ante fenestram (fenestral); fenestral alone most common (85%, conductive hearing loss); approximately 15% progress to cochlear (mixed hearing loss).
- •
Semicircular Canal Dehiscence Syndrome
CT shows a small defect or dehiscence in the bony wall of the superior or less commonly posterior semicircular canal. Seen as ≥2 mm dehiscence of roof of superior semicircular canal on coronal or ideally transverse oblique (Poschl) CT reformats for superior semicircular canal dehiscence. Clinically presents with dizziness and vertigo +/– nystagmus with loud sound or pressure (Tullio phenomenon). Clinical syndrome + positive CT = semicircular canal dehiscence syndrome. Can also be associated with inner ear conductive hearing loss. The cause is unknown, likely developmental, possibly also secondary to trauma.
Other Otodystrophies and Dysplasias
- •
Paget disease
- •
Fibrous dysplasia
- •
Osteogenesis imperfecta
- •
Skull base osteopetrosis
- •
Craniometaphyseal dysplasia (Pyle disease)
- •
Craniodiaphyseal dysplasia and Camurati-Engelmann disease (progressive diaphyseal dysplasia)
- •
Cleidocranial dysostosis
- •
Congenital Anomalies
Congenital Abnormalities of the Inner Ear
- •
Cochlear incomplete partition type I: spectrum of abnormalities ranging from lack of internal structure of the cochlea to severe cystic cochleovestibular malformation
- •
Cochlear incomplete partition type II: incomplete partition with deficient interscalar septum between middle and apical turns (Mondini anomaly: historic terminology – incomplete partition type II + large vestibular aqueduct)
- •
Cochlear hypoplasia: small, underdeveloped cochlea, typically <2 turns
- •
Cochlear aplasia: absent cochlea with variable anomalies of other inner ear structures
- •
Labyrinthine aplasia: aplasia or hypoplasia of otic capsule, petrous apex hypoplasia, and other associated temporal bone abnormalities (Michel aplasia: historic terminology for complete labyrinthine aplasia)
- •
Common cavity malformation: undifferentiated cochlea and vestibule represented by a common cavity of variable size.
- •
Large vestibular aqueduct: ≥1 mm diameter at midpoint and/or ≥2 mm at operculum perpendicular to long axis of vestibular aqueduct; rule of thumb—abnormal if larger than the posterior semicircular canal. High incidence of associated cochlear abnormalities (also see incomplete partition II above).
- •
Small IAC
- •
Petrous Malformations Associated With Recurrent Meningitis
- •
The presence of a fistula in the petrous portion of the temporal bone may lead to otorrhea, pneumocephalus, meningitis, or abscess; rare.
- •
Acquired lesion of the petrous apex can potentially have similar complications depending on extent and violation of adjacent structures.
- •
Overview of Syndromes
| Syndrome/Disease | Inner Ear | Middle Ear | Outer Ear | Other Abnormalities |
|---|---|---|---|---|
| Otocraniofacial | ||||
| Treacher-Collins syndrome | ++ | ++ | ++ | Coloboma, mandibular hypoplasia (micrognathia), microtia |
| Otocervical | ||||
| Klippel-Feil syndrome | ++ | ++ | ++ | Cervical fusion, short neck, low posterior hairline, limited cervical motion |
| Cleidocranial dysplasia (dysostosis) | + | + | ++ | Hypoplastic, malformed, or absent clavicles; large head, underdeveloped facial bones |
| Otoskeletal | ||||
| Osteogenesis imperfecta | ++ | + | − | Fractures, blue sclera in some subtypes |
| Osteopetrosis | + | ++ | ++ | Autosomal recessive: macrocephaly, deafness and blindness; autosomal dominant much less severe, may even be asymptomatic |
| Other | ||||
| Hemifacial macrosomia (Goldenhar syndrome, oculoauriculovertebral spectrum) | + | ++ | ++ | Facial asymmetry, microtia, variable ocular abnormalities, cervical spine deformity |
| CHARGE | ++ | ++ | ++ | Coloboma, heart anomaly, choanal atresia, mental retardation, genital hypoplasia |
| Pendred syndrome | ++ | − | − | Thyroid organification defect with goiter |
| Branchio-oto-renal syndrome | ++ | ++ | ++ | Branchial and renal anomalies |
| Thalidomide | ++ | ++ | ++ | Short limbs, cardiac and GI abnormalities |
a There can be variations in the type and extent of otologic abnormalities associated with each syndrome.
Skull Base, Foramina, and Cranial Nerves
General
Anterior and Central Skull Base Anatomy
- •
Anterior skull base: broadly consists of floor of anterior cranial fossa and the roof of the nose, ethmoid air cells, and orbits.
- •
Central skull base: broadly consists of floor of middle cranial fossa, roof of sphenoid sinus, and greater wing of sphenoid.
- •
Anterior and central skull base boundary:
Medially: posterior margin of planum sphenoidale (tuberculum sellae)
Laterally: lesser wing of sphenoid/sphenoid
- •
Central Nervous System (CNS), Foramina, and Cavernous Sinus ( Figs. 7.9 – 7.10 )
- •

FIG. 7.9

FIG. 7.10
- •
CN II: optic nerve
- •
CN III: oculomotor nerve
- •
CN IV: trochlear nerve
- •
CN V: trigeminal nerve
- •
CN VI: abducens nerve
- •
CN VII: facial nerve
- •
CN VIII: auditory nerve
- •
CN IX: glossopharyngeal nerve
- •
CN X: vagus nerve
- •
CN XI: spinal accessory nerve
- •
CN XII: hypoglossal nerve
- •
| Opening | Cranial Nerve | Artery | Vein |
|---|---|---|---|
| Optic canal | II | Ophthalmic artery | |
| Superior orbital fissure | III, IV, V1, VI | Orbital branches of middle meningeal artery (occasionally), recurrent meningeal branches of lacrimal artery | Ophthalmic veins |
| Inferior orbital fissure | Infraorbital nerve (V2) | Infraorbital artery | Ophthalmic vein (inferior division) |
| Carotid canal | Sympathetic plexus | ICA | |
| Foramen rotundum | V2 | Artery of foramen rotundum | Emissary veins |
| Foramen ovale | V3 | Accessory meningeal artery | Emissary veins |
| Foramen spinosum | Meningeal (recurrent) branch of mandibular nerve, lesser petrosal nerve (occasionally) | Middle meningeal artery | Middle meningeal vein |
| Foramen lacerum (not a true foramen) | Nerve of the pterygoid canal (formed by greater petrosal and deep petrosal nerves) | Terminal (meningeal) branches of ascending pharyngeal artery | Emissary veins |
| Vidian (pterygoid) canal | Vidian nerve | Vidian artery | Vidian vein |
| Stylomastoid foramen | VII | Stylomastoid artery | |
| Jugular foramen pars nervosa | IX, Jacobson nerve | Inferior petrosal sinus | |
| Jugular foramen pars vascularis | X, XI, Arnold nerve | Posterior meningeal artery | Jugular bulb |
| Hypoglossal canal | XII |
Pterygopalatine Fossa (PPF) (see Fig. 7.10 )
- •
Important space and potential route of spread of disease in the deep face
- •
Contents:
Pterygopalatine ganglion
Maxillary nerve (V2) via foramen rotundum
Distal internal maxillary artery via pterygomaxillary fissure
- •
Relations and boundaries:
Anterior: posterior maxillary sinus wall
Posterior: pterygoid plates and inferior part of lesser wing of sphenoid
Superior: inferior orbital fissure
Inferior: tapers into the greater palatine canal
Medial wall: perpendicular plate of palatine bone, sphenopalatine foramen superiorly
Lateral wall: pterygomaxillary fissure (vertical communication with infratemporal fossa)
- •
Anterior Skull Base Lesions
Lesion affecting the anterior skull base can be centered in the bone, arise in the anterior cranial fossa above, or arise from sinonasal cavities below; localization of lesion center can help with the differential.
Neoplasms: Benign and Malignant
- •
Meningioma: classic locations olfactory groove and planum sphenoidale
- •
Olfactory neuroblastoma (esthesioneuroblastoma): malignant tumor arising from olfactory mucosa in superior nasal cavity
Heterogeneously enhancing mass in upper nasal cavity
Larger tumors extend to the floor of anterior cranial fossa with erosive bone changes.
May have “waist” at level of cribriform plate
Peripheral tumor cysts at intracranial tumor-brain margin are highly suggestive of diagnosis.
- •
Osteoma (sinonasal): well-defined nonaggressive bony mass, most common in frontal and ethmoid sinuses.
- •
Metastasis: bone destruction, may involve dura or brain parenchyma
- •
Sinonasal SCC: most common primary sinonasal malignancy, ethmoid sinus and nasal cavity primaries may extend to the anterior skull base.
Aggressive lesion with bone destruction
- •
Sinonasal undifferentiated CA: rare, highly aggressive sinonasal malignancy
- •
Sinonasal lymphoma: cephalad extension from nasal cavity through skull base
Typically, homogeneous lesions with relatively high density on unenhanced CT
Septal destruction, occasional bone remodeling
On MRI, relatively low signal on T2W images, homogeneously enhancing
- •
Sinonasal melanoma: highly malignant, nasal cavity often site of origin
Bone destruction more frequent than remodeling
On MRI lesions may have intrinsically high signal on T1W and low signal on T2W images (paramagnetic properties of melanin)
Avid enhancement
- •
Hemangiopericytoma: hypervascular lesion with aggressive growth pattern
Dural-based mass that may have internal flow voids
Intensely enhancing
- •
Sinonasal nerve sheath tumor: benign neoplasm arising from peripheral nerve Schwann cells
Well-defined lesion with smooth remodeling
Enhancing sharply marginated mass, may have internal cystic changes
- •
Nonneoplastic Lesions
- •
Fibrous dysplasia: expansile developmental bone lesion
Classically ground-glass matrix (varies depending on amount of fibrous and ossified components)
Enhancing lesion, can be deceptively aggressive on MRI (suspect if very low signal on T1 and T2)
Obtain CT to demonstrate typical characteristics
- •
Mucocele: expanded sinus from chronic obstruction
Variable signal depending on protein content of secretions
No solid enhancement (can see mucosal enhancement around the margins)
Nonaggressive with bone remodeling, MRI highly accurate for distinguishing higher density/proteinaceous secretions that are equivocal on CT from solid masses.
- •
Meningocele and encephalocele: extension of meninges ± brain parenchyma through skull base defect into nasal cavity or ethmoidal labyrinth
CT frequently shows bone defect.
High resolution MRI for confirmation
Heavily T2W high resolution sequences can be helpful for clear demonstration of extension of meninges and/or brain through defect.
- •
Nasal dermal sinus: midline developmental lesion anywhere from nasal tip to anterior skull base at foramen cecum, may be associated with nasal pit or repetitive bouts of meningitis clinically.
Look for tract from nasal lesion to anterior cranial fossa.
May see widened foramen cecum ± bifid crista galli
May have associated dermoid/epidermoid along tract
- •
Central Skull Base Lesions
Lesions may arise from central skull base components, represent inferior extension from above or superior extension from below. Characterization of calcified matrix can help in the diagnosis of cartilaginous lesions and is best seen on CT.
Neoplasms: Benign and Malignant
- •
Metastasis: suspect in patient with known malignant neoplasm with new craniofacial pain or cranial neuropathy
Lytic destructive lesion
May have associated soft tissue mass
Look for multiple lesions
- •
Meningioma: in addition to those with a classic appearance, occasionally lesions can be infiltrative, extend to extracranial spaces such as pterygopalatine and infratemporal fossa, or have intraosseous component.
- •
Multiple myeloma: commonly lytic, multiple, may be indistinguishable from extensive metastatic disease with lytic pattern.
- •
Lymphoma: may originate in bone or from dura, wide range of appearances.
Typically enhance uniformly
Can be dural-based
Can involve bone with lytic changes
Extensive soft tissue mass
Relatively restricted diffusion with low apparent diffusion coefficient (ADC) values
- •
Pituitary macroadenoma: may occasionally extend inferiorly into clivus or sphenoid sinus.
- •
Chordoma (clivus): rare, locally aggressive tumor arising from primitive notochord remnants
May present with headaches and diplopia secondary to CN VI involvement in Dorello canal, other nerves can be involved depending on extent.
Expansile destructive midline clival mass, may be near sphenooccipital synchondrosis
Classically high signal on T2W images secondary to high water content
Can also have mix of calcification, hemorrhage, and mucoid material with increased T1 and decreased T2 signal
Enhancing lesion, sometimes in a “honeycomb” pattern
- •
Chondrosarcoma: arises in skull base fissures and synchondroses, most commonly petrooccipital fissure.
Typically eccentric (in contradistinction to chordoma)
Chondroid ring and arc-like calcifications on CT
Heterogeneously enhancing with high T2 signal with scattered hypointense foci (calcifications) on MRI
- •
Langerhans cell histiocytosis: lytic enhancing lesion typically presenting in the first decade of life
- •
Nonneoplastic Lesions
- •
Fibrous dysplasia: relatively common expansile bone lesion
Classically ground-glass matrix (varies depending on amount of fibrous and ossified components)
Enhancing lesion, can be deceptively aggressive on MRI (suspect if very low signal on T1 and T2)
Obtain CT to demonstrate typical characteristics
- •
Paget disease: primary metabolic bony disease, often asymptomatic, typically seen in older adults, more common in males
May be multifocal disease, with mixed lytic-sclerotic pattern
Well-defined lytic regions with bone expansion in early phase
“Cotton wool” appearance later in lytic-sclerotic phase
On MRI, hypointense on T1 and heterogeneous enhancement
- •
Aneurysm: cavernous or other ICA segments
Rounded “mass,” low signal/flow void on MRI: must recognize!
Pulsation artifact in phase encoding direction
CT or magnetic resonance (MR) angiography to confirm
- •
Arachnoid granulation: lesions found along dural sinuses and dural surface, typically incidental but in patients with CSF leaks may represent the site of osteodural defect.
- •
Basal cephalocele: uncommon, usually congenital
- •
Persistent craniopharyngeal canal: developmental anomaly resulting in a persistent tract from nasopharynx to pituitary fossa.
Smoothly marginated midline canal between presphenoid and basisphenoid.
Typically incidental finding but may be associated with pituitary abnormalities, cephaloceles, midline craniofacial anomalies, or rarely even tumors arising from tissue within the canal.
- •
Ecchordosis physaliphora: benign nodule of tissue in the dorsal clivus and/or prepontine cistern considered to represent ectopic notochordal remnant.
Benign clival variant of chordoma
Hyperintense on T2, but no enhancement (distinguishes from chordoma)
Often shows restricted diffusion
- •
Perineural Tumor Spread
General
- •
Spread of malignant tumor along sheath of large nerves
- •
Most commonly along CN V and VII branches
- •
Contiguous spread from the primary tumor site along nerve tracks via epineurium/perineurium distant from primary site, do not confuse with “perineural invasion” at site of primary tumor invasion on histopathology
- •
Often retrograde but can also be antegrade
- •
Important to identify for initial staging and management planning—carefully evaluate major nerve pathways according to primary tumor site
- •
Some head and neck cancer types have particularly high propensity (e.g., adenoid cystic carcinoma [ACC]) but SCC is much more common therefore overall more commonly seen with SCC; can also be seen with desmoplastic melanoma and lymphoma
- •
Subtle but may be seen on CT:
Asymmetry and soft tissue infiltration in PPF, neural foramina; widening of these structures when more advanced
- •
Contrast-enhanced high resolution MRI is the optimal technique for evaluation of perineural spread of tumor.
- •
May also see secondary findings: look for denervation changes
- •
Differential Diagnosis (DDx)
- •
Nerve sheath tumors
Tubular, fusiform, lobular mass along nerve or nerves
Typically larger than perineural tumor spread
No other primary head and neck tumor/malignancy
- •
Skull base meningioma
Homogeneously enhancing dural-based mass
May extend into neural foramina, jugular foramen, or PPF
- •
Invasive fungal sinusitis
Immunocompromised patients, including diabetics
Infiltrating disease but does not follow nerves exclusively
- •
Sarcoidosis
Nerve involvement may mimic perineural tumor spread
Absence of primary head and neck malignancy
May have other associated findings such as dural-based inflammation, leptomeningeal component
- •
Orbit
General
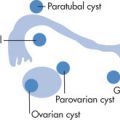
Orbital Spaces ( Figs. 7.11 – 7.12 )
- •
Intraconal space: space inside the rectus muscle pyramid

FIG. 7.11

FIG. 7.12
- •
Extraconal space: space outside the rectus muscle pyramid
- •
Preseptal space
- •
Postseptal space
- •
Lacrimal fossa
- •
Orbital Structures
- •
Globe (anterior chamber, posterior chamber, lens, vitreous, sclera/choroid/retina)
- •
Intraconal, extraconal fat
- •
Optic nerve and sheath
- •
Ophthalmic artery and vein
- •
Rectus muscles
- •
Orbital Septum
- •
Fascia arising from orbital rim periosteum
- •
Attaches to outer margins of bony orbit and deep tissues of lids
- •
Separates structures in the orbit from soft tissues in the face (postseptal vs. preseptal)
- •
Globe
Retinoblastoma
- •
Malignant tumor that arises from neuroectodermal cells of retina. Clinical: leukokoria (white mass behind pupil). Age: <3 years (70%)
- •
30% bilateral, may also be multifocal within one eye
- •
60% sporadic, 40% hereditary, 10% of patients have a positive family history
- •
Radiographic Features
- •
Intraocular mass
- •
High density (calcification, hemorrhage)
- •
Dense vitreous, common (secondary to hemorrhage)
- •
Calcifications ( Fig. 7.13 ) are common (90%); in absence of calcifications suspect other mass lesions:
Persistent hyperplastic primary vitreous (PHPV)
Retrolental fibroplasia (retinopathy of prematurity); calcium may be seen if advanced
Toxocariasis (no calcification acutely)
Coats disease

FIG. 7.13
- •
MRI findings:
T1: variable, mildly hyperintense compared with vitreous (unless hemorrhage in vitreous)
T2: hypointense relative to vitreous
T1 postcontrast: moderate to marked heterogeneous enhancement
- •
Primary role of imaging is to determine tumor spread:
Scleral breakthrough
Optic nerve extension
Intracranial spread
- •
Pearls
- •
Tumors may occur bilaterally or trilaterally (bilateral + intracranial, pineal region tumor much more common than suprasellar)
- •
Associated with other malignancies (osteosarcoma most common) later in life; also, risk of postradiation sarcoma in treatment field
- •
Melanoma
- •
Most common (75%) primary ocular malignancy in adults. Arises from pigmented choroidal layer; retinal detachment is common.
- •
Radiographic Features ( Fig. 7.14 )
- •
Thickening or irregularity of choroid (localized, polypoid, or flat)

FIG. 7.14
- •
Exophytic, biconvex mass lesion
- •
Usually unilateral, posterior location
- •
Retinal detachment, common
- •
Contrast enhancement
- •
MRI: T1W hyperintense, T2W hypointense (can vary based on pigmentation)
- •
Poor prognostic indicators:
Large tumor size
Lack of pigmentation associated with aggressiveness
Infiltration of the angles, optic nerve, sclera, ciliary body
- •
Persistent Hyperplastic Primary Vitreous (PHPV) ( Fig. 7.15 )
Caused by persistence of portions of the fetal hyaloid artery and primary vitreous in Cloquet canal. Associated with ocular dysplasias (e.g., Norrie disease = PHPV, seizures, deafness, low intelligence quotient [IQ]). Clinical findings of blindness, leukokoria, and microphthalmia. Unilateral more common. Rare.

Radiographic Features
- •
Small globe (microphthalmia)
- •
Vitreous body hyperdensity along the remnant of the hyaloid artery
- •
No calcification rare (in contrast to retinoblastoma)
- •
Complications:
Retinal detachment
Chronic retinal hemorrhage
- •
Retrolental Fibroplasia (Retinopathy of Prematurity)
Toxic retinopathy caused by oxygen treatment (e.g., for hyaline membrane disease [HMD]). A retinal vasoconstriction leads to neovascularization and fibrovascular proliferation of the posterior vitreous and retina. Typically bilateral, retinal detachment common, may have associated hemorrhage, calcification rare except in advanced stages.
Coats Disease
Primary vascular abnormality (exudative retinopathy) causing lipoprotein accumulation in retina, telangiectasia, neovascularization, and retinal detachment (pseudoglioma). Age: typically first decade, male predominance. Rare.
Radiographic Features
- •
Unilateral (90%)
- •
Retinal detachment (V-shaped contour)
- •
Dense vitreous/subretinal exudates
- •
Calcification uncommon
- •
Hyperintense (T1 and T2) proteinaceous, hemorrhagic exudate
- •
Nerve enhancement in advanced disease as a result of secondary glaucoma
- •
Drusen
Focal calcification in hyaline bodies in the optic nerve head. Usually bilateral and asymptomatic but may be associated with macular degeneration. Blurred disk margins may be mistaken for papilledema. On CT, seen as punctate hyperdensity most commonly at optic nerve head or macula.
Globe-Shape Abnormalities ( Fig. 7.16 )
- •
Coloboma: focal outpouching involving retina, choroid, iris; caused by deficient closure of fetal optic fissure; located in region of optic disc. Associated with various congenital globe, CNS, and other systemic anomalies.

FIG. 7.16
- •
Staphyloma: acquired defect of globe wall with thinning of posterior sclera-uveal rim and protrusion of choroid or sclera. On imaging, see elongated globe with focal deformity, usually posterior, but not as pronounced as coloboma.
- •
Axial myopia: anteroposterior (AP) elongation but no protrusion
- •
Buphthalmos: congenital glaucoma, anterior ocular chamber drainage problem.
- •
Enlarged globe, increased depth of anterior chamber.
- •
Leukokoria
Leukokoria refers to a white pupil. Clinical, not a radiologic, finding. Underlying causes:
- •
Retinoblastoma
- •
PHPV
- •
Congenital cataract
- •
Toxocariasis
- •
Other
Sclerosing endophthalmitis
Coats disease
Retrolental fibroplasia
Trauma
Chronic retinal detachment
- •
Retinal Detachment ( Fig. 7.17 )
Separation of the sensory retina from the outer pigmented epithelium. Appears in a characteristic V shape, with the apex of the detachment at the optic disc. The presence of retinal or choroidal detachment may be caused by an ocular mass.

Choroidal Detachment (see Fig. 7.17 )
Usually results after ocular surgery, trauma, or uveitis, causing fluid to accumulate in the choroidal space. Characteristic appearance spares the posterior third of the globe (region of the optic disc) in contradistinction with retinal detachment.
Optic Nerve
Optic Nerve Glioma
Most common cause of diffuse optic nerve enlargement, especially in childhood. Pathology: childhood lesions most commonly low grade astrocytomas (grade I pilocytic astrocytoma > grade II fibrillary astrocytoma). In patients with neurofibromatosis type 1 (NF1), pathology may be perineural arachnoid gliomatosis (PAG) rather than true astrocytoma. In adults, commonly high-grade astrocytomas. Clinical findings include loss of vision, proptosis (bulky tumors). Most common in first decade of life. In NF1 the disease may be bilateral.
Radiographic Features
- •
Types of tumor growth: tubular, excrescent, fusiform widening of optic nerve
- •
Enlargement of optical canal; >1 mm difference between left and right is abnormal.
- •
Lower CT density than meningioma
- •
Contrast enhancement variable
- •
Calcifications rare (but common in meningioma)
- •
Tumor extension best detected by MRI: chiasm → optic tracts → lateral geniculate body → optic radiation
- •
Optic Nerve Meningioma
Optic nerve sheath meningiomas arise from arachnoid rests in meninges covering the optic nerve. Age: fourth and fifth decades (female predominance in adults); younger patients typically have neurofibromatosis type 2 (NF2). Progressive loss of vision.
Radiographic Features
Mass
- •
Tubular, 65%
- •
Eccentric (exophytic), 25%
- •
Fusiform, surrounding the optic nerve, 10%
- •
Calcification (common)
- •
Enhancement
- •
Intense contrast enhancement
- •
Linear bands of enhancement (nerve within tumor): “tramtrack sign”
- •
Other
- •
Sphenoid bone and/or optical canal hyperostosis in advanced tumors
- •
Optic Neuritis
Clinical Findings
- •
Visual loss
- •
Pain on eye movement
- •
Afferent papillary defects
- •
Causes
- •
Isolated (idiopathic)
- •
Multiple sclerosis (MS)
- •
Neuromyelitis optica (Devic syndrome)
- •
Acute demyelinating encephalomyelitis (ADEM)
- •
Pediatric optic neuritis: rare, may follow viral illness or vaccination, ADEM
- •
40%–60% of patients ultimately develop MS (and 70%–90% of MS patients develop optic neuritis at some point)
- •
Radiographic Features (Acute Phase)
- •
Coronal T2W or postgadolinium T1W with fat suppression best for diagnosis
- •
T2W: obliteration of the perioptic space; increased T2 signal of the affected optic nerve
- •
Enhancement of the optic nerve
- •
Extraocular Tumors and Vascular Lesions
Vascular Lesions
Orbital cavernous venous malformation (previously/commonly known as cavernous hemangioma ): adults, not a true neoplasm, rather vascular malformation; true capsule, benign, most common vascular orbital mass in adults
- •
Most commonly in lateral intraconal space
- •
Well-defined nonaggressive mass
- •
Hyperintense on T2W images
- •
Progressive enhancement “fill-in”
- •
Orbital infantile hemangioma (capillary hemangioma): benign vascular tumor of infancy, no capsule
- •
Lobular or infiltrative hypervascular, intensely enhancing mass
- •
On T2W images: hyperintense, flow voids may be visible.
- •
Most frequently superficial extraconal location, may have postseptal extension, uncommonly presents as exclusively retrobulbar mass
- •
Grows for <1 year and then typically involutes
- •
Venous, lymphatic, or venolymphatic malformations: vascular malformation with or without lymphatic component
- •
Multiloculated, transspatial lesions
- •
Those with significant lymphatic component tend to be more cystic and have propensity to hemorrhage with fluid-fluid levels.
- •
Those with predominantly venous component tend to have more homogenous enhancement.
- •
Venous varix: distensible venous channel with systemic connection
- •
Dynamic enlargement of lesion with provocative maneuver (e.g., Valsalva)
- •
May not be visible when patient relaxed
- •
May present with thrombosis or hemorrhage
- •
Hemangiopericytoma: uncommon, slow-growing vascular neoplasm that can be benign or malignant
- •
Well-circumscribed or invasive when high grade
- •
May remodel or erode bone
- •
Avidly enhancing
- •
Flow voids common on T2W images
- •
Other vascular lesions: AVM, dural arteriovenous fistula, and cavernous carotid fistula
Dermoid Cyst
Common orbital tumor in childhood. Age: typically present in the first two decades.
Radiographic Features
- •
Low CT attenuation and T1 hyperintensity (fat) are diagnostic.
- •
Contiguous bone scalloping or sclerosis is common.
- •
May contain debris (inhomogeneous MRI signal).
- •
Calcification present occasionally.
- •
Lacrimal Gland Tumors
Lymphoid
- •
Benign reactive lymphoid hyperplasia
- •
Lymphoma
- •
Epithelial tumors
- •
Benign mixed (pleomorphic) tumor (most common epithelial tumor)
- •
ACC
- •
Mucoepidermoid CA
- •
Malignant mixed tumor (carcinoma ex pleomorphic adenoma)
- •
Rhabdomyosarcoma
Most common malignant orbital tumor in childhood. Mean age: 7 years.
Radiographic Features
- •
Large, aggressive soft tissue mass (intraconal or extraconal)
- •
Metastases to lung and cervical nodes
- •
Metastases
Adults: breast, lung, renal cell, prostate CA, melanoma. Breast metastasis to the orbit may have retractile fibrotic stroma and paradoxically be associated with enophthalmos. There can also be direct extension of malignant sinonasal tumors to the orbit. Children: rare, neuroblastoma, leukemia.
Infectious, Inflammatory, and Infiltrative Lesions
Orbital Infection
The orbital septum represents a barrier to infectious spread from anterior to posterior structures. Common causes of orbital infection include spread from infected sinus and less commonly trauma.
Radiographic Features
- •
Periorbital cellulitis: soft tissue swelling
- •
Postseptal infection (true orbital cellulitis)
Infiltration of extraconal, postseptal fat
Subperiosteal infiltrate or abscess
Lateral displacement of enlarged medial rectus muscle
Stranding of retrobulbar fat if intraconal extension
Proptosis
- •
Evaluate paranasal sinuses for potential source
- •
Bacterial infections can be complicated by cavernous sinus thrombosis.
- •
Thyroid Ophthalmopathy
Orbital pathology (cellular infiltration, deposition of glycoproteins and mucopolysaccharides in the orbit, fibrosis) caused by autoantibodies targeting thyrotropin receptors found in orbit (in addition to thyroid). Clinical: painless proptosis; patients may be euthyroid, hypothyroid, or hyperthyroid. Functional classification (clinical severity and risk):
- •
Mild: eyelid lag and retraction with proptosis in setting of active hyperthyroidism
- •
Moderate: soft tissue inflammation and intermittent myopathy; stabilizes without major sequelae
- •
Severe: rapid and fulminant, greater mass effect, severe sequelae including optic nerve compromise
- •
Treatment: prednisone → radiation therapy → surgical decompression; surgery or 131 iodine (I) for thyroid.
Radiographic Features ( Figs. 7.18 – 7.19 )
- •

FIG. 7.18

FIG. 7.19
- •
Muscle involvement
- •
Mnemonic for involvement: I’M SLow :
- •
I nferior (most common)
- •
M edial
- •
S uperior
- •
L ateral
- •
- •
Enlargement is maximal in the middle of the muscle and tapers toward the end (infiltrative, not inflammatory disease).
- •
Spares tendon insertions (although may be involved in acute phase)
- •
Often bilateral, symmetric
- •
Other
Straightened or stretched optic nerve
Expansion of orbital fat
Lacrimal gland enlargement
- •
Idiopathic Orbital Inflammation (Orbital Pseudotumor)
Inflammation of orbital soft tissues of unknown origin
Clinical Findings
- •
Painful proptosis
- •
Typically unilateral (25% bilateral)
- •
Steroid responsive
- •
Variants
- •
Tolosa-Hunt: variant extending into cavernous sinus
- •
Sclerosing orbital inflammatory pseudotumor: variant characterized by chronic progressive fibrosis
- •
Radiographic Features ( Fig. 7.20 )
- •
Infiltrating intraconal or extraconal inflammation presenting as ill-defined infiltration or less commonly as a mass

FIG. 7.20
- •
Typical features:
Unilateral
Myositic form (involves extraocular muscles) most common, followed by lacrimal gland involvement, followed by other areas of involvement
Any muscle can be affected; superior complex and medial rectus most frequent.
Muscle enlargement
Unlike thyroid ophthalmopathy, involves tendons of muscles (because it is an inflammatory disease)
Stranding of orbital fat secondary to inflammation
Diffusion weighted images may be helpful for distinguishing pseudotumor from lymphoma/malignant disease: pseudotumor generally has higher values on ADC (less restricted).
- •
| Pseudotumor | Thyroid Ophthalmopathy | |
|---|---|---|
| Involvement | Unilateral, 75% | Bilateral, 90% |
| Tendon | Involved | Spared |
| Muscle | Enlargement | Enlargement: I > M > S > L |
| Fat | Inflamed | Increased amount of fat |
| Lacrimal gland | May be inflamed | May be enlarged |
| Steroids | Good, rapid response | Less responsive, slower response |
Trauma
Types:
- •
Blunt trauma with orbital blow-out fractures
- •
Penetrating injury
- •
Detection of ocular foreign bodies:
- •
CT > plain radiography
Metal: CT has 100% sensitivity for objects >0.06 mm 3
Glass: depends on type of glass, overall high sensitivity of CT for denser glass types >1.5 mm 3
Wood: difficult to detect because wood density is similar to that of soft tissue
- •
On CT, wood appears as air density with geographic margin, dry wood much lower attenuation than fresh wood
- •
- •
Other
Erdheim-Chester Disease
Lipid granulomatosis (non-Langerhans histiocytosis) with retroorbital deposition or mass, xanthelasma of eyelids, skeletal manifestations (medullary sclerosis, cortical thickening), and cardiopulmonary manifestations as a result of cholesterol emboli. Rare. Diffuse infiltrative mass most commonly involving intraconal space or other area in orbit, bilateral.
Ocular Manifestations of Phakomatoses
NF1
- •
Lisch nodules
- •
Optic pathway glioma
- •
Optic nerve sheath ectasia
- •
Sphenoid bone dysplasia
- •
Choroidal hamartoma
- •
Plexiform neurofibroma
- •
NF2 (orbital involvement rare)
- •
Meningioma
- •
Schwannoma
- •
Sturge-Weber (encephalotrigeminal angiomatosis)
- •
Choroidal angioma
- •
Buphthalmos
- •
Glaucoma
- •
Abnormal ocular enhancement on MRI, thickest over posterior portion of the globe
- •
Tuberous sclerosis
- •
Retinal hamartomas
- •
Punched out areas of retinal depigmentation
- •
Angiofibromas of the eyelids
- •
Colobomas.
- •
Von Hippel-Lindau (VHL)
- •
Retinal hemangioblastomas
- •
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree