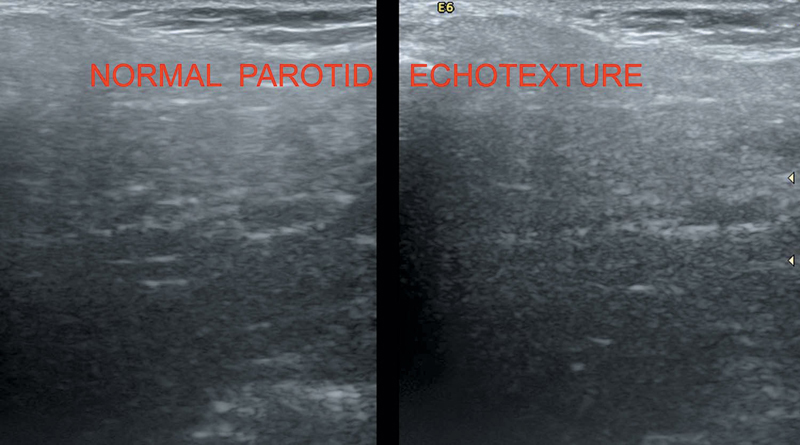
Normal parotid gland (Figure 37.1) has homogenously hyperechoic echotexture (because of high fat content) in the retromandibular fossa. Small intraparotid lymph nodes are noted. Stenson’s duct is the main duct. Retromandibular vein and facial nerve differentiates between the superficial and deep part of the parotid gland.
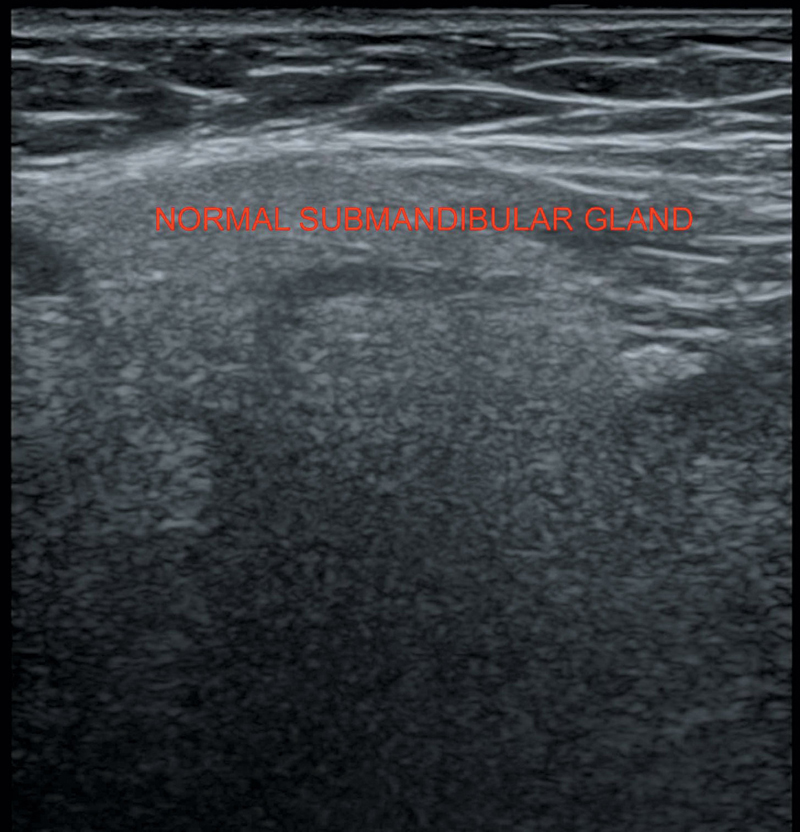
Submandibular gland is homogeneous hyperechoic structure at the posterior border of mylohyoid muscle (Figure 37.2). Wharton’s duct is its main duct. Facial artery and vein lie posterior to the gland.
Sublingual gland lies deep to the mylohyoid.
Level 1 a—Submental nodes
Level 1 b—Submandibular nodes
Internal jugular (deep cervical) chain—Levels 2, 3, and 4
Level 2—(Upper cervical) from the base of skull to the hyoid bone
Around internal jugular vein
Level 3—(Midcervical) from lower border of hyoid to the lower cricoid border
Lateral to internal jugular vein/common carotid artery
Level 4—(Lower cervical) from cricoid to clavicle
Level 5—Posterior triangle/spinal accessory nodes
Level 6—Anterior to visceral space usually prelaryngeal/pretracheal nodes
Level 7—Superior mediastinal nodes
Figure 37.1 Illustrating normal parotid gland echo pattern.
Figure 37.2 Demonstrating normal echo pattern of submandibular gland.
Explained in detail in the next paragraph.
Usually not visualized routinely due to its small size and deep location.
Supine with neck in extension. Pillow may be placed for the support beneath the shoulder. Both transverse and longitudinal planes are scanned with 7.5–10 MHz linear transducer. Color Doppler and spectral waveform too are helpful.
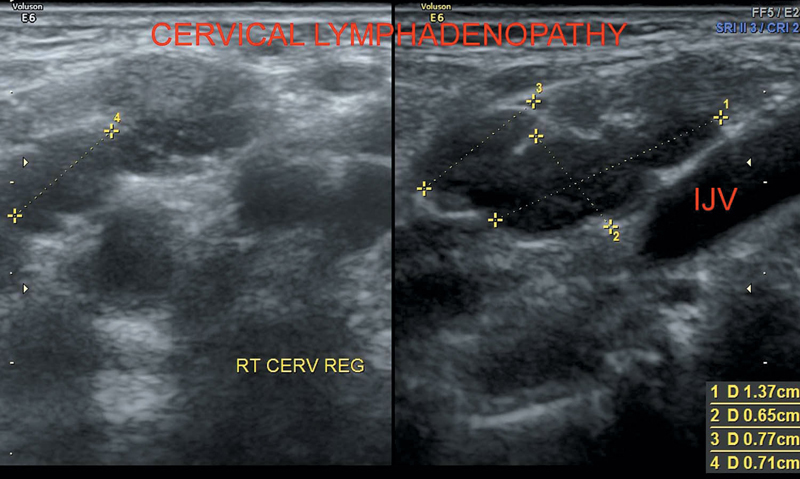
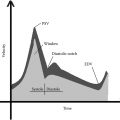
Metastasis in cervical lymph nodes is common in head and neck cancers, lymphoma, inflammatory and infective (tuberculosis) lesions. Evaluation of lymphadenopathy helps in the assessment of prognosis and monitoring response to treatment (Figure 37.3).
Benign nodes
Usually oval in shape (long axis/short axis L/S >1.5–2)
Iso to hyperechoic in echotexture
Echogenic hilum is seen suggestive of preserved sinusoidal architecture
Central hilar flow pattern
Malignant nodes
Usually round in shape (long axis/short axis L/S <2 or 1.5)
Hypoechoic with pseudocystic/necrotic areas
Absence of hilum
Disorganized peripheral flow pattern
Metastatic nodes from papillary thyroid carcinoma may show punctuate calcification.
Figure 37.3 Depicting abnormal cervical lymph nodes.
Thin-walled, round/oval anechoic lesion usually seen anterolateral to common carotid artery bifurcation. May show echoes or septae, if infected/hemorrhagic.
Thin-walled, round/oval anechoic lesion usually seen anteriorly above the thyroid cartilage in the midline.
Multiseptated, compressible, thin-walled cystic lesion usually located in the posterior triangle of the neck.
Thin-walled cystic lesion in the sublingual space; can be imaged both from the skin and transorally with a small probe. Contents become echogenic with thick walls if it gets infected.
If simple ranula extends into the submandibular space, it is known as the plunging ranula.
Well-defined anechoic lesions (with posterior acoustic enhancement) in the submandibular or sublingual space. It may be homogeneous with low-level echoes or heterogeneous due to presence of fat globules.
Well-defined, compressible avascular hypoechoic mass with linear echogenic streaks parallel to the transducer.
Schwannoma and neurofibromas.
Involve vagus nerve, cervical nerve roots, sympathetic chain, and brachial plexus.
Well-defined heterogeneous, hypervascular mass in continuity with the thickened nerve.
Parotid gland—Pleomorphic adenoma is the most common benign tumor involving the parotid gland.
Warthin’s tumor (adenolymphoma) is the second most common tumor of parotids, usually bilateral with multiple cysts.
Mucoepidermod carcinoma is the malignant variety.
Abscesses—Irregular, heterogeneous lesion with necrotic areas and hypervascularity.
Sialedenitis with/without sialoliths.
More common in submandibular gland. Inflammation of the gland presenting as enlarged gland with heterogeneous echotexture and high vascularity.
Sialolith (echogenic calculus with acoustic shadowing) sometimes may be seen in the dilated duct.
Acute parotitis
Viral/bacterial
Heterogeneous hypoechoic echotexture of the gland with increased vascularity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree