, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
According to statistics, every year more than 35,000 cases of planocellular cancer of the head and neck are registered (Forastiere et al. 2001). Head and neck cancers make up about 5% of the total number of tumors, planocellular cancer being the widest-spread histological subtype. Smoking and other ways of consuming tobacco as well as alcohol consumption increase the risk of developing this kind of cancer. Planocellular cancer of the head and neck (PCHN) has specific development stages for every anatomic region in the larynx, buccal cavity, oropharynx, hypopharynx, nasopharynx and paranasal sinuses. More than 50% cases of this kind of cancer appear in the oropharynx, especially on the palatine tonsils and at the base of tongue. Currently about 60% PCHN patients have developed local manifestations and undergo treatment with surgical intervention, radiotherapy, chemotherapy or a combination of these kinds of treatment (Forastiere and Urba 1995; Forastiere 1994).
3.1 Planocellular Cancer of the Head and Neck
According to statistics, every year more than 35,000 cases of planocellular cancer of the head and neck are registered (Forastiere et al. 2001). Head and neck cancers make up about 5% of the total number of tumors, planocellular cancer being the widest-spread histological subtype. Smoking and other ways of consuming tobacco as well as alcohol consumption increase the risk of developing this kind of cancer. Planocellular cancer of the head and neck (PCHN) has specific development stages for every anatomic region in the larynx, buccal cavity, oropharynx, hypopharynx, nasopharynx and paranasal sinuses. More than 50% cases of this kind of cancer appear in the oropharynx, especially on the palatine tonsils and at the base of tongue. Currently about 60% PCHN patients have developed local manifestations and undergo treatment with surgical intervention, radiotherapy, chemotherapy or a combination of these kinds of treatment (Forastiere and Urba 1995; Forastiere 1994).
In patients with head and neck tumors 5-year survivability reaches 60% in absence of metastases, in case of metastatic lesion it is 30%. Five-year survivability for patients with locoregional tumor dissemination undetected when making diagnosis amounts to 30% for all cases of neck and head cancer. In order to make a decision on the choice of treatment or/and to determine long-term prognosis, the correct and timely staging of primary tumors is needed (Bhattacharyya et al 2005).
Staging of head and neck cancer (HNC) is done according to clinical signs and is specific for each affected region of the head or neck. The clinical approach to staging is based on the most precise assessment of the disease dissemination before treatment. For all the regions of the head and neck, except for the thyroid gland, a common classification system of regional lymph nodes is used (Table 3.1).
Table 3.1
Classification of regional lymph nodes
NX | Regional lymph nodes are unassessable/were not assessed |
NO | No metastases to regional lymph nodes |
N1 | Tumor dissemination to one lymph node with diameter less than 3 cm on the side of lesion |
N2 | (a) Tumor dissemination to one lymph node with diameter more than 3 cm but less than 6 cm on the side of lesion |
(b) Tumor dissemination to several lymph nodes with diameter less than 6 cm on the side of lesion | |
(c) Tumor dissemination to one or several lymph nodes with diameter less than 6 cm on both sides of the neck or on the contralateral side | |
N3 | Tumor dissemination to lymph nodes with diameter more than 6 cm |
Diagnosis of the primary tumor is mainly based on visual examination, palpation and endoscopy in less accessible areas such as the larynx. Corresponding regions of lymphatic drainage are subjected to careful palpation. Besides that, information is used in HNC staging obtained by imaging methods (MRI, CT) and necessary for detecting and localizing head and neck tumors as well as for differentiating lymph nodes from surrounding soft tissues and blood vessels and determining the dimensions, structure and contours of solid mass (structural tomographic visualization). However, none of these technologies permits the detection of persistent or recurrent cancer (Stern et al. 1990).
Precise initial assessment of the primary tumor and of the state of lymph nodes is crucial. Early detection of relapsing neck and head cancer with subsequent adequate treatment may induce a decrease in volume of surgical intervention and help prevent disability as well as achieve the optimum clinical outcome. Until recently, such a possibility was based only on the combination of clinical assessment and anatomic visualization (CT or MRI). At present, besides clinical and radiologic methods, PET technology is used as well. Its role in staging and observation of neck-and-head cancer patients keeps growing (Reske, Kotzerke 2001).
3.1.1 Clinical Use of PET and PET-CT in Head and Neck Cancers
18F-FDG PET has a number of clinical advantages over CT and MRI as far as PCHN diagnosis is concerned.
Diagnosis of Primary Tumors
The diagnosis of the primary tumor and assessment of its dissemination to adjacent tissues and structures constitute an important clinical task. This problem is solved by means of physical examination and standard anatomic visualization with use of CT and MRI, which are quite sensitive when detecting primary tumors (67–88%), even though they are less specific (50–75%). 18F-FDG PET has roughly the same sensitivity (71–95%) but its specificity is higher (67–100%) (Stokkel et al. 1998).
Assessment of the State of Regional Lymph Nodes
Tumor affection of lymph nodes has a negative impact on survivability. In the case of their metastatic affection it is necessary to change the tactics of treatment. The percentage of false-negative results in palpation reaches 5–44%, and false-positive results make up 13–25% (Ali et al. 1985). When detecting the infiltration of lymph nodes, the conventional visualization is characterized by a high variability of the levels of sensitivity (from 36 to 95%) and of specificity (from 58% to 97%) (Braams et al. 1995). When CT or MRI is used, diagnosis of affected lymph nodes is based on measuring their dimensions. The point of reference is the upper limit for unaffected nodes which is 1.0–1.5 cm. In this way benign and malignant alterations are differentiated. This approach has its shortcomings. For example, lymph nodes significantly enlarged in diameter and nodes with complex structure may reflect a reaction to processes of non-tumorous nature (inflammation), whereas small lymph nodes may well contain tumor cells. It has been proved that more than 40% metastases are situated in lymph nodes whose size is below 1 cm. When using routine methods of visualization (MRI, CT and US) they are often overlooked.
Since PET is a metabolic tool, it permits the detection of lesions in small nodes and lesions in enlarged nodes with the additional option of quantification by means of SUV. The SUV level seems to be a predictive factor for overall survival as first study reports implicate (Kubicek 2010). Basing on available data, 18F-FDG PET can be stated to significantly exceed in sensitivity (70–100%) and in specificity (84–100%) the standard methods of radiological visualization (MRI, CT, US) as regards diagnosing metastases to lymph nodes.
Primary Tumor of Unknown Localization
Diagnosis of latent primary tumor is made only if the primary tumor is not found by careful complex patient examination and is not detected in the therapy process. In head and neck cancer, malignant affection of lymph nodes in the absence of the primary focus of the disease is observed only in 2% of cases. However, all of these cases present an important aspect in treating tumors of this localization. The rate of 3-year survivability without relapses after surgical intervention and/or radiotherapy with unknown primary focus ranges from 40% to 50% for patients in stage N1, to 38% in stage N2 and to 26% in stage N3. For patients in whom primary tumors are subsequently detected the survivability rate is lower than for patients with primary focus remaining unknown. High sensitivity of PET makes this method inestimable for examining these kinds of patients. It has been established that PET permits detection of the tumor focus for the first time in 40–60% of cases (Fig. 3.1) (Jungehulsing et al. 2000; Kole et al. 1998).
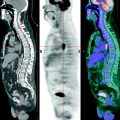
Fig. 3.1
(a–c) 18F-FDG PET-CT. Primary tumor at the base of the tongue on the left. Neck lymphadenopathy. Histological examination of an enlarged neck lymph node detected its lesion by metastases of planocellular cancer. (a) Fused 18F-FDG PET-CT image (coronary cut). (b) CT image (axial cut). (c) Fused 18F-FDG PET-CT image (axial cut). 18F-FDG PET-CT (c) detected a focus of hypermetabolism of glucose in the tongue base, SUV = 6.6. PET-CT data are estimated as indication of tumor lesion. Other metastases were not detected
Unfortunately, in spite of progressing development of radiotherapy and chemotherapy and of surgical treatment, the rate of survivability of patients with planocellular cancer of the head and neck has not improved over the last two decades (Vokes et al. 1993). One of the negative factors having a significant impact on the level of survivability of PCHN patients is the development of primary multiple tumor lesion in the area of the head and neck. The risk of occurrence of a second primary tumor for patients recovered from PCHN is 30% and more during the rest of their life. In 10% patients with primary PCHN, a second synchronous tumor in the area of the head and neck may be detected. The detection of these tumors as well as that of metastases plays an important part in further therapy (Wax et al. 2002).
The advantage of 18F-FDG PET over other methods is the possibility of whole-body scanning, which is impracticable or inefficient when using other visualization methods. Whole-body examination by means of 18F-FDG PET permits the detection of a second parallel tumor and metastases to other organs. Stokkel et al. (1998) reported that 18F-FDG PET permitted the detection of a second parallel tumor in 17.6% of cases of primary head and neck cancer that had been overlooked in clinical and tomographic examination. Goerres et al. (2003) noted that in 14.4% of cases of planocellular cancer of the buccal cavity PET results had an impact on the schedule of therapeutic steps.
Treatment Efficiency Control and Relapses
Patient examination after HNC treatment is more complex than the one before treatment. The medical treatment, be it surgical intervention, radiotherapy or chemotherapy, may lead to the alteration of anatomic structures of the affected region. In order to identify a relapse, post-therapy changes and cicatrices, surgical biopsy is often needed. However, biopsy in the region subjected to treatment is invasive and may induce complications. As for metabolic PET visualization, it permits to differentiate with high precision post therapy alterations and relapsing cancer. Collins with coauthors have shown that combined use of fine needle biopsy and 18F-FDG PET helps reach 94% sensitivity in detecting relapsing head and neck cancer (Collins et al. 1998). Other research shows that using 18F-FDG PET alone in detecting relapsing head and neck cancer yields more than 90% sensitivity (Zhuang et al. 2004).
Additional Capacities of PET-CT
In spite of its high sensitivity PET suffers from insufficient accuracy in determining the anatomic localization of radiopharmaceutical (RP) uptake foci. 18F-FDG is accumulated, besides in tumors, also in the muscles and in areas of inflammatory changes as well as in some metabolically active organs (palatine tonsils and salivary glands). Therefore PET may give inaccurate information on the precise site of pathological uptake foci. In the head and neck area such inaccuracy may provoke the wrong detection of tumor at the base of the tongue and adjacent tonsillar mass or hyperchordal affection of the larynx and of the vocal chords. The limitations of using each of the visualization methods (CT or PET) can be overcome if they are used in combination. Anatomic high-resolution information provided by CT completes data on tissue characteristics obtained by means of PET. PET-CT data co-registration unites functional and anatomic kinds of visualization into one whole, both information sources being equally important. Such a result is achieved owing to the combination of data of different modalities, integration of separate PET and CT visualization results into one whole by means of their fusion.
PET-CT apparatuses permit additional data to be obtained on the staging and restaging of cancer, prognosis of clinical course and treatment efficiency assessment (Fig. 3.2). The advantages of PET-CT include a more accurate localization of foci by means of anatomic-functional registration approaching the ideal with fewer motor artifacts, better differentiation between physiologic and pathologic uptake, and shorter duration of scanning due to CT data for attenuation correction (Schoeder 2004). The latter circumstance contributes to the patient’s comfort and helps solve the problem of claustrophobia.
Fig. 3.2
18F-FDG PET-CT in planocellular head and neck cancer. Carcinoma of the palatine tonsil on the left. (a) Asymmetry of anatomic structures observed in CT – a displacement to the right due to a volumetric formation in the projection of a palatine tonsil. (b) 18F-FDG PET detects a focus of hypermetabolism of glucose in the area of the soft palate on the right (SUV = 6.6). (c) In a coregistred PET-CT image there is a coincidence of the focus of metabolism and volumetric formation. After surgical and radiological treatment relatively lowered RP uptake in the area of cicatricial alterations is determined. In CT (d) and 18F-FDG PET (e) images on the same level, restoration of anatomic geometry of the oropharynx and a 2.7-times SUV decrease are detected. (f) In a fused 18F-FDG PET/CT image the focus of hypermetabolism of glucose partially coincides with the area of perifocal oedema and inflammatory infiltration
So, diagnosis and posterior observation in planocellular carcinoma of the head and neck are usually based on clinical examination and anatomic visualization by means of CT or MRI with contrast enhancement. Yet, as useful as these methods are for assessment of suspicious regions, they do not always permit the detection of differences between residual and relapsing tumor as well as those between inflammatory and post therapy alterations. It has been proved that 18F-FDG PET may be successfully used for detection and staging of the primary or recurrent planocellular cancer of the head and neck. PET also has shown its efficiency in diagnosing primary tumor foci of unknown localization and in controlling subsequent surgical and other treatments of HNC. The introduction into clinical practice of combined PET-CT scanners has increased the information value of visualization methods for clinicians engaged in treatment of the head and neck cancers.
3.2 Thyroid Cancer
Clinically detected carcinoma of the thyroid gland makes up only 1% of all the cases of malignant tumors. Its annual primary diagnosis in different regions of the globe ranges from 0.5 to 10 cases per 100,000 of the population. In spite of the fact that this pathology is not so frequent, thyroid carcinoma rivals in prevalence with multiple myeloma, it occurs twice as often as Hodgkin’s lymphoma and is comparable in frequency with tumors of the esophagus, larynx, buccal cavity and neck of uterus. Moreover, this is the most frequent endocrine malignant formation which causes more deaths than all the rest of endocrine cancers taken together (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001).
According to the American Cancer Society, in 2003 up to 22,000 new cases of thyroid cancer (TC) were detected in the USA, which made up 90% of all endocrine cancers. TC is more frequently found in women than in men, the ratio being 3.2:1. A permanent increase in number of new TC cases has been observed (Jemal et al. 2007). Survivability is rather high with adequate treatment. The estimated number of people who survived more than 40 years after the diagnosis is 190,000 (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001). Thyroid carcinoma usually originates from follicular cells, but one rare kind of medullary carcinoma develops from parafollicular or C-cells. We know four histological types of thyroid cancer originating from follicular cells (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001). The most frequent of them is papillary cancer (80%). Follicular cancer makes up 10% of cases. B-cell, oncocytic tumors and anaplastic cancer make up 5% each. Papillary and follicular carcinomas are usually considered to belong to differentiated thyroid cancers. A typical papillary carcinoma is a unilateral focus in the thyroid gland. As a rule, in this form regional lymphatic dissemination is observed. Metastases to lymph nodes detected in the primary diagnosis increase the risk of a subsequent relapse.
Follicular carcinoma is another frequent kind of thyroid cancer; usually it consists of nodes which do not transcend the boundaries of the gland capsule. It rarely disseminates to lymph nodes, but it can bring about deposits to lungs and bones due to hematogenous metastasis. B-cell carcinoma is considered as a subtype of follicular thyroid cancer and has a similar course. Anaplastic carcinoma, sometimes called undifferentiated thyroid cancer, is a rare form which is believed to develop in consequence of existing papillary or follicular cancer being transformed. Its course is very aggressive and rapid with distant metastases, and it often results in a lethal outcome. Medullar thyroid cancer cells, unlike those of papillary and follicular cancers, do not secrete thyroid hormones, this form of cancer being associated with hyper-production of calcitonin and carcino-embryonic antigen (American Cancer Society-Thyroid Cancer 2007).
On the whole, in the case of differentiated thyroid cancer patients with small tumors (<2 cm), women, in the absence of both local dissemination and distant metastases, have a good prognosis with low risk of relapses and lethal outcomes. Metastasis to lymph nodes of the neck as an independent prognostic factor can be associated with a high frequency of relapses, and bilateral affection of the neck or involvement of the mediastinum have an impact on bad general prognosis (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001).
Most patients with thyroid cancer have a palpable solid mass in the area of the neck, which can represent both the primary tumor in the gland itself and a metastatic regional lymphadenopathy. However, in some patients the tumor may not have clinical manifestations, and the non-palpable focus is first detected either during examination with high-resolution visualization methods or during a surgical operation on a benign disease of the thyroid gland. Family anamnesis of medullar thyroid cancer or of the syndrome of multiple endocrine neoplasia of the second type, detection of a RET-oncogene mutation, of high level of calcitonin or both can induce implementation of a prophylactic thyroidectomy in patients with high risk of early medullar thyroid cancer, which will be detected only by a histological examination (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001).
Thyroid cancer diagnosis requires a morphological confirmation when examining both cytologic and histologic materials. Fine-needle aspiration biopsy is the most efficient available method of differential diagnosis of thyroid nodes and of assessment of the degree of malignancy. Nevertheless, in each particular case diagnosis should be verified by the histological examination of the operation material.
Differentiated thyroid cancer is considered to be rather curable, because after an efficient surgical resection of the primary tumor with subsequent ablative therapy with radioactive iodine it is possible to apply control of the thyroglobulin rate of blood serum as an extremely sensitive method of relapse detection.
Most thyroid cancer patients first undergo surgical treatment. The goal of the first stage is an adequate excision of the primary tumor and of any foci of locoregional dissemination. Due to high risk of relapses after unilateral hemithyroidectomy as well as to that of hypoparathyreosis after total strumectomy, subtotal thyroidectomy is initially implemented. Almost all patients receive everyday substitutive hormonotherapy. For cancers deriving from follicular cells, this kind of therapy is based on taking peroral supraphysiological doses of levothyroxin for the purpose of complete suppression of secretion of the pituitary thyroid-stimulating hormone (TSH) down to its basal level in blood serum <0.1 IU/L. This implies that the suppression of TSH secretion by hypothesis oppresses TSH-dependent growth of cells of differentiated follicular cancers (AACE Clinical Practice Guidelines for the Management of Thyroid Carcinoma 2001).
The second most frequently used kind of post-operation therapy for follicular cancer patients is radioablation using an isotope of iodine. This kind of therapy has three main tasks:
To destroy occult micro-accumulations of carcinoma cells in the residual tissue of the thyroid gland as well as to destroy distant metastatic lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree